Abstract
To determine the efficacy of intervention programs for young children (4–9 years) with emerging mental health needs, we conducted a review of meta-analytic and systematic reviews of the intervention literature. Of 41,061 abstracts identified and 15,076 screened, 152 review articles met the inclusion criteria. We reviewed interventions across multiple disciplines targeting: (1) general mental health concerns; (2) internalizing symptoms; (3) externalizing symptoms; (4) anxiety; (5) depression; (6) trauma; (7) symptoms of attention-deficit/hyperactivity disorder; and (8) mental health concerns associated with autism spectrum disorder. Substantial evidence was found for the efficacy of behavioral and cognitive behavioral interventions for general mental health concerns, externalizing symptoms (generally, as well as ADHD, conduct, and other behavioral symptoms) and internalizing symptoms (generally, as well as anxiety) aged 4–9 years. Emerging evidence was identified for interventions targeting trauma symptoms, depression symptoms, and social, emotional and behavioral symptoms in autism spectrum disorder in children aged 4–9 years. Currently there is only limited emerging evidence regarding non-behavioral or non-cognitive behavioral interventions for programs targeting children ages 4–9 years where the aim is to deliver an evidence-based program to improve child social, emotional and/or behavioral functioning. Given the recent rises in mental health needs reported in children, targeted behavioral-and/or cognitive behavior therapy-based interventions should be made widely available to children (and their families) who experience elevated symptoms.
Similar content being viewed by others
Mental health disorders are common in children and consequently pose a major public health burden. One epidemiological study estimated 12-month prevalence of mental health disorders for 4–11 year olds at 13.6%, the most common class of disorders being attention deficit and hyperactivity disorder (ADHD) and anxiety disorders (Lawrence et al., 2016). Indeed, childhood behavioral and emotional disorders greatly impact children’s overall wellbeing and are responsible for significant years lost due to disability (Guthold et al., 2021). Stemming from a misconception that mental disorders do not onset until adolescence, impairment and distress in children are often ignored and overlooked. Despite advances in research and clinical service provision, there has been little population level reduction in the prevalence of mental health disorders in young people over recent decades (Sawyer et al., 2018).
One approach to reducing the incidence and burden of childhood mental health disorders is through the identification of children who experience elevated symptoms and delivery of targeted interventions designed to reduce symptoms. Interventions, delivered early in the individual’s life and illness course, can be viewed as both prevention and treatment. For children with subclinical symptoms, targeted interventions can be classified as prevention (more specifically, indicated prevention), because they are delivered before the onset of a disorder (Mrazek & Haggerty, 1994), serving to prevent symptoms from developing into a clinical disorder. They can also have a preventive effect on disorders that the child would otherwise have developed later in childhood, adolescence, or adulthood. For children with elevated symptoms severe enough to warrant a diagnosis, interventions serve as treatment for existing clinical symptoms, as well as prevention for future disorders yet to develop.
Existing reviews of the efficacy of targeted interventions for children tend to have applied a narrow focus on specific domains, such as externalizing symptoms, rather than being inclusive of a broad range of mental health problems that may emerge in childhood. Further, reviews to date have not focused on younger children specifically (i.e., 4–9 years)—an important developmental period when children first transition to formal schooling. This period provides a key window for the detection of early social, emotional, and behavioral problems, and the delivery of effective early intervention. Indeed, there are many mental health interventions delivered in schools that are targeted to young children, yet not all programs are evidence-based (Laurens et al., 2022), perhaps representing the lack of literature on evidence-based interventions for younger children specifically.
As such, the aim of this study was to evaluate the efficacy of a range of interventions designed for children 4–9 years covering mental health difficulties broadly, as well as shared mechanisms and disorder-specific interventions. Broad-based interventions alone aggregate effects across various mental health difficulties by targeting shared mechanisms or general distress which may not provide a sufficient dose to address specific mental health concerns. Reviewing targeted programs for mental health difficulties more broadly, along with programs that target shared mechanisms, and disorder-specific difficulties may allow decision-makers to flexibly adapt interventions to various mental health needs.
Specifically, this review aimed to evaluate the efficacy of early interventions including both indicated preventions and treatments designed for children aged 4–9 years covering: broad mental health problems; internalizing symptoms; externalizing symptoms; anxiety; depression; mental health symptoms related to exposure to trauma; symptoms of attention-deficit/hyperactivity, and mental health symptoms related to autism spectrum disorder. Due to the enormity of this literature, we chose to conduct a systematic review of existing systematic reviews and meta-analyses. The objective was to identify evidence-based approaches, which may be used to assist schools and governments in making decisions about mental health programs. We chose to evaluate interventions targeted at young children aged 4–9 years (and their parents), as this represents a key developmental period of early schooling, for delivery by health and education professionals. Furthermore, we conducted an exploratory narrative synthesis of moderators when available within the texts. To increase the relevance of the findings to practitioners, we engaged an implementation partner, the NSW Department of Health, a state government department responsible for delivering mental health programs in primary schools within one state in Australia.
Methods
Search Strategy
A review of the English-language, peer-reviewed published literature was conducted and included reviews published over the last 23 years (January 2000–May 2023). The search identified systematic reviews and meta-analyses evaluating interventions for emotional, behavioral, and/or social problems in children aged 4- to 9-years. Reviews targeting a broader age range were included if the mean age fell within the 4–9 age range. We chose an iterative clinician-led process to shape the search terms to ensure the review included interventions used by the clinicians in community practice. This made registration of the review impossible as data extraction needed to take place to inform each consultation prior to finalizing the final search strategy.
