Summary
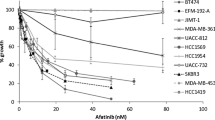
Immunotherapy of HER2-overexpressing cancers by FDA approved monoclonal antibodies (mAbs) such as trastuzumab and pertuzumab has shown promising results. We have recently produced a novel humanized anti-HER2 mAb, hersintuzumab, which did not sterically inhibit binding of trastuzumab and pertuzumab to HER2, thus recognizing a distinct epitope on subdomain I + II of HER2. In this study, we assessed the in vitro and in vivo anti-tumor activity of this mAb individually and in combination with trastuzumab. Different HER2-overexpressing human cancer cell lines, including SKOV3, NCI-N87 HCC1954 and BT-474 were cultured and binding reactivity of Hersintuzumab to these cell lines was analyzed by flow cytometry. In addition, the inhibitory effect of different concentrations of hersintuzumab, trastuzumab and their combination on tumor cells growth was assessed by XTT assay. For Assessment of tumor growth inhibition in xenograft model, Balb/c athymic nude mice were subcutaneously injected with NCI-N87 and SKOV3 tumor cells and then treated intravenously with these mAbs. Our results showed that hersintuzumab could bind to all HER2-overexpressing cell lines similar to trastuzumab. In vitro experiments showed that both hersintuzumab and trastuzumab individually and in combination inhibited growth of all cell lines with the exception of HCC-1954.Inhibitory effect of the combination of mAbs was significantly higher than that of each mAb alone. Similar results were obtained in the gastric (NCI-N87) and ovarian (SKOV-3) tumor xenograft models. Hersintuzumab in combination with trastuzumab induces synergic anti-tumor effects on HER2-overexpressing cells in vitro and in vivo and is potentially a therapeutic tool for treatment of HER2-overexpressing cancers.



Similar content being viewed by others
Data availability
All available data are reported in the manuscript.
References
Olayioye MA, Neve RM, Lane HA, Hynes NE (2000) The ErbB signaling network: receptor heterodimerization in development and cancer. EMBO J 19(13):3159–3167
Roskoski R Jr (2014) The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacol Res 79:34–74
Brandt-Rauf PW, Pincus MR, Carney WP (1994) The c-erbB-2 protein in oncogenesis: molecular structure to molecular epidemiology. Crit Rev Oncog 5(2–3):313–329
Hubbard SR, Till JH (2000) Protein tyrosine kinase structure and function. Annu Rev Biochem 69(1):373–398
Maruyama IN (2014) Mechanisms of activation of receptor tyrosine kinases: monomers or dimers. Cells 3(2):304–330
Tai W, Mahato R, Cheng K (2010) The role of HER2 in cancer therapy and targeted drug delivery. J Control Release 146(3):264–275
Dittrich A, Gautrey H, Browell D, Tyson-Capper A (2014) The HER2 signaling network in breast cancer—like a spider in its web. J Mammary Gland Biol Neoplasia 19(3–4):253–270
Mukohara T (2011) Mechanisms of resistance to anti-human epidermal growth factor receptor 2 agents in breast cancer. Cancer Sci 102(1):1–8
Kaptain S, Tan LK, Chen B (2001) Her-2/neu and breast cancer. Diagn Mol Pathol 10(3):139–152
Schuell B, Gruenberger T, Scheithauer W, Zielinski C, Wrba F (2006) HER 2/neu protein expression in colorectal cancer. BMC Cancer 6(1):123
McKenzie S, DeSombre K, Bast B, Hollis D, Whitaker R, Berchuck A, Boyer C, Bast RC Jr (1993) Serum levels of HER-2 neu (C-erbB-2) correlate with overexpression of p185neu in human ovarian cancer. Cancer 71(12):3942–3946
Hirashima N, Takahashi W, Yoshii S, Yamane T, Ooi A (2001) Protein overexpression and gene amplification of c-erbB-2 in pulmonary carcinomas: a comparative immunohistochemical and fluorescence in situ hybridization study. Mod Pathol 14(6):556–562
Matsui Y, Inomata M, Tojigamori M, Sonoda K, Shiraishi N, Kitano S (2005) Suppression of tumor growth in human gastric cancer with HER2 overexpression by an anti-HER2 antibody in a murine model. Int J Oncol 27(3):681–685
Eltze E, Wülfing C, Von Struensee D, Piechota H, Buerger H, Hertle L (2005) Cox-2 and Her2/neu co-expression in invasive bladder cancer. Int J Oncol 26(6):1525–1531
