Abstract
Recent genetic sequencing studies in large series’ of predominantly childhood medulloblastoma have implicated loss-of-function, predominantly truncating, variants in the ELP1 and GPR161 genes in causation of the MBSHH subtype specifically. The latter association, along with a report of an index case with some features of Gorlin syndrome has led to speculation that GPR161 may also cause Gorlin syndrome. We show that these genes are associated with relatively low absolute risks of medulloblastoma from extrapolating lifetime risks in the general population and odds ratios from the population database gnomAD. The projected risks are around 1 in 270–430 for ELP1 and 1 in 1600–2500 for GPR161. These risks do not suggest the need for MRI screening in infants with ELP1 or GPR161 variants as this is not currently recommended for PTCH1 where the risks are equivalent or higher. We also screened 27 PTCH1/SUFU pathogenic variant-negative patients with Gorlin syndrome for GPR161 and found no suspicious variants. Given the population frequencies of 0.0962% for GPR161 and 0.0687% for ELP1, neither of these genes can be a cause of Gorlin syndrome with an unexplained population frequency far lower at 0.0021%.
Similar content being viewed by others
Short report
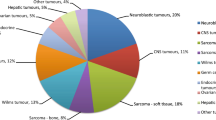
Medulloblastoma is a relatively rare malignant brain tumour that has a main peak of incidence in early childhood and infancy [1, 2]. The main syndromic predisposition to medulloblastoma is Gorlin syndrome which is characterised by multiple skin basal cell carcinoma, macrocephaly and jaw cysts with two proven gene associations (PTCH1 and SUFU) accounting for ~ 70% of cases [3]. Recent genetic sequencing studies in large series of predominantly childhood medulloblastoma have implicated loss-of-function, predominantly truncating, variants in the ELP1 (mean age of onset = 6.5years accounts for 3.2% of cases) and GPR161 (mean age of onset = 1.5years; accounts for 0.38% of cases) genes[4,5-Table 1] in causation of the MBSHH subtype specifically. The latter association, along with a report of an index case with some features of Gorlin syndrome (basal cell carcinomas, frontal bossing and a meningioma, but microcephaly instead of macrocephaly), has led to speculation that GPR161 may also cause Gorlin syndrome [5].
As reported in both papers [4, 5], the frequency of presumed loss-of-function variants in the population database gnomAD (https://gnomad.broadinstitute.org/) is high for a rare condition with both reports showing incidence above the rare disease threshold of 1 in 2,000-(Table 1). Neither paper attempted to assess the overall likelihood of a child with either an ELP1 or GPR161 loss-of-function variants developing medulloblastoma. In view of the likelihood that these genes will be added to multi-gene panels for childhood malignancy and possibly for Gorlin syndrome assessment, we have assessed the overall likelihood of medulloblastoma with each gene and specifically tested for GPR161 variants in our currently unexplained Gorlin syndrome families.
Methods
The population likelihood of medulloblastoma was assessed using data sources on annual rates of childhood medulloblastoma [1, 2] and number of children in the UK and USA. Relative risk of medulloblastoma was assessed from presumed loss-of-function variants for each gene in the published medulloblastoma series divided by the frequency in gnomAD as previously described [3].
We also sequenced the GPR161 gene (NM_001375883.1) in 27 people with Gorlin syndrome who had previously been screened for variants in PTCH1 and SUFU and in whom no causative variant had been found.
Results
Table 1 shows the results of our analysis on likelihood of childhood medulloblastoma assuming 16 years of risk in childhood. The likelihood varied from 1 to 9,000 in the USA to 1 in 14,000 in the UK. We took the derived gnomAD population data from the ELP1 paper for loss-of-function variants showing a very high population frequency of close to 1 in 1000-(Table). Thus, despite a 3.2% frequency of ELP1 loss-of-function variants in medulloblastoma, this only resulted in a relative risk of 33.5 and a childhood risk of 1/ 270-1/430 for medulloblastoma-(Table 1-row 13). For GPR161 we found 86 loss-of-function variants, including canonical splicing variants, in an average of 125,153 individuals in gnomAD. We excluded the putative missense variant in GPR161 and the index case leaving only 4 definite loss-of-function variants amongst 1040 cases. This resulted in a relative risk of only 5.6-fold and childhood risk of 1 in 1600–2500 in the USA/UK. We did not assess the likelihood for the MBSHH subtype separately. However, as all but one of the cases was in the MBSHH subtype and the frequency in non SHH pathway medulloblastoma for ELP1 was only 1/542 (0.18%), similar to the 0.1% frequency in controls, we have assumed that all of the risk related to the MBSHH subtype.
