Abstract
Background
Although current guideline recommends selective use of pre-endoscopic prokinetics to increase diagnostic yield in upper gastrointestinal bleeding (UGIB) patients, no data to guide the use of these drugs are available.
Aims
We aimed to investigate predictive factors for endoscopic visibility and develop simple and useful strategies for pre-endoscopic prokinetics use in UGIB patients.
Methods
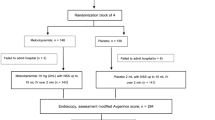
A total of 220 consecutive patients who underwent upper endoscopy for suspicious UGIB were enrolled. Patients were randomly allocated to either a training or a validation set at a 2:1 ratio. Significant parameters on univariate analysis were subsequently tested by a classification and regression tree (CART) analysis.
Results
Time to endoscopy and nasogastric aspirate findings were independently related to endoscopic visibility. The CART analysis generated algorithms proposed sequential use of time to endoscopy (≤5.2 vs. >5.2 h) and nasogastric aspirate findings (red blood or coffee rounds vs. clear aspirate) for predicting endoscopic visibility. Prediction of unacceptable visibility in the validation set produced sensitivity, specificity, positive predictive value, and negative predictive value of 75.8, 67.5, 65.8, and 77.1 %, respectively. Accurate prediction for visibility was identified in 52 of 73 patients (71.2 %).
Conclusions
Time to endoscopy and nasogastric aspirate findings were independently related to endoscopic visibility in patients with UGIB. A decision-tree model incorporating these two variables may be useful for selecting UGIB patients who benefit from pre-endoscopic prokinetics use.




Similar content being viewed by others
References
Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90:206–210.
van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003;98:1494–1499.
Loperfido S, Baldo V, Piovesana E, et al. Changing trends in acute upper-GI bleeding: a population-based study. Gastrointest Endosc. 2009;70:212–224.
Marmo R, Del Piano M, Rotondano G et al. Mortality from nonulcer bleeding is similar to that of ulcer bleeding in high-risk patients with nonvariceal hemorrhage: a prospective database study in Italy. Gastrointest Endosc. 2012;75:263–272, 72 e1.
Adang RP, Vismans JF, Talmon JL, et al. Appropriateness of indications for diagnostic upper gastrointestinal endoscopy: association with relevant endoscopic disease. Gastrointest Endosc. 1995;42:390–397.
Jutabha R, Jensen DM. Management of upper gastrointestinal bleeding in the patient with chronic liver disease. Med Clin North Am. 1996;80:1035–1068.
Bardou M, Benhaberou-Brun D, Le Ray I, et al. Diagnosis and management of nonvariceal upper gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2012;9:97–104.
DiMaio CJ, Stevens PD. Nonvariceal upper gastrointestinal bleeding. Gastrointest Endosc Clin N Am. 2007;17:253–272, v.
Stollman NH, Putcha RV, Neustater BR, et al. The uncleared fundal pool in acute upper gastrointestinal bleeding: implications and outcomes. Gastrointest Endosc. 1997;46:324–327.
Cheng CL, Lee CS, Liu NJ, et al. Overlooked lesions at emergency endoscopy for acute nonvariceal upper gastrointestinal bleeding. Endoscopy. 2002;34:527–530.
Brullet E, Calvet X, Campo R, et al. Factors predicting failure of endoscopic injection therapy in bleeding duodenal ulcer. Gastrointest Endosc. 1996;43:111–116.
Coffin B, Pocard M, Panis Y, et al. Erythromycin improves the quality of EGD in patients with acute upper GI bleeding: a randomized controlled study. Gastrointest Endosc. 2002;56:174–179.
Frossard JL, Spahr L, Queneau PE, et al. Erythromycin intravenous bolus infusion in acute upper gastrointestinal bleeding: a randomized, controlled, double-blind trial. Gastroenterology. 2002;123:17–23.
Carbonell N, Pauwels A, Serfaty L, et al. Erythromycin infusion prior to endoscopy for acute upper gastrointestinal bleeding: a randomized, controlled, double-blind trial. Am J Gastroenterol. 2006;101:1211–1215.
Altraif I, Handoo FA, Aljumah A, et al. Effect of erythromycin before endoscopy in patients presenting with variceal bleeding: a prospective, randomized, double-blind, placebo-controlled trial. Gastrointest Endosc. 2011;73:245–250.
Bai Y, Guo JF, Li ZS. Meta-analysis: erythromycin before endoscopy for acute upper gastrointestinal bleeding. Aliment Pharmacol Ther. 2011;34:166–171.
Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol 2012;107:345–360; quiz 61.
Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101–113.
Breiman L. Classification and regression trees. Wadsworth International Group: Belmont; 1984.
Lee WC. Characterizing exposure-disease association in human populations using the Lorenz curve and Gini index. Stat Med. 1997;16:729–739.
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843.
Camilleri M. Integrated upper gastrointestinal response to food intake. Gastroenterology. 2006;131:640–658.
Pateron D, Vicaut E, Debuc E, et al. Erythromycin infusion or gastric lavage for upper gastrointestinal bleeding: a multicenter randomized controlled trial. Ann Emerg Med. 2011;57:582–589.
Jairath V, Barkun AN. The overall approach to the management of upper gastrointestinal bleeding. Gastrointest Endosc Clin N Am. 2011;21:657–670.
Corley DA, Stefan AM, Wolf M, et al. Early indicators of prognosis in upper gastrointestinal hemorrhage. Am J Gastroenterol. 1998;93:336–340.
Aljebreen AM, Fallone CA, Barkun AN. Nasogastric aspirate predicts high-risk endoscopic lesions in patients with acute upper-GI bleeding. Gastrointest Endosc. 2004;59:172–178.
Huang ES, Karsan S, Kanwal F, et al. Impact of nasogastric lavage on outcomes in acute GI bleeding. Gastrointest Endosc. 2011;74:971–980.
Lee SD, Kearney DJ. A randomized controlled trial of gastric lavage prior to endoscopy for acute upper gastrointestinal bleeding. J Clin Gastroenterol. 2004;38:861–865.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, J.U., Park, J.J., Youn, Y.H. et al. Predictive Factors for Endoscopic Visibility and Strategies for Pre-endoscopic Prokinetics Use in Patients with Upper Gastrointestinal Bleeding. Dig Dis Sci 60, 957–965 (2015). https://doi.org/10.1007/s10620-014-3393-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3393-y