Abstract
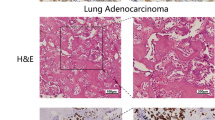
Lung adenocarcinoma is the most common and aggressive type of lung cancer with the highest incidence of bone metastasis. Epidermal growth factor-like domain multiple 6 (EGFL6) is an exocrine protein, and the expression of EGFL6 is correlated with survival of patient with lung adenocarcinoma. However, the association between EGFL6 expression in lung adenocarcinoma and bone metastasis has not been investigated. In this study, we found that EGFL6 levels in lung adenocarcinoma tissues correlate with bone metastasis and TNM stages in surgical patients. In vitro, overexpression of EGFL6 in lung adenocarcinoma cells promoted their proliferation, migration, and invasion ability compared with control by enhancing EMT process and activating Wnt/β-catenin and PI3K/AKT/mTOR pathways. In the nude mouse model, overexpression of EGFL6 enhanced tumor growth and caused greater bone destruction. Moreover, the exocrine EGFL6 of human lung adenocarcinoma cells increased osteoclast differentiation of bone marrow mononuclear macrophages (BMMs) of mice via the NF-κB and c-Fos/NFATc1 signaling pathways. However, exocrine EGFL6 had no effect on osteoblast differentiation of bone marrow mesenchymal stem cells (BMSCs). In conclusion, high expression of EGFL6 in lung adenocarcinomas is associated with bone metastasis in surgical patients. The underlying mechanism may be the increased metastatic properties of lung adenocarcinoma cells with high EGFL6 level and the enhanced osteoclast differentiation and bone resorption by exocrine EGFL6 from tumors. Therefore, EGFL6 is a potential therapeutic target to reduce the ability of lung adenocarcinomas to grow and metastasize and to preserve bone mass in patients with bone metastases from lung adenocarcinomas.
Graphical Abstract








Similar content being viewed by others
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- BMMs:
-
Bone marrow mononuclear macrophage
- BMSCs:
-
Bone marrow mesenchymal stem cells
- CCK-8:
-
Cell Counting Kit-8
- EGFL6:
-
Epidermal growth factor-like domain multiple 6
- EMT:
-
Epithelial mesenchymal transformation
- IHC:
-
Immunohistochemistry
- M-CSF:
-
Macrophage colonies stimulating factor
- MCP1:
-
Monocyte chemoattractant protein 1
- NF-κB:
-
Nuclear factor-kappa B
- OPG:
-
Osteoprotegerin
- RANKL:
-
Receptor activator of the NF-κB ligand
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30
Zhang H, Guo L, Chen J (2020) Rationale for Lung Adenocarcinoma Prevention and Drug Development based on Molecular Biology during Carcinogenesis. Onco Targets Ther 13:3085–3091
Cho YJ, Cho YM, Kim SH, Shin KH, Jung ST, Kim HS (2019) Clinical analysis of patients with skeletal metastasis of lung cancer. BMC Cancer 19(1):303
Bienz M, Saad F (2015) Management of bone metastases in prostate cancer: a review. Curr Opin Support Palliat Care 9(3):261–267
Macedo F, Ladeira K, Pinho F, Saraiva N, Bonito N, Pinto L, Goncalves F (2017) Bone Metastases: An Overview Oncol Rev 11(1):321
Yang M, Sun Y, Sun J, Wang Z, Zhou Y, Yao G, Gu Y, Zhang H, Zhao H (2018) Differentially expressed and survival-related proteins of lung adenocarcinoma with bone metastasis. Cancer Med 7(4):1081–1092
Yin JJ, Pollock CB, Kelly K (2005) Mechanisms of cancer metastasis to the bone. Cell Res 15(1):57–62
Wood SL, Pernemalm M, Crosbie PA, Whetton AD (2014) The role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targets. Cancer Treat Rev 40(4):558–566
Papotti M, Kalebic T, Volante M, Chiusa L, Bacillo E, Cappia S, Lausi P, Novello S, Borasio P, Scagliotti GV (2006) Bone sialoprotein is predictive of bone metastases in resectable non-small-cell lung cancer: a retrospective case-control study. J Clin Oncol 24(30):4818–4824
Zhang L, Hou X, Lu S, Rao H, Hou J, Luo R, Huang H, Zhao H, Jian H, Chen Z, Liao M, Wang X (2010) Predictive significance of bone sialoprotein and osteopontin for bone metastases in resected chinese non-small-cell lung cancer patients: a large cohort retrospective study. Lung Cancer 67(1):114–119
Peng X, Guo W, Ren T, Lou Z, Lu X, Zhang S, Lu Q, Sun Y (2013) Differential expression of the RANKL/RANK/OPG system is associated with bone metastasis in human non-small cell lung cancer. PLoS ONE 8(3):e58361