Databases Searched
We searched seven electronic databases (PsycInfo, PubMed, Cochrane Library, CINAHL, ERIC, Family and Society Studies Worldwide, and Violence and Abuse Abstracts). The search terms were developed by identifying terms and synonyms corresponding to a range of common mental health problems in children. Mental health problems were defined broadly to include anxiety, obsessive compulsive disorder (OCD), depression, suicide/self-harm, conduct problems, sleep problems, emotion dysregulation, ADHD, social skills problems, attachment problems, childhood trauma, sensory regulation, or social-emotional wellbeing. We did not include interventions that were specifically designed to target Autism Spectrum Disorder (ASD) unless they targeted any of the above mental health problems specifically in children with ASD. Mental health terms were combined with terms and synonyms for “interventions.” Additional search terms were included to ensure a sensitive inclusion for programs also designed for First Nations communities. The searches were restricted to meta-analyses and systematic reviews and to populations of, or including, children aged 4- to 9-years. The detailed search strategy is provided in Supplementary Materials 1. The detailed inclusion and exclusion criteria are provided in Supplementary Material 2.
To ensure that the inclusion criteria and databases aligned with the needs of health professionals, the methods including search terms, databases and inclusion exclusion criteria were informed, reviewed, and approved by a Clinical Advisory group (Beames et al., 2021). The group was made up of a range of allied health professionals with experience delivering mental health interventions to children with social, emotional and behavioral problems in the first three years of school. The Clinical Advisory group conducted fortnightly consultations to determine the best scope of this review, integrating their experience with current mental health programs delivered in this age group.
Screening
Screening was completed on Covidence (https://www.covidence.org/). The titles and abstracts of the articles initially identified by the searches were screened to determine their relevance to the review. At this stage, irrelevant articles were excluded. Two members of the research team independently completed title and abstract screening on the remaining articles. The interrater reliability for title and abstract screening was moderate (κ = 0.62). Any discrepancies were resolved via discussion. The full text for each retained article was then examined according to the inclusion/exclusion criteria. One member of the research team completed full text review. A second member of the research team checked all excluded full text articles to ensure agreement on exclusion criteria. When disagreement about inclusion or exclusion occurred, consensus was reached through additional review and discussion. Interrater reliability for full-text screening was substantial (κ = 0.80).
Data Extraction
The following data was extracted for each review: citation, target of intervention (e.g., externalizing symptoms), intervention type (e.g., behavioral-based parent training), number of studies included, design of studies included (e.g., randomized controlled trials), total number of participants, age of participants, evidence statement, review design (e.g., systematic review). One member of the research team conducted data extraction. All extracted data was checked by another member of the research team and discrepancies discussed. Data were extracted in Covidence and downloaded to Excel.
Quality Appraisal
GRADE was used to assess the quality of evidence for each included review (Guyatt et al., 2008, 2011). Four levels of quality make up the GRADE score, with a ‘very low’ score meaning the true effect is different from that found in the research presented; and a ‘high’ score meaning that there is greater confidence in the findings presented in the research. For each article, individual GRADE scores are provided in Table 1 and a written rationale for that score in Table 2. All GRADE scores were checked by another member of the research team.
Data Synthesis
Findings were tabulated as a function of mental health problem (Table 1). Given the heterogeneity of interventions and outcomes, an overall quantitative synthesis was determined to be not possible or valid. A narrative synthesis was then undertaken, with findings synthesized according to the mental health problem and intervention type. The size of treatment effects for specific problems or interventions were described when available (small, moderate, large).
Results
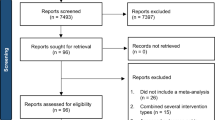
A total of 41,061 abstracts were retrieved, and of these 152 articles met the inclusion criteria (Fig. 1). The findings were evaluated according to interventions targeting the following: broad mental health needs, internalizing symptoms, externalizing symptoms, anxiety, depression, trauma, ADHD and ASD. Reviews within each symptom domain were categorized based on the types of interventions evaluated. Of the 152 included reviews, 48 received a high GRADE, 2 received a moderate/high GRADE, 57 received a moderate GRADE, 7 received a low to moderate GRADE, 25 received a low GRADE, and 13 received a very low GRADE (see Table 2) for GRADE score reasonings.
Characteristics of Included Studies
Most reviews (κ = 101) were meta-analyses, whilst the remaining 51 were systematic reviews. The total number of studies included in the 101 meta-analyses varied (range = 5 to 197 studies). The total participant sample size was variable (range = 12 to 56,620 participants per review; although 6 meta-analyses did not report sample size), as was the age range (range = 0 to 32 years).Footnote 1 The number of studies included in the 51 systematic reviews was also variable (range = 2 to 180 studies). The total number of participants ranged from 55 to 5,759 (12 did not report the total number). Within the systematic reviews, the age range varied from 0 to 21 years (Table 1).
Summary of Evidence by Intervention Type
Interventions for Mental Health Symptoms
A total of 28 reviews of interventions for a broad range of mental health symptoms were identified. These 28 reviews largely represented interventions aimed at improving various broad mental health symptoms, including emotional, social, and behavioral symptoms. Despite that, sometimes measures of specific symptoms were also included (e.g., depression) and we have reported these findings alongside those for broad mental health symptoms.