Our specific screen of GPR161 in our cohort of 27 PTCH1/SUFU pathogenic variant-negative patients with Gorlin syndrome found no pathogenic or likely pathogenic variants.
Discussion
It is likely parents of children are already receiving results indicating that their child has loss-of-function variant in ELP1 or GPR161. Indeed, in England neonates can now undergo genome sequencing at birth without any obvious symptoms and parents could receive results for an incidental pathogenic variant in ELP1 or GPR161 as genes associated with childhood malignancy. The present study will provide counsellors with sufficient risk information to provide an accurate risk assessment and recommendations. For instance, parents of neonates with a GPR161 variant can be reassured that absolute risks of medulloblastoma are very small and the increased risk may disappear after age 4 years (this will be reassuring if results are given for a 5year old) similar to SUFU and PTCH1 [3, 5, 6]. Whereas, parents of neonates with an ELP1 loss-of-function variant can be told the risks are higher but not sufficient for MRI screening [3, 6] and that the increased risk lasts well beyond 7years of age. The risks for siblings of medulloblastoma cases who are heterozygotes may still justify closer monitoring especially for ELP1 as the family may carry additional genetic factors that predispose to medulloblastoma. Without this granular information on the true implications of this finding these parents may become distressed and concerned about the requirements for clinical screening. The implied likelihood of developing medulloblastoma for both ELP1 and particularly GPR161 are overall quite low and at or well below that of PTCH1 for which no screening in childhood for medulloblastoma is recommended [3, 6]. The suggestive features for a possible diagnosis of Gorlin syndrome in the index GPR161 patient was not backed up by information on the father, brother and two nephews who were also heterozygous [2]. The population frequency of both ELP1 and GPR161 of close to 1 in 1,000 are also far too high to account for the small amount of missing heritability in a condition with a birth incidence of only 1 in 14,500 [7, 8]. We did not identify GPR161 in 27 PTCH1/SUFU negative Gorlin syndrome families which represent all the 27/86-(31.4%) unexplained by known genes (59 were due to PTCH1/SUFU) meaning an unexplained population frequency far lower at 0.0021% (1 in 46,400). Given the absence of clinical data and the even higher population frequency of ELP1 we have not assessed this gene in our Gorlin population. ELP1 and GPR161 therefore join PTCH2 as potential candidate genes for Gorlin syndrome that can be dismissed on their population frequencies and, for PTCH2 and GPR161, their absence in Gorlin syndrome kindreds [8].
We do not have an explanation for the apparent higher incidence of childhood medulloblastoma in the USA compared to the UK and this seems unlikely to be linked to an increased frequency of the known predisposition genes.
In examining gnomAD, we found a ClinVar entry for a putative likely pathogenic GPR161 missense variant, c.56T > A,p.Leu19Gln;NM_001267609;chr1:g.168,074,093 A > T[hg19] (this variant is annotated as c.-5T > A; 5’-UTR in the MANE select transcript:NM_001375883.1). The variant had been reported in homozygous form in a Turkish family as causing Pituitary Stalk Interruption Syndrome [9]. Although this quite clear syndromic diagnosis tracked with zygosity in a consanguineous kindred (the unaffected heterozygote parents had 4 further unaffected children who were not homozygous) no population frequency for this variant was supplied. We have now assessed this in gnomAD and found that it is present 18 times in South Asians in homozygous form in 15,296 individuals (1 in 850 individuals) with a further 641 being heterozygote (1 in 24). This clearly cannot be a loss-of-function variant that could cause a medulloblastoma risk (particularly as homozygous) or this would mean a much higher likelihood of medulloblastoma in South Asia and the homozygote frequency is far too high to be associated with such a rare (estimated 0.5 per million) complex condition as Pituitary Stalk Interruption Syndrome [10].