Nakamura ES, Koizumi K, Kobayashi M, Saitoh Y, Arita Y, Nakayama T, Sakurai H, Yoshie O, Saiki I (2006) RANKL-induced CCL22/macrophage-derived chemokine produced from osteoclasts potentially promotes the bone metastasis of lung cancer expressing its receptor CCR4. Clin Exp Metastasis 23(1):9–18
Chim SM, Qin A, Tickner J, Pavlos N, Davey T, Wang H, Guo Y, Zheng MH, Xu J (2011) EGFL6 promotes endothelial cell migration and angiogenesis through the activation of extracellular signal-regulated kinase. J Biol Chem 286(25):22035–22046
Chang CC, Sung WW, Hsu HT, Yeh CM, Lee CH, Chen YL, Liu TC, Yeh KT (2018) Validation of EGFL6 expression as a prognostic marker in patients with lung adenocarcinoma in Taiwan: a retrospective study. BMJ Open 8(6):e021385
An J, Du Y, Fan X, Wang Y, Ivan C, Zhang XG, Sood AK, An Z, Zhang N (2019) EGFL6 promotes breast cancer by simultaneously enhancing cancer cell metastasis and stimulating tumor angiogenesis Oncogene 38(12):2123–2134
Huo FC, Zhu WT, Liu X, Zhou Y, Zhang LS, Mou J (2021) Epidermal growth factor-like domain multiple 6 (EGFL6) promotes the migration and invasion of gastric cancer cells by inducing epithelial-mesenchymal transition. Invest New Drugs 39(2):304–316
Zhu Z, Ni H, You B, Shi S, Shan Y, Bao L, Duan B, You Y (2018) Elevated EGFL6 modulates cell metastasis and growth via AKT pathway in nasopharyngeal carcinoma. Cancer Med 7(12):6281–6289
Yeung G, Mulero JJ, Berntsen RP, Loeb DB, Drmanac R, Ford JE (1999) Cloning of a novel epidermal growth factor repeat containing gene EGFL6: expressed in tumor and fetal tissues. Genomics 62(2):304–307
Kang J, Wang J, Tian J, Shi R, Jia H, Wang Y (2020) The emerging role of EGFL6 in angiogenesis and tumor progression. Int J Med Sci 17(10):1320–1326
Rami-Porta R, Asamura H, Travis WD, Rusch VW (2017) Lung cancer - major changes in the american Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 67(2):138–155
Salvador F, Llorente A, Gomis RR (2019) From latency to overt bone metastasis in breast cancer: potential for treatment and prevention. J Pathol 249(1):6–18
Popper HH (2016) Progression and metastasis of lung cancer. Cancer Metastasis Rev 35(1):75–91
Zhang X (2019) Interactions between cancer cells and bone microenvironment promote bone metastasis in prostate cancer. Cancer Commun (Lond) 39(1):76
Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ Jr, Wu YL, Paz-Ares L (2017) Lung cancer: current therapies and new targeted treatments. Lancet 389(10066):299–311
Kuchuk M, Kuchuk I, Sabri E, Hutton B, Clemons M, Wheatley-Price P (2015) The incidence and clinical impact of bone metastases in non-small cell lung cancer. Lung Cancer 89(2):197–202
Zhang W, Bado IL, Hu J, Wan YW, Wu L, Wang H, Gao Y, Jeong HH, Xu Z, Hao X, Lege BM, Al-Ouran R, Li L, Li J, Yu L, Singh S, Lo HC, Niu M, Liu J, Jiang W, Li Y, Wong STC, Cheng C, Liu Z, Zhang XH (2021) The bone microenvironment invigorates metastatic seeds for further dissemination Cell, 184(9): p. 2471–2486.e20
Wang X, Yuan W, Wang X, Qi J, Qin Y, Shi Y, Zhang J, Gong J, Dong Z, Liu X, Sun C, Chai R, Le Noble F, Liu D (2016) The somite-secreted factor Maeg promotes zebrafish embryonic angiogenesis. Oncotarget 7(47):77749–77763
Zhang G, Chen L, Khan AA, Li B, Gu B, Lin F, Su X, Yan J (2018) miRNA-124-3p/neuropilin-1(NRP-1) axis plays an important role in mediating glioblastoma growth and angiogenesis Int J Cancer, 143(3): p. 635–644
Park JH, Lee NK, Lee SY (2017) Current understanding of RANK Signaling in Osteoclast differentiation and maturation. Mol Cells 40(10):706–713
Macian F (2005) NFAT proteins: key regulators of T-cell development and function. Nat Rev Immunol 5(6):472–484
Zhang L, Feng M, Li Z, Zhu M, Fan Y, Chu B, Yuan C, Chen L, Lv H, Hong Z, Hong D (2018) Bulleyaconitine A prevents Ti particle-induced osteolysis via suppressing NF-kappaB signal pathway during osteoclastogenesis and osteoblastogenesis. J Cell Physiol 233(9):7067–7079
Brabletz T, Kalluri R, Nieto MA, Weinberg RA (2018) EMT in cancer Nat Rev Cancer 18(2):128–134
Zhang Y, Wang X (2020) Targeting the Wnt/beta-catenin signaling pathway in cancer. J Hematol Oncol 13(1):165
Martini M, De Santis MC, Braccini L, Gulluni F, Hirsch E (2014) PI3K/AKT signaling pathway and cancer: an updated review. Ann Med 46(6):372–383