Mixed Psychosocial Interventions for Mental Health Symptoms
Three meta-analyses examined the efficacy of mixed psychosocial interventions in reducing a constellation of mental health problems (emotional, behavioral, social) in children (Pilling et al., 2020; Sanchez et al., 2018; Schleider & Weisz, 2017), with significant small to moderate pooled effect sizes reported. These papers were rated as being of moderate (Pilling et al., 2020) and high quality (Sanchez et al., 2018; Schleider & Weisz, 2017). A large scale meta-analysis conducted by Pilling et al., (2020) found that psychological interventions overall (including a range of treatments like CBT, psychoeducation, and behavioral-based parenting training) conducted in a range of clinical, community, and school settings lead to moderate effects on improving mental health symptoms in children, with effects retained at 12-month follow-up. Similarly, Schleider and Weisz (2017) highlighted in their meta-analysis that single session psychosocial interventions were efficacious for treating some mental health problems, specifically anxiety and conduct problems in young children in mostly clinical settings; though effects were not retained at 13-week follow-up. Behavioral interventions demonstrated a large effect, whereas non-behavioral interventions (e.g., attention bias modification, “growth mindset”) showed small effects. Both meta-analyses showed less (smaller effect sizes) or no (non-significant) efficacy for the use of these mixed psychosocial programs in the treatment of depressive symptoms (Pilling et al., 2020; Schleider & Weisz, 2017). Lastly, Sanchez et al. (2018) reported in their meta-analysis that school-based generic mental health programs similarly were associated with small to medium effect sizes with larger effect sizes for externalizing symptoms (medium effect sizes) compared to internalizing symptoms and attention problems. Taken together, these three moderate to high quality reviews suggest that generic psychosocial interventions overall are efficacious for child mental health symptoms, with smaller effects for depression and internalizing difficulties.
Regarding moderators, the meta-analyses found that younger children benefited more than older children from single-session interventions (Schleider & Weisz, 2017), and tended to do better following psychological interventions at follow up (Pilling et al., 2020). Pilling et al. (2020) emphasized that interventions were generally as effective in school as other settings when outcomes were compared 1-year after the intervention. Furthermore, the efficacy of anxiety and depression interventions (at 1-year follow-up) was similar when conducted by paraprofessionals or professionals. However, interventions led by paraprofessionals were less effective for treatment of conduct problems when compared to interventions led by professionals, and group programs were associated with negative 1-year outcomes. Beyond this, Sanchez et al. (2018) found that targeted intervention and selective prevention programs led to high-medium to large effects (and these were larger than the small effects observed following universal prevention).
Behavioral-Based Parenting Interventions for Mental Health Symptoms
A total of four meta-analyses (Buchanan-Pascall et al., 2018; Carr et al., 2017; Savaglio et al., 2023; Sheridan et al., 2019), and four systematic reviews (Bayer et al., 2009; Everett et al., 2021; Shucksmith et al., 2010; Zarakoviti et al., 2021). evaluated parenting interventions for a range of mental health symptoms in children. Most interventions were rated of moderate to high quality, except for Carr et al. (2017), which was rated as low to moderate quality. A meta-analysis by Savaglio et al., (2023) found the largest evidence base for parenting-focused programs for internalizing and/or externalizing disorders. Furthermore, a systematic review by Everett et al. (2021) denoted those interventions that targeted parenting behavior led to improvements in both child outcomes, as well as parental psychopathology and parental behavior.
Regarding intervention types, one systematic review concluded that the four parenting programs that were considered effective for managing behavioral problems for school-aged children include the Good Behavior Game, Incredible Years, John Hopkins Prevention Program and Parenting Through Change Program (Bayer et al., 2009). For pre-school aged children’s behavioral problems, Incredible Years, Triple P, and the US Family Check-up were found to be the most efficacious. Subsequently, regarding emotional problems, Bayer et al. (2009) found that The Parent Education Program and The Brief Psycho-educational Group-Based Program were the most efficacious for pre-school aged children, and Fast Track for school-aged children.
Four reviews, including three meta-analyses and one systematic review, found that parenting and family-based programs significantly reduced internalizing and externalizing problems in both clinical and community settings (Buchanan-Pascall et al., 2018; Carr et al., 2017; Savaglio et al., 2023; Zarakoviti et al., 2021). The benefits of family-based group behavioral interventions extended to school settings, with two studies showing efficacy for improving social-behavioral competence (e.g., prosocial skills, peer-relationships, self-regulation, externalizing problems) and mental health symptoms (Sheridan et al., 2019; Shucksmith et al., 2010). However, irrespective of setting, there were overall fewer studies but also smaller effect-sizes, or non-significant findings in managing internalizing symptoms compared to externalizing symptoms (Bayer et al., 2009; Buchanan-Pascall et al., 2018; Sheridan et al., 2019).
Consistent moderators of efficacy were identified across systematic reviews conducted in clinical or community settings, including stronger effects for families with children with less severe problems and for externalizing problems (Buchanan-Pascall et al., 2018; Carr et al., 2017; England-Mason et al., 2023). Regarding other moderators, while Carr et al. (2017) highlighted stronger effects for younger children in clinical and community settings, Sheridan et al. (2019) showed no differential age effects in school-based settings. Mixed findings were also found for duration of treatment, with some showing that longer treatments were more effective (Carr et al., 2017) and others highlighting that number of session hours did not impact outcome (Buchanan-Pascall et al., 2018).
