Abstract
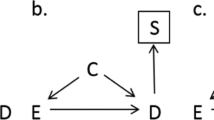
Misconceptions about the impact of case–control matching remain common. We discuss several subtle problems associated with matched case–control studies that do not arise or are minor in matched cohort studies: (1) matching, even for non-confounders, can create selection bias; (2) matching distorts dose–response relations between matching variables and the outcome; (3) unbiased estimation requires accounting for the actual matching protocol as well as for any residual confounding effects; (4) for efficiency, identically matched groups should be collapsed; (5) matching may harm precision and power; (6) matched analyses may suffer from sparse-data bias, even when using basic sparse-data methods. These problems support advice to limit case–control matching to a few strong well-measured confounders, which would devolve to no matching if no such confounders are measured. On the positive side, odds ratio modification by matched variables can be assessed in matched case–control studies without further data, and when one knows either the distribution of the matching factors or their relation to the outcome in the source population, one can estimate and study patterns in absolute rates. Throughout, we emphasize distinctions from the more intuitive impacts of cohort matching.


Similar content being viewed by others
References
Rothman KJ, Greenland S, Lash TL. Design strategies to improve study accuracy. In: Rothman KJ, Greenland S, Lash TL, eds. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2008. p. 168–82.
Greenland S. Partial and marginal matching in case-control studies. In: Moolgavkar SH, Prentice RL, editors. Modern statistical methods in chronic disease epidemiology. New York: Wiley; 1986. p. 35–49.
Rothman KJ, Greenland S, Lash TL. Case-control studies. In: Rothman KJ, Greenland S, Lash TL, eds. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2008. p. 111–27.
Jewell NP. Statistics for epidemiology, chapter 5. Boca Raton: Chapman & Hall/CRC; 2004.
Glymour MM, Greenland S. Causal diagrams. In: Rothman KJ, Greenland S, Lash T, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 183–209.
Jewell NP. Statistics for epidemiology, chapter 8. Boca Raton: Chapman & Hall/CRC; 2004.
Greenland S, Mansournia MA. Limitations of individual causal models, causal graphs, and ignorability assumptions, as illustrated by random confounding and design unfaithfulness. Eur J Epidemiol. 2015;30:1101–10.
Mansournia MA, Higgins JPT, Sterne JAC, Hernán MA. Biases in randomized trials: a conversation between trialists and epidemiologists. Epidemiology. 2017;28:54–9.
Suzuki E, Tsuda T, Mitsuhashi T, Mansournia MA, Yamamoto E. Errors in causal inference: an organizational schema for systematic error and random error. Ann Epidemiol. 2016;26:788–93.
Mansournia MA, Etminan M, Danaei G, Kaufman JS, Collins G. Handling time varying confounding in observational research. BMJ 2017;359:j4587.
Rothman KJ. Modern epidemiology, chapter 13. Boston: Little, Brown; 1986.
Pearce N. Analysis of matched case-control studies. BMJ. 2016;352:i969.
Gharibzadeh S, Mohammad K, Rahimiforoushani A, Amouzegar A, Mansournia MA. Standardization as a tool for causal inference in medical research. Arch Iran Med. 2016;19:666–70.
Greenland S, Lash TL. Bias analysis. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 345–80.
Hernán MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15:615–25.
Gail MH. Selection bias. In: Armitage P, Colton T, editors. Encyclopedia of biostatistics. 2nd ed. Hoboken: John Wiley & Sons; 2005. p. 4869–70.
Mansournia MA, Hernán MA, Greenland S. Matched designs and causal diagrams. Int J Epidemiol. 2013;42:860–9.
Smith PG, Day NE. Matching and confounding in the design and analysis of epidemiological case-control studies. In: Blithell JF, Coppi R, editors. Perspectives in medical statistics. New York: Academic Press; 1981.
Kupper LL, Karon JM, Kleinbaum DG, Morgenstern H, Lewis DK. Matching in epidemiologic studies: validity and efficiency considerations. Biometrics. 1981;37:271–92.
Samuels ML. Matching and design efficiency in epidemiological studies. Biometrika. 1981;68:577–88.
Thomas DC, Greenland S. The relative efficiencies of matched and independent sample designs for case-control studies. J Chronic Dis. 1983;36:685–97.
Smith PG, Day NE. The design of case-control studies: the influence of confounding and interaction effects. Int J Epidemiol. 1984;13:356–65.
Thomas DC, Greenland S. The efficiency of matching in case-control studies of risk-factor interactions. J Chronic Dis. 1985;38:569–74.
Greenland S. Estimating variances of standardized estimators in case-control studies and sparse data. J Chronic Dis. 1986;39:473–7.
Greenland S, Rothman KJ. Introduction to stratified analysis. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 258–82.
Clayton D, Hills M. Statistical models in epidemiology, chapter 18. New York: Oxford University Press; 1993.
Greenland S. Re: Estimating relative risk functions in case-control studies using a nonparametric logistic regression. Am J Epidemiol. 1997;146:883–4.
Breslow NE, Lubin JH, Marek P, Langholz B. Multiplicative models and cohort analysis. J Am Stat Assoc. 1983;78:1–12.
Greenland S. Introduction to regression modeling. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 418–55.
Greenland S. Applications of stratified analysis methods. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 283–302.
