Abstract
Background and Aim
Cholangiocarcinoma (CCA) often develops after the hepatic resection for hepatolithiasis as well as indwelling it. We studied the incidence and prognosis of subsequent CCA in patients with hepatolithiasis in South Korea.
Methods
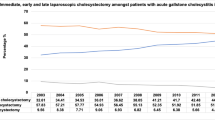
We identified individuals with diagnosed CCA at the time of or after surgery, during 2002–2016, from the Korean National Health Insurance. The incidences and survival rates of subsequent CCA were analyzed and compared with concomitant CCA. The standardized incidence ratios (SIRs) of CCA in this cohort were evaluated in the standard Korean population. All data were stratified by the presence of intrahepatic or extrahepatic CCA, age and sex.
Results
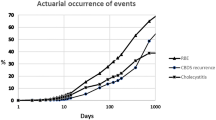
Of the 7852 patients with hepatectomy for BDS, 433 (5.84%) had concomitant CCA. Over the 12-year follow-up, 107 of 7419 (1.98%) patients were diagnosed with subsequent CCA. Patients with hepatic resection for BDS revealed higher SIRs for subsequent CCA (12.89, 95% CI 10.96–15.15) in cases of both intrahepatic CCA (13.40, 10.55–17.02) and extrahepatic CCA (12.42, 9.98–15.46). The median survival time for subsequent CCA was 0.87 years, while that for concomitant CCA was 2.79 years. Having subsequent CCA (HR 2.71, 95% CI 2.17–3.40) and being male (HR 1.28, 1.05–1.57) were related to a shorter survival time. The CCA site and age at CCA diagnosis were not related to prognoses.
Conclusions
Subsequent CCA developed in 2% of the patients with hepatic resection for benign BDS until 10 years and was associated with poorer prognoses than concomitant CCA. Future studies focused on the long-term surveillance for CCA in such patients are needed.



Similar content being viewed by others
References
Kim HJ, Kim JS, Joo MK, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol. 2015;21:13418–13431.
Catena M, Aldrighetti L, Finazzi R, et al. Treatment of non-endemic hepatolithiasis in a Western country. The role of hepatic resection. Ann R Coll Surg Engl. 2006;88:383–389.
Kim YT, Byun JS, Kim J, et al. Factors predicting concurrent cholangiocarcinomas associated with hepatolithiasis. Hepatogastroenterology. 2003;50:8–12.
Tsuyuguchi T, Miyakawa K, Sugiyama H, et al. Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy. J Hepatobiliary Pancreat Sci. 2014;21:795–800.
Suzuki Y, Mori T, Yokoyama M, et al. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014;21:617–622.
Li SQ, Liang LJ, Peng BG, et al. Hepaticojejunostomy for hepatolithiasis: a critical appraisal. World J Gastroenterol. 2006;12:4170–4174.
Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007;31:479–482.
Tabrizian P, Jibara G, Shrager B, Schwartz ME, Roayaie S. Hepatic resection for primary hepatolithiasis: a single-center Western experience. J Am Coll Surg. 2012;215:622–626.
Park HM, Hur YH, Cho CK, Koh YS, Kim HJ, Park EK. Incidence of underlying biliary neoplasm in patients after major hepatectomy for preoperative benign hepatolithiasis. Ann Hepatobiliary Pancreat Surg. 2016;20:173–179.
Lee CC, Wu CY, Chen GH. What is the impact of coexistence of hepatolithiasis on cholangiocarcinoma? J Gastroenterol Hepatol. 2002;17:1015–1020.
Chen DW, Tung-Ping Poon R, Liu CL, Fan ST, Wong J. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386–393.
Lin CC, Lin PY, Chen YL. Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: clinical implications. World J Gastroenterol. 2013;19:375–380.
Kim HJ, Kim JS, Suh SJ, et al. Cholangiocarcinoma risk as long-term outcome after hepatic resection in the hepatolithiasis patients. World J Surg. 2015;39:1537–1542.
Hong SN, Kim HJ, Kim KH, Han SJ, Ahn IM, Ahn HS. Risk of incident Mycobacterium tuberculosis infection in patients with inflammatory bowel disease: a nationwide population-based study in South Korea. Aliment Pharmacol Ther. 2017;45:253–263.
Li SQ, Liang LJ, Peng BG, et al. Outcomes of liver resection for intrahepatic stones: a comparative study of unilateral versus bilateral disease. Ann Surg. 2012;255:946–953.
Suzuki Y, Mori T, Abe N, et al. Predictive factors for cholangiocarcinoma associated with hepatolithiasis determined on the basis of Japanese Multicenter study. Hepatol Res. 2012;42:166–170.
Liu ZY, Zhou YM, Shi LH, Yin ZF. Risk factors of intrahepatic cholangiocarcinoma in patients with hepatolithiasis: a case-control study. Hepatobiliary Pancreat Dis Int. 2011;10:626–631.