Child-Centered Play Therapy for Mental Health Symptoms
Four reviews examined mental health and related outcomes following child-centered play-based therapy, with one meta-analysis reviewing case-studies (Pester et al., 2019), one meta-analysis evaluating a range of controlled trials (Bratton et al., 2005), and one systematic review and one meta-analysis evaluating mixed methods designs (Ledford et al., 2023; Money et al., 2021). Studies on play therapy were rated as very low to low/moderate in quality. Two meta-analyses reported small to large effect sizes of child-centered play therapy for various mental health outcomes (Bratton et al., 2005; Pester et al., 2019) and social skills (Ledford et al., 2023). Consistently, play therapy led to improvements in internalizing and externalizing symptoms (Bratton, 2005; Money et al., 2021; Pester et al., 2019). Pester et al. (2019) also found small to moderate effect-sizes for social skills, but play therapy was not effective for improving self-regulation skills.
Socio-Emotional Interventions for Mental Health Symptoms
A total of five systematic reviews and three meta-analyses (Bauer et al., 2021; Blewitt et al., 2021; Dalgaard et al., 2022; England-Mason et al., 2023; Jugovac et al., 2022; Law et al., 2012; Sprung et al., 2015; Sun et al., 2021) investigated the effect of interventions targeting socio-emotional aspects of child mental health, with mixed evidence. One moderate quality meta-analysis examined the effects of programs delivered in a range of settings (including outpatient clinics and school settings) focusing on improving children’s understanding of emotions (recognizing, understanding and reflecting upon emotions) (Sprung et al., 2015). These researchers reported small to moderate effect-sizes in improving emotional competence across these three domains, with longer treatments associated with stronger effects. Furthermore, a recent high quality meta-analysis by England-Mason et al. (2023) found that parenting interventions that focused on emotion socialization were also effective for improving aspects of internalizing and externalizing symptoms, including child emotional competence and behavioral adjustment.
Two studies investigated attachment-based intervention programs. One high quality meta-analysis by Jugovac et al. (2022) found that attachment and emotion-focused parenting interventions led to improvements in internalizing and externalizing disorders, with larger effects for internalizing disorders. However, this result is not consistent across studies, as a systematic review by Dalgaard et al. (2022) found that attachment-based interventions led to a slightly greater effect for externalizing disorders rather than internalizing disorders for children with foster and adoptive parents.
Beyond this, two systematic reviews evaluating social and emotional learning programs found that they led to improvements in various social-emotional outcomes (Blewitt et al., 2021; Sun et al., 2021), though the quality of these studies were low to moderate. Blewitt et al. (2021) found that social and emotional learning programs overall improved social competence but had mixed evidence on behavioral regulation and led to non-significant differences in emotional competence. Sun et al. (2021) evaluated yoga and mindfulness-based interventions on social-emotional learning and found positive results in behavioral regulation, emotion regulation, and social skills. There was evidence for three other programs targeting social support, social skills, and communication skills specifically, but quality for these papers were low (Bauer et al., 2021) and very low (Law et al., 2012). Bauer et al. (2021) found that interventions aimed at mobilizing social support led to improvements in child behavior, cognitive and social development outcomes, coping, and psychological functioning, with small effect sizes. Law et al. (2012) also found overall positive results for behavioral interventions targeting communication difficulties, but results are limited by study quality.
Regarding potential moderators, Sprung et al. (2015) found that whereas improvements in external emotional competency were more often found when the program was delivered in group settings, improvements in reflective emotional understanding were more likely found for individually delivered programs. Environmental setting (e.g., classroom, area in school, lab) also moderated results. Children with lower baseline social-emotional functioning also demonstrated greater improvements (Sun et al., 2021).
Art Therapy for Mental Health Symptoms
Three systematic reviews examined art-based therapies conducted with primary age children (5 to 12 years) in school settings, reporting some small but significant effects on some mental health outcomes (McDonald & Drey, 2018; Moula, 2020; Moula et al., 2020). One review reported significant positive improvements in reducing defiant behavior and separation anxiety symptoms but not for locus of control (McDonald & Drey, 2018). Two other reviews showed significant improvements in self-esteem and aggression but small changes in depression, anxiety, attention and withdrawal (Moula, 2020; Moula et al., 2020). However, these results are provisional due to a small number of trials included in these reviews and the low to moderate quality of these studies.
Positive Psychology Interventions for Mental Health Symptoms
One systematic review investigated the effect of positive psychology interventions on broad child mental health symptoms (Benoit & Gabola, 2021). Positive psychology interventions were shown to have mixed benefits on child wellbeing, including non-significant or positive results for change in positive emotions and engagement and improvements in prosocial behavior but non-significant changes in teacher–child relationships. However, positive psychology interventions did show benefits on quality of life and life satisfaction in two studies. Importantly, conclusions are limited due to the small number of studies meeting inclusion criteria (n = 3) and the subsequent low-quality appraisal of this review.
Interventions for Children with Internalizing Symptoms
We identified two meta-analyses which evaluated the efficacy of interventions in managing internalizing symptoms in children. These two meta-analyses are discussed below.
Mixed Psychosocial Interventions for Internalizing Symptoms in Children
One meta-analysis of moderate quality evaluated the efficacy of a range of psychosocial interventions in managing internalizing symptoms in children, with small effect sizes at post-intervention and follow-up reported (Yap et al., 2016). A significantly better, albeit small effect size was found for selective relative to universal interventions.
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Internalizing Symptoms in Children
One high quality meta-analysis evaluated the efficacy of CBT interventions in reducing internalizing symptoms in children and reported a large, within-group effect size post-therapy and at follow-up (Sun et al., 2019). Interventions which included parental involvement contributed to a significantly larger effect size, whereas age, treatment mode (individual vs. group), goal setting or length did not moderate treatment efficacy.
