Abstract
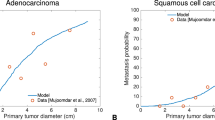
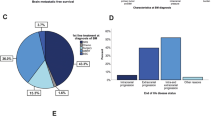
Intracranial progression after curative treatment of early-stage non-small cell lung cancer (NSCLC) occurs from 10 to 50% and is difficult to manage, given the heterogeneity of clinical presentations and the variability of treatments available. The objective of this study was to develop a mechanistic model of intracranial progression to predict survival following a first brain metastasis (BM) event occurring at a time \({T}_{BM}\). Data included early-stage NSCLC patients treated with a curative intent who had a BM as the first and single relapse site (N = 31). We propose a mechanistic mathematical model able to derive computational markers from primary tumor and BM data at \({T}_{BM}\) and estimate the amount and sizes of (visible and invisible) BMs, as well as their future behavior. These two key computational markers are \(\alpha \), the proliferation rate of a single tumor cell; and \(\mu \), the per day, per cell, probability to metastasize. The predictive value of these individual computational biomarkers was evaluated. The model was able to correctly describe the number and size of metastases at \({T}_{BM}\) for 20 patients. Parameters \(\alpha \) and \(\mu \) were significantly associated with overall survival (OS) (HR 1.65 (1.07–2.53) p = 0.0029 and HR 1.95 (1.31–2.91) p = 0.0109, respectively). Adding the computational markers to the clinical ones significantly improved the predictive value of OS (c-index increased from 0.585 (95% CI 0.569–0.602) to 0.713 (95% CI 0.700–0.726), p < 0.0001). We demonstrated that our model was applicable to brain oligoprogressive patients in NSCLC and that the resulting computational markers had predictive potential. This may help lung cancer physicians to guide and personalize the management of NSCLC patients with intracranial oligoprogression.






Similar content being viewed by others
Data availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
References
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Cancer of the Lung and Bronchus-Cancer Stat Facts. SEER.
Chargari C, Dhermain F (2013) Métastases cérébrales d’un cancer bronchique non à petites cellules : du traitement standardisé au traitement personnalisé. Rev Mal Respir Actual 5:547–556
Tabouret E et al (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer Res 32:4655–4662
Hall W, Djalilian H, Nussbaum E, Cho K (2000) Long-term survival with metastatic cancer to the brain. Med Oncol 17:279–286
Gauger J, Patz EF, Coleman RE, Herndon JE (2007) Clinical stage I non-small cell lung cancer including FDG-PET Imaging: sites and time to recurrence. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer 2:499–505
Yano T et al (1994) The first site of recurrence after complete resection in non-small-cell carcinoma of the lung. J Thorac Cardiovasc Surg 108:680–683
Sadoyama S et al (2018) Isolated brain metastases as the first relapse after the curative surgical resection in non–small-cell lung cancer patients with an EGFR mutation. Clin Lung Cancer 19:e29–e36
Figlin RA, Piantadosi S, Feld R, The Lung Cancer Study Group (1988) Intracranial recurrence of carcinoma after complete surgical resection of stage I, II, and III non-small-cell lung cancer. N Engl J Med 318:1300–1305
Novello S, Barlesi F, Califano R, Cufer T, Ekman S, Levra MG, Kerr K, Popat S, Reck M, Senan S, Simo GV (2016) Metastatic non-small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 27:v1-27
Hellman S, Weichselbaum RR (1995) Stereotactic body radiotherapy for multisite extracranial oligometastases: final report of a dose escalation trial in patients with 1 to 5 sites of metastatic disease. J Clin Oncol Off J Am Soc Clin Oncol 13:8–10