Iqbal N, Iqbal N (2014) Human epidermal growth factor receptor 2 (HER2) in cancers: overexpression and therapeutic implications. Molecular biology international 2014:1–9
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. 235(4785):177–182
Nitta H, Kelly BD, Allred C, Jewell S, Banks P, Dennis E, Grogan TM (2016) The assessment of HER2 status in breast cancer: the past, the present, and the future. Pathol Int 66(6):313–324
Cervantes A, Roselló S, Roda D, Rodriguez-Braun E (2008) The treatment of advanced gastric cancer: current strategies and future perspectives. Annals of oncology 19(suppl_5):v103–v107
Teplinsky E, Muggia F (2015) EGFR and HER2: is there a role in ovarian cancer? Translat Cancer Res 4(1):107–117
Smith MB, Reardon J, Olson EM (2012) Pertuzumab for the treatment of patients with previously untreated HER2-positive metastatic breast cancer. Drugs Today (Barc) 48(11):713–722. https://doi.org/10.1358/dot.2012.48.11.1885879
Faratian D, Zweemer AJ, Nagumo Y, Sims AH, Muir M, Dodds M, Mullen P, Um I, Kay C, Hasmann M (2011) Trastuzumab and pertuzumab produce changes in morphology and estrogen receptor signaling in ovarian cancer xenografts revealing new treatment strategies. Clin Cancer Res 17(13):4451–4461
Ko B-K, Lee S-Y, Lee Y-H, Hwang I-S, Persson H, Rockberg J, Borrebaeck C, Park D, Kim K-T, Uhlen M (2015) Combination of novel HER2-targeting antibody 1E11 with trastuzumab shows synergistic antitumor activity in HER2-positive gastric cancer. Mol Oncol 9(2):398–408
Meng Y, Zheng L, Yang Y, Wang H, Dong J, Wang C, Zhang Y, Yu X, Wang L, Xia T (2016) A monoclonal antibody targeting ErbB2 domain III inhibits ErbB2 signaling and suppresses the growth of ErbB2-overexpressing breast tumors. Oncogenesis 5(3):e211–e211
Nahta R, Hung M-C, Esteva FJ (2004) The HER-2-targeting antibodies Trastuzumab and Pertuzumab synergistically inhibit the survival of breast Cancer cells. Cancer Res 64:2343–2346
Shen G, Huang H, Zhang A, Zhao T, Hu S, Cheng L, Liu J, Xiao W, Ling B, Wu Q (2011) In vivo activity of novel anti-ErbB2 antibody chA21 alone and with paclitaxel or Trastuzumab in breast and ovarian cancer xenograft models. Cancer Immunol Immunother 60(3):339–348
Amiri MM, Golsaz-Shirazi F, Soltantoyeh T, Hosseini-Ghatar R, Bahadori T, Khoshnoodi J, Navabi SS, Farid S, Karimi-Jafari MH, Jeddi-Tehrani M (2018) Hersintuzumab: a novel humanized anti-HER2 monoclonal antibody induces potent tumor growth inhibition. Investig New Drugs 36(2):171–186
Shokri F, Jeddi-Tehrani M, Amiri MM (2019) Production of hersintuzumab: a new humanized antibody against HER2 for cancer treatment. Google Patents,
Arndt-Jovin DJ, Botelho MG, Jovin TM (2014) Structure-function relationships of ErbB RTKs in the plasma membrane of living cells. Cold Spring Harb Perspect Biol 6(4):a008961
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Hegg R, Tausch C, Seo JH, Tsai Y-F, Ratnayake J (2013) Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol 24(9):2278–2284
Molina MA, Codony-Servat J, Albanell J, Rojo F, Arribas J, Baselga J (2001) Trastuzumab (herceptin), a humanized anti-Her2 receptor monoclonal antibody, inhibits basal and activated Her2 ectodomain cleavage in breast cancer cells. Cancer Res 61(12):4744–4749
Scheuer W, Friess T, Burtscher H, Bossenmaier B, Endl J, Hasmann M (2009) Strongly enhanced antitumor activity of Trastuzumab and Pertuzumab combination treatment on HER2-positive human xenograft tumor models. Cancer Res 69(24):9330–9336. https://doi.org/10.1158/0008-5472.CAN-08-4597
Hosseini-Ghatar R, Soltantoyeh T, Bahadori M, Golara M, Hassannia H, Khosravi-Eghbal R, Khoshnoodi J, Judaki MA, Golsaz-Shirazi F, Jeddi-Tehrani M (2017) Epitope mapping of human HER2 specific mouse monoclonal antibodies using recombinant extracellular subdomains of HER2. Asian Pac J Cancer Prev 18(11):3103–3110
Zhang X, Chen J, Weng Z, Li Q, Zhao L, Yu N, Deng L, Xu W, Yang Y, Zhu Z (2020) A new anti-HER2 antibody that enhances the anti-tumor efficacy of trastuzumab and pertuzumab with a distinct mechanism of action. Mol Immunol 119:48–58