In conclusion, the absolute risk of developing childhood medulloblastoma with ELP1 and GPR161 appears low and families can be reassured particularly if these genes are found incidentally on panels. There is still a need to identify and follow patients with medulloblastoma in order to better analyse the clinical features, outcome and risk of second malignancies associated with these variants Radiological screening for medulloblastoma appears not to be justified in incidentally identified cases but the risks for siblings of medulloblastoma cases who are heterozygotes may still justify closer monitoring. ELP1 and GPR161 can be dismissed as candidates for Gorlin syndrome and it now also seems unlikely that GPR161 homozygotes have Pituitary Stalk Interruption Syndrome.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
https://www.cancerresearchuk.org/about-cancer/childrens-cancer/brain-tumours/types/medulloblastoma
https://www.cancer.net/cancer-types/medulloblastoma-childhood/statistics#:~:text=About%2020%25%20of%20childhood%20brain,ages%20of%205%20and%209
Guerrini-Rousseau L, Smith MJ, Kratz CP et al (2021) Current recommendations for cancer surveillance in Gorlin syndrome: a report from the SIOPE host genome working group (SIOPE HGWG). Fam Cancer 20(4):317–325. https://doi.org/10.1007/s10689-021-00247-z
Waszak SM, Robinson GW, Gudenas BL et al (2020) Germline elongator mutations in Sonic hedgehog medulloblastoma. Nature 580(7803):396–401. https://doi.org/10.1038/s41586-020-2164-5
Begemann M, Waszak SM, Robinson GW et al (2020) Germline GPR161 mutations predispose to Pediatric Medulloblastoma. J Clin Oncol 38(1):43–50. https://doi.org/10.1200/JCO.19.00577Epub 2019 Oct 14
Foulkes WD, Kamihara J, Evans DGR et al (2017) Cancer Surveillance in Gorlin Syndrome and Rhabdoid Tumor Predisposition Syndrome. Clin Cancer Res 23(12):e62–e67. https://doi.org/10.1158/1078-0432.CCR-17-0595
Evans DG, Howard E, Giblin C et al (2010) Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet A 152A(2):327–332. https://doi.org/10.1002/ajmg.a.33139
Smith MJ, Evans DG (2022) PTCH2 is not a strong candidate gene for gorlin syndrome predisposition. Fam Cancer 21(3):343–346. https://doi.org/10.1007/s10689-021-00269-7
Karaca E, Buyukkaya R, Pehlivan D et al (2015) Whole-exome sequencing identifies homozygous GPR161 mutation in a family with pituitary stalk interruption syndrome. J Clin Endocrinol Metab 100(1):E140–E147. https://doi.org/10.1210/jc.2014-1984
Guo Q, Yang Y, Mu Y et al (2013) : Pituitary stalk interruption syndrome in Chinese people: clinical characteristic analysis of 55 cases. PLoS One. 8: e53579-10.1371/journal.pone.0053579
Acknowledgements
This research was supported by the Manchester National Institute for Health Research (NIHR) Biomedical Research Centre (IS-BRC-1215-20007).
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: D.G.E Formal analysis D.G.E., M.J.S. Funding acquisition: D.G.E., M.J.S. Writing – original draft: D.G.E Writing – review & editing: all.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Ethical declaration
Ethical approval for the use of anonymised samples from the Manchester Centre for Genomic Medicine archive was obtained from the North West – Greater Manchester Central Research Ethics Committee (reference 10/H1008/74).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smith, M.J., Woodward, E.R. & Evans, D.G. Perspectives on the implications of carrying putative pathogenic variants in the medulloblastoma predisposition genes ELP1 and GPR161. Familial Cancer 22, 341–344 (2023). https://doi.org/10.1007/s10689-023-00330-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-023-00330-7