Laurie SA et al (2019) Canadian consensus: oligoprogressive, pseudoprogressive, and oligometastatic non-small-cell lung cancer. Curr Oncol Tor Ont 26:e81–e93
Schoenmaekers JJAO, Paats MS, Dingemans A-MC, Hendriks LEL (2020) Central nervous system metastases and oligoprogression during treatment with tyrosine kinase inhibitors in oncogene-addicted non-small cell lung cancer: how to treat and when? Transl Lung Cancer Res 9:2599–2617
Ceresoli GL et al (2002) Brain metastases in locally advanced nonsmall cell lung carcinoma after multimodality treatment: Risk factors analysis. Cancer 95:605–612
Zimm S, Wampler GL, Stablein D, Hazra T, Young HF (1981) Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer 48:384–394
Yamamoto M et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15:387–395
Zindler JD et al (2017) Whole brain radiotherapy versus stereotactic radiosurgery for 4–10 brain metastases: a phase III randomised multicentre trial. BMC Cancer 17:500
Gerosa M, Nicolato A, Foroni R, Tomazzoli L, Bricolo A (2005) Analysis of long-term outcomes and prognostic factors in patients with non-small cell lung cancer brain metastases treated by gamma knife radiosurgery. J Neurosurg 102:75–80
Motta M et al (2011) Gamma knife radiosurgery for treatment of cerebral metastases from non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 81:e463-468
Fuentes R et al (2018) Surgery versus stereotactic radiotherapy for people with single or solitary brain metastasis. Cochrane Database Syst Rev 8:CD012086
Aupérin A et al (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. N Engl J Med 341:476–484
Liu L et al (2020) The role of prophylactic cranial irradiation in patients with non-small cell lung cancer: an updated systematic review and meta-analysis. Front Oncol 10:11
Chang EL et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Soffietti R et al (2013) A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life results. J Clin Oncol Off J Am Soc Clin Oncol 31:65–72
Besse B et al (2015) Bevacizumab in patients with nonsquamous non-small cell lung cancer and asymptomatic, untreated brain metastases (BRAIN): a nonrandomized, phase II study. Clin Cancer Res Off J Am Assoc Cancer Res 21:1896–1903
Socinski MA et al (2018) Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 378:2288–2301
Reck M et al (2016) Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N Engl J Med 375:1823–1833
Gandhi L et al (2018) Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med 378:2078–2092
Sweeney MD, Zhao Z, Montagne A, Nelson AR, Zlokovic BV (2019) Blood-brain barrier: from physiology to disease and back. Physiol Rev 99:21–78
Cortinovis D et al (2019) Italian cohort of the nivolumab EAP in squamous NSCLC: efficacy and safety in patients With CNS metastases. Anticancer Res 39:4265–4271
Dudnik E et al (2016) Intracranial response to nivolumab in NSCLC patients with untreated or progressing CNS metastases. Lung Cancer Amst Neth 98:114–117
Goldberg SB et al (2016) Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol 17:976–983
Gauvain C et al (2018) Intracerebral efficacy and tolerance of nivolumab in non–small-cell lung cancer patients with brain metastases. Lung Cancer 116:62–66
Leighl NB et al (2020) CCTG BR.34: a randomized trial of durvalumab and tremelimumab +/- platinum-based chemotherapy in patients with metastatic (Stage IV) squamous or nonsquamous non-small cell lung cancer (NSCLC). J Clin Oncol 38:9502–9502
Powell SF et al (2019) Pembrolizumab (pembro) plus platinum-based chemotherapy (chemo) in NSCLC with brain metastases: Pooled analysis of KEYNOTE-021, 189, and 407. Ann Oncol 30:v606–v607