Interventions for Children with Externalizing Symptoms
We identified 44 reviews which evaluated the efficacy of interventions in managing externalizing symptoms only in children. These reviews are discussed below.
Mixed Psychosocial Interventions for Externalizing Symptoms in Children
A total of 11 reviews (seven meta-analyses and four systematic reviews) of mostly moderate to high quality examined mixed psychosocial interventions for externalising symptoms (Bakker et al., 2017; Barlow & Stewart-Brown, 2000; Battagliese et al., 2015; Burkey et al., 2018; Comer et al., 2013; Connor et al., 2006; Fossum et al., 2008, 2016; Lane et al., 2023; Stoltz et al., 2012; Tse, 2006). Of these studies, quality was lower for Lane (2023) and Tse (2006), which were rated low. Meta-analyses showed that behavioral-based interventions had greater efficacy than non-behavioral-based interventions (Comer et al., 2013; Fossum et al., 2008, 2016). However, meta-analyses which examined interventions that included behavioral and non-behavioral elements still revealed small to moderate effect-sizes for externalizing symptoms (Bakker et al., 2017). Beyond this, one meta-analysis also found that personalized interventions led to a slightly greater improvement in child conduct problems compared to non-personalized interventions, as measured through the ECBI Problem Subscale in the short term, but not for other outcome measures (Lane et al., 2023). However, conclusions are limited as the study was considered low quality. Three systematic reviews evaluated the efficacy of a mixed array of psychosocial interventions for managing externalizing symptoms in children (Barlow & Stewart-Brown, 2000; Connor et al., 2006; Tse, 2006). Collectively, the findings from these reviews supported the small to moderate effect sizes documented in the meta-analyses.
There were inconsistent findings in the reviews about the moderating impact of age (Burkey et al., 2018; Comer et al., 2013; Fossum et al., 2016) and the involvement of children on outcome (Battagliese et al., 2015; Comer et al., 2013). Individual, compared to group interventions demonstrated greater reductions in conduct problems in one review (Fossum et al., 2016) but not in another (Comer et al., 2013). For young children, individual psychosocial interventions delivered at school were more beneficial for reducing disruptive behavior when combined with additional classroom and/or school-wide interventions (Stoltz et al., 2012).
Behavioral-Based Parenting Interventions for Externalizing Symptoms in Children
For externalising disorder interventions, parenting treatments had the strongest evidence. We identified 22 meta-analyses, three systematic reviews, and one meta-meta-analysis, that evaluated behavioral-based parenting interventions. Commonly evaluated interventions included: Incredible Years (Forster et al., 2012; Furlong et al., 2012; Gardner et al., 2019a, 2019b; Leijten et al., 2013, 2016, 2018, 2020; Menting et al., 2013), Parent Child Interaction Therapy (Forster et al., 2012; Leijten et al., 2013), and Triple P (de Graaf et al., 2008; Forster et al., 2012; Leijten et al., 2013, ; Nogueira et al., 2022; Tully & Hunt, 2016). More broad-based psychoeducational or behavioral skills-based programs were also evaluated (Cai et al., 2022; Dretzke et al., 2005, 2009; Maughan et al., 2005). Most reviews on parenting treatment were of moderate to high quality, with the exception of one review rated low to moderate quality by Gardner et al. (2019a, 2019b). On average, small to moderate effect-sizes were reported (Cai et al., 2022; de Graaf et al., 2008; Dretzke et al., 2005, 2009; Forster et al., 2012; Furlong et al., 2012; Gardner et al., 2019a, 2019b; Leijten et al., 2013, 2016, 2018, 2020; Maughan et al., 2005; Menting et al., 2013; Mingebach et al., 2018), which were maintained at follow-up (Cai et al., 2022; de Graaf et al., 2008; Leijten et al., 2018). Notably, one meta-analysis, which focused solely on evaluating Parent Child Interaction Therapy, reported a large effect size in improving child behavior (Ward et al., 2016). Another meta-analysis, which evaluated a range of parenting interventions, also reported large effect sizes for Parent Child Interaction Therapy and reported small to moderate effect sizes for both Incredible Years and Triple P (Leijten et al., 2016). Furthermore, the effectiveness of behavioral-based parenting interventions extended to foster families, as demonstrated in two meta-analyses, in which effect sizes were found to be small to moderate when interventions were delivered to foster carers (Solomon et al., 2017; Uretsky & Hoffman, 2017).
Some moderators of efficacy were identified across these meta-analyses. Two reviews found that children with greater symptom severity showed greater improvement following intervention (de Graaf et al., 2008; Leijten et al., 2020) and two found stronger effect sizes in treatment, rather than prevention, trials (Gardner et al., 2019a, 2019b; Leijten et al., 2018; Menting et al., 2013). One review reported stronger effect sizes the greater the number of therapy sessions attended (Menting et al., 2013); another found that male children did better at follow-up (de Graaf et al., 2008), while another found that disadvantaged families showed less benefit by one-year follow-up (Leijten et al., 2013). However, age, delivery format (individual vs. group) and provider were not found to moderate efficacy of the programs delivered on child outcomes (Cai et al., 2022; de Graaf et al., 2008; Gardner et al., 2019a, 2019b).
The findings of the systematic reviews generally supported those of the meta-analyses. One systematic review focused on evaluating brief (< 8 sessions), behavioral parent training programs (such as Triple P and Parent Management Training Oregon) (Tully & Hunt, 2016). The researchers noted that all eight studies reported significant improvements in parent ratings for externalizing symptoms in children, with small to large effect sizes found for these programs. Another systematic review evaluated predictors of efficacy of behavioral-based parenting programs (including Incredible Years, Parent Child Interaction Therapy and Triple P) and reported some evidence for better outcomes in families with more positive child-parent relations (Dedousis-Wallace et al., 2021).