Soltantoyeh T, Bahadori T, Hosseini-Ghatar R, Khoshnoodi J, Roohi A, Mobini M, Golsaz-Shirazi F, Jeddi-Tehrani M, Amiri MM, Shokri F (2018) Differential effects of inhibitory and stimulatory anti-HER2 monoclonal antibodies on AKT/ERK signaling pathways. Asian Pacific journal of cancer prevention: APJCP 19(8):2255–2262
Moasser MM, Basso A, Averbuch SD, Rosen N (2001) The tyrosine kinase inhibitor ZD1839 (“Iressa”) inhibits HER2-driven signaling and suppresses the growth of HER2-overexpressing tumor cells. Cancer Res 61(19):7184–7188
Zhang H, Wang Y, Wu Y, Jiang X, Tao Y, Yao Y, Peng Y, Chen X, Fu Y, Yu L (2017) Therapeutic potential of an anti-HER2 single chain antibody–DM1 conjugates for the treatment of HER2-positive cancer. Signal transduction and targeted therapy 2(1):1–11
Yu L, Wang Y, Yao Y, Li W, Lai Q, Li J, Zhou Y, Kang T, Xie Y, Wu Y (2014) Eradication of growth of HER2-positive ovarian cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate in mouse xenograft model. International Journal of Gynecologic Cancer 24(7):1158–1164
Yamashita-Kashima Y, Iijima S, Yorozu K, Furugaki K, Kurasawa M, Ohta M, Fujimoto-Ouchi K (2011) Pertuzumab in combination with trastuzumab shows significantly enhanced antitumor activity in HER2-positive human gastric cancer xenograft models. Clin Cancer Res 17(15):5060–5070
Shu M, Yan H, Xu C, Wu Y, Chi Z, Nian W, He Z, Xiao J, Wei H, Zhou Q (2020) A novel anti-HER2 antibody GB235 reverses Trastuzumab resistance in HER2-expressing tumor cells in vitro and in vivo. Sci Rep 10(1):1–12
Claret FX, Vu TT (2012) Trastuzumab: updated mechanisms of action and resistance in breast cancer. Front Oncol 2:62
Acknowledgements
This study was partially supported by grants from Tehran University of Medical Sciences (Grant No. 97-02-27-38550), Avicenna Research Institute (Grant No. 97-002) and National Animal Modeling Network and In vivo Research, Council for Development of Stem Cell Sciences and Technologies, Vice-Presidency for Science and Technology, grant number 98/11611.
Funding
The work was supported by grants from Tehran University of Medical Sciences (grant number 97–02–27-38550), Avicenna Research Institute (grant number 97–002) and National Animal Modeling Network and in vivo Research, Council for Development of Stem Cell Sciences and Technologies, Vice-Presidency for Science and Technology (grant number 98/11611).
Author information
Authors and Affiliations
Contributions
FS and MMA made substantial contributions to the study conception, design, analysis and interpretation of the data. FS made substantial contributions to the design, acquisition, analysis and interpretation of the data. MM, FG-S, TB, MAJ, FF, HAZ, FNH, MM and MJ-T contributed to the acquisition of the data. The first draft of the manuscript was written by FS and MMA; FS commented on subsequent versions of the manuscript. All authors approved the final manuscript submitted to the journal.
Corresponding authors
Ethics declarations
Conflict of interest
Fariba Shiravi declares that she has no conflict of interest. Mehdi Mohammadi declares that he has no conflict of interest. Forough Golsaz-Shirazi declares that she has no conflict of interest. Tannaz Bahadori declares that she has no conflict of interest. Mohammad Ali Judaki declares that he has no conflict of interest. Forough Fatemi declares that she has no conflict of interest. Hengameh Ahmadi Zare declares that she has no conflict of interest. Farzaneh Notash Haghighat declares that she has no conflict of interest. Maryam Mobini declares that she has no conflict of interest. Mahmood Jeddi-Tehrani declares that he has no conflict of interest. Mohammad Mehdi Amiri declares that he has no conflict of interest. Fazel Shokri declares that he has no conflict of interest.
Ethics approval
This study was approved by the Ethical Committee of Tehran University of Medical Sciences. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shiravi, F., Mohammadi, M., Golsaz-Shirazi, F. et al. Potent synergistic anti-tumor activity of a novel humanized anti-HER2 antibody hersintuzumab in combination with trastuzumab in xenograft models. Invest New Drugs 39, 697–704 (2021). https://doi.org/10.1007/s10637-020-01048-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-01048-4