Wang X, Xu Y, Tang W, Liu L (2018) Efficacy and safety of radiotherapy plus EGFR-TKIs in NSCLC patients with brain metastases: a meta-analysis of published data. Transl Oncol 11:1119–1127
Levy A et al (2018) Diversity of brain metastases screening and management in non-small cell lung cancer in Europe: results of the European Organisation for Research and Treatment of Cancer Lung Cancer Group survey. Eur J Cancer 93:37–46
Gaspar L et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastases trials. Int J Radiat Oncol 37:745–751
Sperduto PW et al (2014) Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1–3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 90:526–531
Sperduto PW et al (2017) Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (Lung-molGPA). JAMA Oncol 3:827–831
Bajard A et al (2004) Multivariate analysis of factors predictive of brain metastases in localised non-small cell lung carcinoma. Lung Cancer 45:317–323
Hayashi N et al (2017) Negative impact of leukoaraiosis on the incidence of brain metastases in patients with lung cancer. J Neurooncol 135:299–306
Liotta LA, Saidel GM, Kleinerman J (1976) Stochastic model of metastases formation. Biometrics 32:535–550
Hartung N et al (2014) Mathematical modeling of tumor growth and metastatic spreading: validation in tumor-bearing mice. Cancer Res 74:6397–6407
Baratchart E et al (2015) Computational modelling of metastasis development in renal cell carcinoma. PLoS Comput Biol 11:e1004626
Benzekry S et al (2016) Modeling spontaneous metastasis following surgery: an in vivo-in silico approach. Cancer Res 76:535–547
Laird AK (1965) Dynamics of tumour growth: comparison of growth rates and extrapolation of growth curve to one cell. Br J Cancer 19:278–291
Norton L (1988) A Gompertzian model of human breast cancer growth. Cancer Res 48:7067–7071
Benzekry S et al (2014) Classical mathematical models for description and prediction of experimental tumor growth. PLoS Comput Biol 10:e1003800
Iwata K, Kawasaki K, Shigesada N (2000) A dynamical model for the growth and size distribution of multiple metastatic tumors. J Theor Biol 203:177–186
Schlicke P, Kuttler C, Schumann C (2021) How mathematical modeling could contribute to the quantification of metastatic tumor burden under therapy: insights in immunotherapeutic treatment of non-small cell lung cancer. Theor Biol Med Model 18:11
Nicolò C et al (2020) Machine learning and mechanistic modeling for prediction of metastatic relapse in early-stage breast cancer. JCO Clin Cancer Inform. https://doi.org/10.1200/CCI.19.00133
Cooley LS et al (2021) Experimental and computational modeling for signature and biomarker discovery of renal cell carcinoma progression. Mol Cancer 20:136
Benzekry S, Sentis C, Coze C, Tessonnier L, André N (2021) Development and validation of a prediction model of overall survival in high-risk neuroblastoma using mechanistic modeling of metastasis. JCO Clin Cancer Inform. https://doi.org/10.1200/CCI.20.00092
Bilous M et al (2019) Quantitative mathematical modeling of clinical brain metastasis dynamics in non-small cell lung cancer. Sci Rep 9:13018
Spratt JS, Meyer JS, Spratt JA (1995) Rates of growth of human solid neoplasms: Part I. J Surg Oncol 60:137–146
Vaghi C et al (2020) Population modeling of tumor growth curves and the reduced Gompertz model improve prediction of the age of experimental tumors. PLOS Comput Biol 16:e1007178
Bethge A, Schumacher U, Wree A, Wedemann G (2012) Are metastases from metastases clinical relevant? Computer modelling of cancer spread in a case of hepatocellular carcinoma. PLoS ONE 7:e35689
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cancer 9:302–312
MathWorks: MATLAB Documentary GlobalSearch.