In addition to face-to-face behavioral parent training, three meta-analyses and one systematic review demonstrated that digitally assisted parent training (including self-directed parent training) (Tarver et al., 2014) was effective. Effect sizes ranged from small to moderate (Baumel et al., 2016 and 2017; Florean et al., 2020; Thongseiratch et al., 2020; Tarver et al., 2014) and gains were maintained at follow-up (Baumel et al., 2016). Stronger effect sizes were observed with a greater number of sessions (Florean et al., 2020), children’s difficulties being in the clinical range at baseline (compared to non-clinical children in middle school; Baumel et al., 2016), the inclusion of interactive elements in the digital treatment (compared to non-interactive digital treatment; Baumel et al., 2016), and sending reminders to parents/carers (Thongseiratch et al., 2020).
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Externalizing Symptoms in Children
One moderate to high quality meta-analysis evaluated the efficacy of CBT, behavioral therapy and/or cognitive therapy interventions in managing externalizing symptoms and found a large effect size which was retained at follow-up (Riise et al., 2021). The interventions examined in this meta-analysis included behavioral-based parenting programs such as Incredible Years and PCIT, in addition to other forms of behavioral, cognitive, and/or cognitive behavioral intervention delivered directly with the child. The effect size did not differ as a function of therapy format (individual vs. group) or degree of parent, teacher and/or professional involvement. However, younger children (mean age = 8.2 years) and those with greater baseline symptoms showed greater improvement.
Behavior-based interventions were also found to be effective in reducing externalizing symptoms when delivered in a school setting in two meta-analyses and one systematic review (Nye et al., 2019; Smith et al., 2021; Veenman et al., 2018). These three reviews were of moderate to high quality. Two meta-analyses reported small to moderate effect sizes for behavioral-based classroom programs (Smith et al., 2021; Veenman et al., 2018), whilst a systematic review of the Incredible Year Teacher Classroom Management intervention indicated a moderate effect size (Nye et al., 2019). Length of treatment was related to outcome, such that briefer classroom interventions were found to be more effective (Veenman et al., 2018). Mixed results were found on the moderating effect of gender, including having no significant impact (Veenman et al., 2018), or behavioral-based programs being more effective in girls than boys (Smith et al., 2021). Conversely, age and severity of problems were not related to outcome (Veenman et al., 2018).
Child-Centered Play Therapy for Externalizing Symptoms in Children
One moderate quality meta-analysis (Parker et al., 2021a, b) found that child-centered play therapy led to reductions in externalizing and overall problem behaviors with medium effects. There were also reductions in aggressive behaviors, with small effects.
Child Social Skills Training for Externalizing Symptoms in Children
One high quality meta-analysis (Lösel & Beelmann, 2003) revealed that social skills interventions (predominately, but not exclusively, based on behavioral and/or cognitive model of social learning), yielded small to moderate effect sizes on antisocial behavior, with small effects maintained at follow-up. Social skills programs targeting at-risk children were found to be more effective than universal interventions.
Music Interventions for Externalizing Symptoms in Children
One moderate quality meta-analysis evaluated group-based music intervention and reported a large effect-size in reducing aggressive behaviors and a moderate effect-size in increasing self-control (Ye et al., 2021). However, children less than 10 years benefited less than older children, while more than one music session per week resulting in greater benefit than less frequent sessions.
Interventions for Children with Anxiety and Related Disorders
There were 18 reviews reporting on interventions targeting anxiety and/or related disorders/symptoms. These are evaluated below.
Mixed Psychosocial Interventions for Children with Anxiety and Related Disorders
Five meta-analyses and one systematic review reported on a wide range of psychosocial interventions for anxiety symptoms in children (Caldwell et al., 2019; Comer et al., 2019; Grist et al., 2019; Reynolds et al., 2012; Werner-Seidler et al., 2017, 2021). Four of the five meta-analyses were considered high quality, and one meta-analysis (Caldwell et al., 2019) was of moderate quality. Four out of five meta-analyses reported small to moderate effect sizes, demonstrating a positive impact of psychosocial interventions for children. Smaller effects were observed when interventions were compared to active control conditions and at follow-up. One meta-analysis did not find psychosocial interventions had any significant effect on anxiety following universal or targeted interventions delivered in primary schools (Caldwell et al., 2019). This review did report some, albeit weak, evidence in support of the efficacy of universal CBT interventions for reducing student anxiety. In further support of this effect, two additional reviews reported that CBT delivered stronger effects (moderate effect sizes) compared to non-CBT interventions (Grist et al., 2019; Reynolds et al., 2012). Results from one systematic review similarly concluded that CBT treatments were the only interventions that were probably efficacious to well-established (Comer et al., 2019). Individual interventions (vs group) and greater treatment length were both associated with stronger effects (Reynolds et al., 2012). Therapist assisted (vs self-help) and parental involvement increased effects of interventions (Comer et al., 2019; Grist et al., 2019).
Behavioral-Based Parenting Interventions for Children with Anxiety
One low quality meta-analysis investigated Parent–Child Interaction Therapy (PCIT) on youth anxiety and found that PCIT was effective at reducing anxious symptoms, with large effect sizes (Phillips & Mychailyszyn, 2021). PCIT was effective regardless of single diagnosis or comorbid diagnoses, and regardless of clinical status. The inclusion of family is also shown to be effective for cases of selective mutism, with one meta-analysis showing that combined behavioral and family systems approaches have the most supporting evidence for selective mutism (Steains et al., 2021).
