Abstract
Background
Emergency presentation (EP) of cancer, a new cancer diagnosis made following an emergency department (ED) visit, is associated with worse patient outcomes and greater organizational stress on healthcare systems. Pancreatic cancer has the highest rate of EPs among European studies but remains understudied in the U.S.
Aims
To evaluate the association between pancreatic cancer EPs and cancer stage, treatment, and survival.
Methods
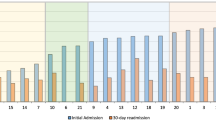
We conducted a retrospective cohort study among patients with pancreatic adenocarcinoma diagnosed from 2007 to 2019 at a tertiary-care Veterans Affairs medical center. Electronic health records were reviewed to identify EP cases, defined as a new pancreatic cancer diagnosis made within 30 days of an ED visit where cancer was suspected. We used multivariate logistic regression models and Cox proportional hazards models to examine the associations between EPs and cancer stage, treatment, and survival.
Results
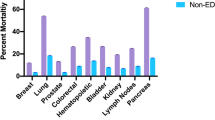
Of 243 pancreatic cancer patients, 66.7% had EPs. There was no difference in stage by EP status. However, patients diagnosed through EPs were 72% less likely to receive cancer treatment compared to non-emergency presenters (adjusted OR 0.28; 95% CI 0.13–0.57). Patients with EPs also had a 73% higher mortality risk (adjusted HR 1.73; 95% CI 1.29–2.34). This difference in mortality remained statistically significant after adjusting for cancer stage and receipt of cancer treatment (adjusted HR 1.47; 95% CI 1.09–1.99).
Conclusions
Pancreatic cancer EPs are common and independently associated with lower treatment rates and survival. Enhanced understanding of process breakdowns that lead to EPs can help identify care gaps and inform future quality improvement efforts.
Similar content being viewed by others
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- BMI:
-
Body mass index
- CCR:
-
Cancer Care Registry
- CDW:
-
Corporate data warehouse
- CI:
-
Confidence interval
- CMS:
-
Centers for Medicare and Medicaid Services
- CPT:
-
Current Procedural Terminology
- ECOG:
-
Eastern Cooperative Oncology Group
- ED:
-
Emergency department
- EP:
-
Emergency presentation
- EHR:
-
Electronic health record
- HR:
-
Hazards ratios
- ICD:
-
International Classification of Disease
- IQR:
-
Interquartile range
- NASEM:
-
National Academies of Sciences, Engineering, and Medicine
- NCIN:
-
National Cancer Intelligence Network
- OR:
-
Odds ratio
- U.K.:
-
United Kingdom
- U.S.:
-
United States
- VA:
-
Veterans Affairs
References
Lyratzopoulos G, Saunders CL, Abel GA. Are emergency diagnoses of cancer avoidable? A proposed taxonomy to motivate study design and support service improvement. Future Oncol Lond Engl 2014;10:1329–1333.
Elliss-Brookes L, McPhail S, Ives A et al. Routes to diagnosis for cancer - determining the patient journey using multiple routine data sets. Br J Cancer 2012;107:1220–1226.
Kang S, McLeod SL, Walsh C et al. Patient outcomes associated with cancer diagnosis through the emergency department: A systematic review. Acad Emerg Med Off J Soc Acad Emerg Med. 2023. https://doi.org/10.1111/acem.14671.
Abel GA, Mendonca SC, McPhail S et al. Emergency diagnosis of cancer and previous general practice consultations: insights from linked patient survey data. Br J Gen Pract J R Coll Gen Pract 2017;67:e377–e387.
Pham TM, Gomez-Cano M, Salika T et al. Diagnostic route is associated with care satisfaction independently of tumour stage: evidence from linked English cancer patient experience survey and cancer registration data. Cancer Epidemiol 2019;61:70–78.
National Cancer Intelligence Network. Routes to diagnosis of cancer by stage, 2012–2013. Public Health England [http://www.ncin.org.uk/view?rid=3071]. Accessed February 18, 2023.
National Cancer Intelligence Network. Routes to diagnosis: exploring emergency presentations. Public Health England [http://www.ncin.org.uk/publications/data_briefings/routes_to_diagnosis_exploring_emergency_presentations]. Accessed March 30, 2023.
Herbert A, Abel GA, Winters S et al. Are inequalities in cancer diagnosis through emergency presentation narrowing, widening or remaining unchanged? Longitudinal analysis of English population-based data 2006–2013. J Epidemiol Community Health 2019;73:3–10.
Rahib L, Smith BD, Aizenberg R et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913–2921.
Khalaf N, El-Serag HB, Abrams HR et al. Burden of pancreatic cancer-from epidemiology to practice. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2020. https://doi.org/10.1016/j.cgh.2020.02.054.
Siegel RL, Miller KD, Wagle NS et al. Cancer statistics, 2023. CA Cancer J Clin 2023;73:17–48.
McPhail S, Swann R, Johnson SA et al. Risk factors and prognostic implications of diagnosis of cancer within 30 days after an emergency hospital admission (emergency presentation): an International Cancer Benchmarking Partnership (ICBP) population-based study. Lancet Oncol 2022;23:587–600.