Jewell NP. Statistics for epidemiology, chapter 16. Boca Raton: Chapman & Hall/CRC; 2004.
Robinson LD, Jewell NP. Some surprising results about covariate adjustment in logistic regression. Int Stat Rev. 1991;59:227–40.
Brookmeyer R, Liang KY, Linet M. Matched case-control designs and overmatched analyses. Am J Epidemiol. 1986;124:693–701.
Greenland S. Quantifying biases in causal models: classical confounding vs collider-stratification bias. Epidemiology. 2003;14:300–6.
Didelez V, Kreiner S, Keiding N. On the use of graphical models for inference under outcome dependent sampling. Stat Sci. 2010;25:368–87.
Kalish LA. Matching on a non-risk factor in the design of case-control studies does not always result in an efficiency loss. Am J Epidemiol. 1986;123:551–4.
Mansournia MA, Altman DG. Inverse probability weighting. BMJ. 2016;15(352):i189.
Mansournia MA, Danaei G, Forouzanfar MH, Mahmoudi M, Jamali M, Mansournia N, Mohammad K. Effect of physical activity on functional performance and knee pain in patients with osteoarthritis: analysis with marginal structural models. Epidemiology. 2012;23:631–40.
Szklo M, Nieto F. Epidemiology: beyond the basics, chapter 6. 3rd ed. Sudbury: Jones and Bartlett Publishers; 2014.
Greenland S. Tests for interaction in epidemiologic studies: a review and a study of power. Stat Med. 1983;2:243–51.
Greenland S, Maldonado G. The interpretation of multiplicative model parameters as standardized parameters. Stat Med. 1994;13:989–99.
Mohammad K, Hashemi Nazari SS, Mansournia N, Mansournia MA. Marginal versus conditional causal effects. J Biostat Epidemiol. 2015;1:121–8.
Greenland S. Dose-response and trend analysis: alternatives to category-indicator regression. Epidemiology. 1995;6:356–65.
Sjölander A, Greenland S. Ignoring the matching variables in cohort studies: when is it valid and why? Stat Med. 2013;32:4696–708.
Greenland S, Morgenstern H. Matching and efficiency in cohort studies. Am J Epidemiol. 1990;131:151–9.
Kurth T, Walker AM, Glynn RJ, Chan KA, Gaziano JM, Berger K, Robins JM. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol. 2006;163:262–70.
Greenland S, Robins JM, Pearl J. Confounding and collapsibility in causal inference. Stat Sci. 1999;14:29–46.
Mansournia MA, Greenland S. The relation of collapsibility and confounding to faithfulness and stability. Epidemiology. 2015;26:466–72.
Greenland S, Pearl J. Adjustments and their consequences: collapsibility analysis using graphical models. Int Stat Rev. 2011;79:401–26.
Pang M, Kaufman JS, Platt RW. Studying noncollapsibility of the odds ratio with marginal structural and logistic regression models. Stat Methods Med Res. 2016;25:1925–37.
Lombard HL, Doering CR. Cancer studies in Massachusetts. 2. Habits, characteristics and environment of individuals with and without cancer. N Engl J Med. 1928;198:481–7.
Lane-Claypon JE. A further report on cancer of the breast. London: Her Majesty’s Stationery Office; 1926.
VanderWeele TJ, Shpitser I. A new criterion for confounder selection. Biometrics. 2011;67:1406–13.
Greenland S, Schwartzbaum JA, Finkle WD. Problems from small samples and sparse data in conditional logistic regression analysis. Am J Epidemiol. 2000;151:531–9.
Greenland S. Small-sample bias and corrections for conditional maximum-likelihood odds-ratio estimators. Biostatistics. 2000;1:113–22.
Jewell NP. Small-sample bias of point estimators of the odds ratio from matched sets. Biometrics. 1984;40:421–35.
Greenland S, Mansournia MA, Altman DG. Sparse data bias: a problem hiding in plain sight. BMJ. 2016;27(352):i1981.
Greenland S, Mansournia MA. Penalization, bias reduction, and default priors in logistic and related categorical and survival regressions. Stat Med. 2015;34:3133–43.
Mansournia MA, Geroldinger A, Greenland S, Heinze G. Separation in logistic regression–causes, consequences, and control. Am J Epidemiol. 2017. doi:10.1093/aje/kwx299.
Shrier I. Re: the design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med. 2008;27:2740–1.
Pearl J. Remarks on the method of propensity score. Stat Med. 2009;28:1415–6.
King G, Nielsen R. Why propensity scores should not be used for matching. Vers. 2 Feb. 2016 downloaded from http://j.mp/1FQhySn.
Mansson R, Joffe MM, Sun W, Hennessy S. On the estimation and use of propensity scores in case-control and case-cohort studies. Am J Epidemiol. 2007;166:332–9.
Austin H, Flanders WD, Rothman KJ. Bias arising in case-control studies from selection of controls from overlapping groups. Int J Epidemiol. 1989;18:713–6.
Acknowledgements
The authors are grateful to David Clayton and the referees for helpful comments on earlier drafts of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mansournia, M.A., Jewell, N.P. & Greenland, S. Case–control matching: effects, misconceptions, and recommendations. Eur J Epidemiol 33, 5–14 (2018). https://doi.org/10.1007/s10654-017-0325-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-017-0325-0