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Children with Anxiety and Related Disorders
Seven meta-analyses of moderate to high quality evaluated CBT-based interventions. One review solely focused on evaluating age effects and no significant differences emerged, concluding that CBT was effective in reducing anxiety symptoms across development (Bennet et al., 2013). The other six meta-analyses found that CBT significantly reduced anxiety symptoms in children (Ale et al., 2015; Fisak et al., 2011; Howes Vallis et al., 2020; McGuire et al., 2015; Viswanathan et al., 2022; Yin et al., 2021). Only one meta-analysis reported small effect-sizes (Fisak et al., 2011), while the other five reported moderate to large effect sizes on average. Beyond these meta-analyses, one low quality systematic review demonstrated that these findings provisionally extend to children with selective mutism, concluding that CBT is ‘promising’ in reducing anxiety symptoms in these children (Østergaard, 2018).
Regarding moderators of efficacy, two meta-analyses showed no difference in effects based on parental attendance at sessions (Ale et al., 2015; Howes Vallis et al., 2020); two showed no effect of intervention duration (Ale et al., 2015; Fisak et al., 2011); two showed no difference between individual and group formats (Ale et al., 2015; Howes Vallis et al., 2020); and, one showed no difference between universal compared to targeted CBT interventions (Fisak et al., 2011). Two moderators were identified: (i) CBT interventions administered by professionally qualified mental health providers had significantly better effects relative to minimal effects for interventions administered by laypersons (Fisak et al., 2011), and, (ii) in-person CBT interventions had significantly stronger effects than internet-based CBT interventions in young children (mean age = 5.45 years; Howes Vallis et al., 2020).
In terms of CBT components/types, Ale et al. (2015) found that CBT interventions that explicitly included exposure and response prevention for OCD had significantly stronger effects relative to other types of CBT interventions for other types of anxiety disorders (Ale et al., 2015). Exposure-based interventions also exhibited larger effects compared to cognitive therapies for OCD, although this effect was not statistically significant (McGuire et al., 2015). Finally, there was some conflicting evidence for the efficacy of cognitive bias modification interventions in reducing anxiety in children. One review reported a significant, yet small effect-size for reducing anxiety symptoms (Krebs et al., 2018), while another reported a minimal, non-significant effect-size for a very small number of trials (Grist et al., 2019).
Mindfulness Interventions for Children with Anxiety and Related Disorders
One moderate quality meta-analysis investigated the efficacy of mindfulness-based interventions on anxiety for children (Odgers et al., 2020). A small effect-size was reported overall, with the meta-analysis pooling the results from a small number of studies conducted in Iran that produced a significantly larger effect-size relative to studies conducted in Western countries, where the effects were found to be non-significant. This review does not support the use of mindfulness interventions for the reduction of anxiety in children.
Interventions for Children with Depressive Symptoms
Seven reviews reported on a range of interventions targeting depressive symptoms in children. These are evaluated below.
Mixed Psychosocial Interventions for Children with Depressive Symptoms
Five meta-analyses of moderate to high quality reviewed a range of psychosocial interventions for depression: two reported small but significant effect sizes (Werner-Seidler et al., 2017, 2021) and one failed to find any effect at post treatment for school-based interventions (Caldwell et al., 2019). However, Caldwell and colleagues (2019) did find that between 13 and 24 months follow-up, CBT-based targeted programs led to significant reductions in depressive symptoms, with a moderate effect-size. One meta-analysis examined response rates instead of effect sizes and Cuijpers et al. (2023) found that 39% of youth responded to treatment compared to 24% response rates in controls. However, of those that did respond, effects of response retained at 6–12 months. In further support of the medium-term effects, Werner-Seidler et al., (2017, 2021) also found that effects of school-based programs, predominantly comprising CBT components, were also evident at 12 months follow-up, although the effect-size was smaller.
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Children with Depressive Symptoms
One low quality meta-analysis comprised a range of CBT programs, including computerized interventions, self-control therapy, and CBT combined with pharmacotherapy (Forti-Buratti et al., 2016). The authors reported non-statistically significant effects when CBT programs were compared to waitlist/no treatment conditions, showing a lack of evidence for CBT in successfully treating depression in children younger than 13 years of age. Conversely, another high quality review evaluated the efficacy of a range of psychotherapy programs, predominantly CBT, in managing depression in children and reported a moderate to large effect-size, which was retained at follow-up (Michael & Crowley, 2002). Larger effects were observed for adolescents older than 12 years of age compared to younger children. A low quality systematic review of psychotherapy programs for children with dysregulated mood showed some, albeit limited and preliminary, evidence of symptom improvement following psychological intervention (Benarous et al., 2017).
Interventions for children exposed to trauma
Eight reviews investigated the efficacy of interventions for children exposed to trauma. These are evaluated below.