Meng ZW, Han SH, Zhu JH, Zhou LY, Chen YL. Risk Factors for Cholangiocarcinoma after initial hepatectomy for intrahepatic stones. World J Surg. 2017;41:835–843.
Park JS, Jeong S, Lee DH, et al. Risk factors for longterm outcomes after initial treatment in hepatolithiasis. J Korean Med Sci. 2013;28:1627–1631.
Jeong YI, Shin HE, Lee SE, et al. Prevalence of clonorchis sinensis infection among residents along 5 major rivers in the Republic of Korea. Korean J Parasitol. 2016;54:215–219.
Park B, Jung KW, Oh CM, Choi KS, Suh M, Jun JK. Ten-year changes in the hepatitis B prevalence in the birth cohorts in Korea: results from nationally representative cross-sectional surveys. Medicine (Baltimore). 2015;94:e1469.
Shon HS, Choi HY, Kim JR, et al. Comparison and analysis of the prevalence of hepatitis C virus infection by region in the Republic of Korea during 2005–2012. Clin Mol Hepatol. 2015;21:249–256.
Lim SH, Kwon JW, Kim N, et al. Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol. 2013;13:104.
Bergquist A, von Seth E. Epidemiology of cholangiocarcinoma. Best Pract Res Clin Gastroenterol. 2015;29:221–232.
Welzel TM, Graubard BI, El-Serag HB, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case-control study. Clin Gastroenterol Hepatol. 2007;5:1221–1228.
Cai H, Kong WT, Chen CB, et al. Cholelithiasis and the risk of intrahepatic cholangiocarcinoma: a meta-analysis of observational studies. BMC Cancer. 2015;15:831.
Uenishi T, Hamba H, Takemura S, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009;198:199–202.
Chen MF, Jan YY, Hwang TL, et al. Impact of concomitant hepatolithiasis on patients with peripheral cholangiocarcinoma. Dig Dis Sci. 2000;45:312–316.
Guglielmi A, Ruzzenente A, Valdegamberi A, et al. Hepatolithiasis-associated cholangiocarcinoma: results from a multi-institutional national database on a case series of 23 patients. Eur J Surg Oncol. 2014;40:567–575.
Fan ST, Wong J. Complications of hepatolithiasis. J Gastroenterol Hepatol. 1992;7:324–327.
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146:843–853.
Nakanuma Y, Terada T, Tanaka Y, Ohta G. Are hepatolithiasis and cholangiocarcinoma aetiologically related? A morphological study of 12 cases of hepatolithiasis associated with cholangiocarcinoma. Virchows Arch A Pathol Anat Histopathol. 1985;406:45–58.
Li FY, Cheng NS, Mao H, et al. Significance of controlling chronic proliferative cholangitis in the treatment of hepatolithiasis. World J Surg. 2009;33:2155–2160.
Zhou Q, Gong Y, Huang F, et al. Expression levels and significance of nuclear factor-κB and epidermal growth factor receptor in hepatolithiasis associated with intrahepatic cholangiocarcinoma. Dig Surg. 2013;30:309–316.
Sung R, Lee SH, Ji M, et al. Epithelial-mesenchymal transition-related protein expression in biliary epithelial cells associated with hepatolithiasis. J Gastroenterol Hepatol. 2014;29:395–402.
Tajima Y, Kanematsu T. Hepatolithiasis and intrahepatic cholangiocarcinoma: carcinogenesis based on molecular mechanisms. J Hepato Biliary Pancreat Surg. 2005;12:463–466.
Ohta T, Nagakawa T, Ueda N, et al. Mucosal dysplasia of the liver and the intraductal variant of peripheral cholangiocarcinoma in hepatolithiasis. Cancer. 1991;68:2217–2223.
Chang JS, Tsai CR, Chen LT. Medical risk factors associated with cholangiocarcinoma in Taiwan: a population-based case–control study. PLoS ONE. 2013;8:e69981.
Palmer WC, Patel T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. J Hepatol. 2012;57:69–76.
Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54:173–184.
Lim MK, Ju YH, Franceschi S, et al. Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg. 2006;75:93–96.
Antwi SO, Mousa OY, Patel T. Racial, ethnic, and age disparities in incidence and survival of intrahepatic cholangiocarcinoma in the United States; 1995–2014. Ann Hepatol. 2018;17:604–614.
Korean Statistical Information Service. Population by Census, 2016. http://kosis.kr/eng/. Accessed August 8, 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no potential conflicting interests related to this paper.
Rights and permissions
About this article
Cite this article
Kim, H.J., Kang, T.U., Swan, H. et al. Incidence and Prognosis of Subsequent Cholangiocarcinoma in Patients with Hepatic Resection for Bile Duct Stones. Dig Dis Sci 63, 3465–3473 (2018). https://doi.org/10.1007/s10620-018-5262-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5262-6