Peluso I, Yarla NS, Ambra R, Pastore G, Perry G (2019) MAPK signalling pathway in cancers: olive products as cancer preventive and therapeutic agents. Semin Cancer Biol 56:185–195
Meurette O, Mehlen P (2018) Notch Signaling in the Tumor Microenvironment. Cancer Cell 34(4):536–548
Katso R, Okkenhaug K, Ahmadi K, White S, Timms J, Waterfield MD (2001) Cellular function of phosphoinositide 3-kinases: implications for development, homeostasis, and cancer. Annu Rev Cell Dev Biol 17:615–675
Guerrero-Zotano A, Mayer IA, Arteaga CL (2016) PI3K/AKT/mTOR: role in breast cancer progression, drug resistance, and treatment. Cancer Metastasis Rev 35(4):515–524
Fattahi S, Amjadi-Moheb F, Tabaripour R, Ashrafi GH, Akhavan-Niaki H (2020) PI3K/AKT/mTOR signaling in gastric cancer: epigenetics and beyond. Life Sci 262:118513
Ediriweera MK, Tennekoon KH, Samarakoon SR (2019) Role of the PI3K/AKT/mTOR signaling pathway in ovarian cancer: Biological and therapeutic significance. Semin Cancer Biol 59:147–160
Chen H, Zhou L, Wu X, Li R, Wen J, Sha J, Wen X (2016) The PI3K/AKT pathway in the pathogenesis of prostate cancer. Front Biosci (Landmark Ed) 21:1084–1091
Iksen S, Pothongsrisit, Pongrakhananon V (2021) Targeting the PI3K/AKT/mTOR signaling pathway in Lung Cancer: an update regarding potential drugs and Natural Products. Molecules, 26(13)
Mortensen DS, Fultz KE, Xu S, Xu W, Packard G, Khambatta G, Gamez JC, Leisten J, Zhao J, Apuy J, Ghoreishi K, Hickman M, Narla RK, Bissonette R, Richardson S, Peng SX, Perrin-Ninkovic S, Tran T, Shi T, Yang WQ, Tong Z, Cathers BE, Moghaddam MF, Canan SS, Worland P, Sankar S, Raymon HK (2015) CC-223, a potent and selective inhibitor of mTOR kinase: in Vitro and in vivo characterization. Mol Cancer Ther 14(6):1295–1305
Acknowledgements
We highly appreciated the patient samples provided by the Biological Resource Center of Enze Medical Center, Taizhou Hospital, and the support of Taizhou Discipline Group Fund.
Funding
This work was supported by the Medical and Health Science and Technology Program Project of Zhejiang Province for Dun Hong, Grant/Award Number: 2020PY030; the Basic and Public Research Project of Zhejiang Province for Mingxuan Ming, Grant/Award Number: LGF19H070003.
Author information
Authors and Affiliations
Contributions
Dun Hong and Zhenghua Hong designed the study. The material preparation was performed by Xu Cheng, Xianquan Xu and Shengyu Ruan. Xinhui Wu, Feng Lu and Fangying Lu collected and analyzed the data. The animal experiment was conducted by Xiangang Jin and Mingxuan Feng. The first draft was written by Xiaoting Song. Review and editing were performed by Dun Hong, Zhenghua Hong, Renshan Ge and Haixiao Chen. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This research was approved by the Medical Ethics Committee of the Taizhou Hospital and obtained the informed consent of all patients. All experiments of animal followed the instruction of the Institutional Animal Ethics Committee of Taizhou Hospital.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

10585_2023_10219_MOESM1_ESM.jpg
Supplementary Material 1: Fig. S1 Detection of the siRNAs targeting EGFL6 and LV-EGFL6-RNAi transfection efficiency of A549 cells. (a) Western blot analysis is utilized to detect the levels of EGFL6 in blank control, normal control and three kinds of siRNA transfection. (b) RT-PCR shows that the result of EGFL6 knockdown efficiency was consistent with WB. (c,d) Fluorescence microscopy shows lentivirus transfection efficiency. (e,g) Western blot analysis shows that EGFL6 knockdown group and EGFL6 overexpression group were constructed successfully. This sequence 899 has been shown to have a greater ability to knock down EGFL6 in A549 cells, so we used it directly for EGFL6 knockdown in NCI-H292 cells. (f,h) RT-PCR verifies the result of WB
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, X., Cheng, X., Jin, X. et al. EGFL6 promotes bone metastasis of lung adenocarcinoma by increasing cancer cell malignancy and bone resorption. Clin Exp Metastasis 40, 357–371 (2023). https://doi.org/10.1007/s10585-023-10219-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-023-10219-5