US Preventive Services Task Force, Owens DK, Davidson KW, et al. Screening for Pancreatic Cancer: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA 2019; 322:438–444.
Conroy T, Desseigne F, Ychou M et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817–1825.
Paniccia A, Hosokawa P, Henderson W et al. Characteristics of 10-Year survivors of pancreatic ductal adenocarcinoma. JAMA Surg 2015;150:701–710.
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol 2019;10:10–27.
Sohn M-W, Arnold N, Maynard C et al. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr 2006;4:2.
Hawn MT, Graham LA, Richman JS et al. Risk of major adverse cardiac events following noncardiac surgery in patients with coronary stents. JAMA 2013;310:1462–1472.
Miao B, Hernandez AV, Alberts MJ et al. Incidence and predictors of major adverse cardiovascular events in patients with established atherosclerotic disease or multiple risk factors. J Am Heart Assoc 2020;9:e014402.
Lapham GT, Achtmeyer CE, Williams EC et al. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Med Care 2012;50:179–187.
Zhou Y, Abel GA, Hamilton W et al. Diagnosis of cancer as an emergency: a critical review of current evidence. Nat Rev Clin Oncol 2017;14:45–56.
Hargarten SW, Richards MJ, Anderson AJ. Cancer presentation in the emergency department: a failure of primary care. Am J Emerg Med 1992;10:290–293.
Singhi AD, Koay EJ, Chari ST et al. Early detection of pancreatic cancer: opportunities and challenges. Gastroenterology 2019;156:2024–2040.
Tataru D, Jack RH, Lind MJ et al. The effect of emergency presentation on surgery and survival in lung cancer patients in England, 2006–2008. Cancer Epidemiol 2015;39:612–616.
Comber H, Sharp L, de Camargo CM et al. Causes and outcomes of emergency presentation of rectal cancer. Int J Cancer 2016;139:1031–1039.
McPhail S, Elliss-Brookes L, Shelton J et al. Emergency presentation of cancer and short-term mortality. Br J Cancer 2013;109:2027–2034.
Danckert B, Falborg AZ, Christensen NL et al. Routes to diagnosis and the association with the prognosis in patients with cancer - A nationwide register-based cohort study in Denmark. Cancer Epidemiol 2021;74:101983.
Nakata B, Amano R, Kimura K et al. Comparison of prognosis between patients of pancreatic head cancer with and without obstructive jaundice at diagnosis. Int J Surg Lond Engl 2013;11:344–349.
Sjo OH, Larsen S, Lunde OC et al. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis Off J Assoc Coloproctology G B Irel 2009;11:733–739.
Committee on Diagnostic Error in Health Care, Board on Health Care Services, Institute of Medicine, et al. Improving Diagnosis in Health Care. (Balogh EP, Miller BT, Ball JR, eds.). Washington (DC): National Academies Press (US), 2015. http://www.ncbi.nlm.nih.gov/books/NBK338596/. Accessed April 9, 2020.
Handley NR, Schuchter LM, Bekelman JE. Best practices for reducing unplanned acute care for patients with cancer. J Oncol Pract 2018;14:306–313.
Placido D, Yuan B, Hjaltelin JX et al. A deep learning algorithm to predict risk of pancreatic cancer from disease trajectories. Nat Med 2023;29:1113–1122.
Schmidt-Hansen M, Berendse S, Hamilton W. Symptoms of pancreatic cancer in primary care: a systematic review. Pancreas 2016;45:814–818.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs of the United States Government.
Funding
The study was funded in part by Texas Medical Center Digestive Diseases Center (PHS grant P30DK056338); the Gordon and Betty Moore Foundation (Diagnostic Excellence Award, grant number: GBMF11505); and a Veterans Affairs Health Services Research and Development Career Development Award (1 IK2 HX003346-01A2). Drs. Khalaf, Kramer, Singh and Kanwal are additionally supported by the Veterans Administration Health Services Research and Development Service Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413). Dr. Singh is also supported by the VA National Center for Patient Safety, the VA HSR&D Service (IIR17-127) and the Agency for Healthcare Research and Quality (R18 HS029347 and R01 HS028595).
Author information
Authors and Affiliations
Contributions
NK, BA and HS contributed to study concept and design, analysis and interpretation of data, drafting of the manuscript and critical revision of the manuscript for important intellectual content. NK, FK, and HS contributed to obtaining funds and providing material support. YL contributed to acquisition of data, analysis and interpretation of data. JK contributed to study concept and design, acquisition of data, analysis and interpretation of data, critical revision of the manuscript and study supervision. HES, FK and HS contributed to study concept and design, interpretation of data, and critical revision of the manuscript. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflicts of interest
No relevant conflicts of interest exist.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Baylor College of Medicine and Research and Development at the Michael E. DeBakey Veterans Affairs Medical Center approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khalaf, N., Ali, B., Liu, Y. et al. Emergency Presentations Predict Worse Outcomes Among Patients with Pancreatic Cancer. Dig Dis Sci 69, 603–614 (2024). https://doi.org/10.1007/s10620-023-08207-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08207-6