Ugray Z et al (2007) Scatter search and local NLP solvers: a multistart framework for global optimization. Inf J Comput 19:328–340
Bland JM, Altman DG (2004) The logrank test. BMJ 328:1073
Davidson-Pilon C (2019) lifelines: survival analysis in Python. J Open Source Softw 4:1317
Harrell FE, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Pope WB (2018) Brain metastases: neuroimaging. In: Handbook of clinical neurology. Elsevier, vol 149, pp. 89–112
Brindle KM, Izquierdo-García JL, Lewis DY, Mair RJ, Wright AJ (2017) Brain tumor imaging. J Clin Oncol 35:2432–2438
Azin M, Demehri S (2022) STK11 loss: a novel mechanism for melanoma metastasis with therapeutic implications. J Invest Dermatol 142:1007–1009
Huang D et al (2018) Mutations of key driver genes in colorectal cancer progression and metastasis. Cancer Metastasis Rev 37:173–187
Wikman H et al (2012) Relevance of PTEN loss in brain metastasis formation in breast cancer patients. Breast Cancer Res 14:R49
Lohmann P et al (2020) PET/MRI radiomics in patients with brain metastases. Front Neurol 11:1
Zhao S et al (2021) MRI radiomic signature predicts intracranial progression-free survival in patients with brain metastases of ALK-positive non-small cell lung cancer. Transl Lung Cancer Res 10:368–380
Huang C-Y et al (2020) Radiomics as prognostic factor in brain metastases treated with Gamma Knife radiosurgery. J Neurooncol 146:439–449
Zhang J et al (2021) Computer tomography radiomics-based nomogram in the survival prediction for brain metastases from non-small cell lung cancer underwent whole brain radiotherapy. Front Oncol 10:610691
Perlikos F, Harrington KJ, Syrigos KN (2013) Key molecular mechanisms in lung cancer invasion and metastasis: a comprehensive review. Crit Rev Oncol Hematol 87:1–11
Retsky MW et al (1997) Computer simulation of a breast cancer metastasis model. Breast Cancer Res Treat 45:193–202
Pérez-García VM et al (2020) Universal scaling laws rule explosive growth in human cancers. Nat Phys 16:1232–1237
Ocaña-Tienda B et al (2023) Growth exponents reflect evolutionary processes and treatment response in brain metastases. Npj Syst Biol Appl 9:1–11
Nakamura R et al (2014) Epidermal growth factor receptor mutations: effect on volume doubling time of non–small-cell lung cancer patients. J Thorac Oncol 9:1340–1344
Zhang R et al (2017) Volume doubling time of lung adenocarcinomas considering epidermal growth factor receptor mutation status of exon 19 and 21: three-dimensional volumetric evaluation. J Thorac Dis 9:4387–4397
Robin TP et al (2018) Excellent outcomes with radiosurgery for multiple brain metastases in ALK and EGFR driven non-small cell lung cancer. J Thorac Oncol 13:715–720
Wu Y-L et al (2020) Osimertinib in resected EGFR -mutated non–small-cell lung cancer. N Engl J Med 383:1711–1723
Forde PM et al (2022) Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N Engl J Med. https://doi.org/10.1056/NEJMoa2202170
Felip E et al (2021) Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. The Lancet 398:1344–1357
Endo H, Inoue M (2019) Dormancy in cancer. Cancer Sci 110:474–480
Quail DF, Joyce JA (2017) The microenvironmental landscape of brain tumors. Cancer Cell 31:326–341
Gompertz B (1833) On the nature of the function expressive of the law of human mortality, and on a new mode of determining the value of life contingencies: In a letter to Francis Baily, Esq. FRS & c. Philos Trans R Soc Lond 2:252–253
Casey AE (1934) The experimental alteration of malignancy with an homologous mammalian tumor material. I: results with intratesticular inoculation. Am J Cancer 21:760
Acknowledgements
PS wants to thank Christina Kuttler for valuable discussions on the mathematical modelling method. Supported by Deutsche Forschungsgemeinschaft (DFG) through TUM International Graduate School of Science and Engineering (IGSSE), GSC 81.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceived the research idea: SB, PT. Model setup: PS, SB. Collected the data: ES, PT. Performed data analysis and presentation: PS. Wrote software to estimate parameters and simulate: PS, SB. The paper was written by ES and PS with editorial input from all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Non-small cell lung cancer is difficult to manage when brain metastases are present. This study presents a mathematical model that can be calibrated on individual patients’ data early in the treatment course to explain the growth dynamics of brain metastases and demonstrates that the mathematically derived parameters can serve as predictive tool in clinical routine care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benzekry, S., Schlicke, P., Mogenet, A. et al. Computational markers for personalized prediction of outcomes in non-small cell lung cancer patients with brain metastases. Clin Exp Metastasis 41, 55–68 (2024). https://doi.org/10.1007/s10585-023-10245-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-023-10245-3