Psychosocial Interventions for Children Exposed to Trauma
Three meta-analyses investigated the efficacy of psychosocial interventions on a range of trauma symptoms. Collectively, two high quality meta-analyses showed efficacy of interventions (including trauma-focused CBT and eye movement desensitization and processing) relative to control on symptoms of post-traumatic stress disorder (PTSD) (Bastien et al., 2020; Purgato et al., 2018), and one moderate quality meta-analysis demonstrated efficacy relative to control for bereavement and total mental health (Rosner et al., 2010) and in low-resource humanitarian settings (Purgato et al., 2018). The meta-analysis by Purgato et al. (2018) further showed that these small to moderate effects were retained at follow up. However, while efficacious for PTSD symptoms, these interventions did not influence depression and anxiety symptoms relative to control groups (Purgato et al., 2018), with one study (the only one eligible for inclusion) in the meta-analysis conducted by Bastien et al. (2020) showing that trauma-focused CBT was no more efficacious than waitlist control for children. Nevertheless, most studies indicated small to moderate pooled effect sizes (Bastien et al., 2020). Moreover, the effectiveness of psychosocial interventions for trauma symptoms, specifically children with a history of neglect (no matter the severity), provisionally extended to children in foster care, but requires more rigorous evaluation in community-based settings (Hambrick et al., 2016).
Regarding moderators of efficacy, Purgato et al. (2018) indicated that psychosocial interventions were more effective for non-displaced (versus displaced) children and those from smaller households (< six people versus > six people). However, there were mixed findings regarding the impact of age on outcome, with Hambrick et al. (2016) showing that younger children benefited more from the interventions, while Purgato et al. (2018) and Rosner et al. (2010) indicating stronger effects for children over the age of 12 years.
Behavioral-Based Parenting Interventions for Children Exposed to Trauma
One moderate quality meta-analysis investigated trauma-informed behavioral-based parenting interventions (Lindstrom Johnson et al., 2018). Such interventions had a moderate to large effect on child trauma symptoms, as well as on positive parenting practices, child Internalizing problems and child Externalizing problems. The type of trauma impacted efficacy, with greater effect sizes observed for child maltreatment-focused interventions compared to interventions that focused on intimate partner violence or family conflict. Moreover, longer interventions showed a stronger effect on Internalizing problems. Interestingly, efficacy did not differ as a function of child involvement.
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Children Exposed to Trauma
One moderate quality systematic review examined trauma-focused cognitive-behavioral interventions (TF-CBT) for preschool children, aged 3- to 6-years (McGuire et al., 2021). The authors concluded that since few of the studies assessed efficacy in preschool children as well as the vast differences in treatment protocols for TF-CBT used with preschool aged children, TF-CBT is currently classified as “probably efficacious” intervention for preschool children. The authors also highlighted that when considering the use of TF-CBT for preschool-aged children with PTSD, clinicians must consider their cognitive abilities, family context and culture.
Child-Centered Play Therapy for Children Exposed to Trauma
Two systematic reviews focused on child-centered play therapy for children who have experienced trauma. One moderate quality systematic review found that child-centered play therapy was a promising intervention for children who experienced adverse childhood experiences, leading to reductions in externalizing and internalizing behavior and increases in parental empathy (Parker et al., 2021a). However, another low quality systematic review found that although some changes have been demonstrated pre-to post-intervention, this was not consistent across measurements and very few differences were demonstrated between treatment and control groups (Humble et al., 2019). Thus, the authors concluded that, presently, there is limited evidence to recommend child-centered play therapy for children who have experienced trauma.
Interventions for Children with Attention Deficit Hyperactivity Disorder (ADHD)
Overall, 35 reviews investigated the efficacy of interventions for ADHD symptoms. The bulk of the literature reviewed the efficacy of behavioral-based parenting interventions. The findings are summarized below.
Behavioral-Based Parenting Interventions for Children with ADHD
We identified six meta-analyses and seven systematic reviews that evaluated behavioral-based parenting interventions for children with ADHD. Most of these reviews evaluated a range of broad-based behavioral psychoeducational parent training interventions, and quality of reviews ranged from low to high. On average, the meta-analyses reported small to large effects in reducing ADHD symptoms, as well as comorbid externalizing and internalizing symptoms (Coates et al., 2015; Corcoran & Dattalo, 2006; Lee et al., 2012; Mulqueen et al., 2015; Rimestad et al., 2019; Zwi et al., 2011).
The findings of the systematic reviews were similar to the findings of the meta-analyses (Bjornstad & Montgomery, 2005; Ghuman et al., 2008; McGoey et al., 2002; Murray et al., 2018; Tan-MacNeill et al., 2021; Vacher et al., 2020; Vetter, 2018). Of note, systematic reviews were of low to moderate quality. Three systematic reviews evaluated specific interventions, namely Parent Child Interaction Therapy (PCIT) and the Incredible Years, showing they were efficacious for reducing parent and/or teacher reported ADHD symptoms (Ghuman et al., 2008; Murray et al., 2018; Vetter, 2018). One review evaluating various online parenting interventions also reported improvements in parent-rated ADHD symptoms overall (Tan-MacNeill et al., 2021). Two reviews also found beneficial effects on other child outcomes, such as social skills, emotion regulation and peer interaction (Murray et al., 2018; Vacher et al., 2020), and two reported improved parent–child interactions and parental confidence in managing child behavior (McGoey et al., 2002; Tan-MacNeill et al., 2021).
Notably however, one systematic review of low quality including two studies showed that a behavioral-based parenting intervention was not as effective as medication but did not differ from treatment as usual in the community (Bjornstad & Montgomery, 2005) and two indicated they were not efficacious when based on teacher reported ADHD symptoms (McGoey et al., 2002; Murray et al., 2018). Nevertheless, these authors concluded overall that behavioral-based parenting interventions had strong efficacy for some children and their families, and this depended on a number of moderating factors.
Some moderators of efficacy were considered across the meta-analyses and systematic reviews. Two meta-analyses showed no difference in efficacy depending on the delivery format of group vs individual (Lee et al., 2012; Rimestad et al., 2019), and two systematic reviews showed no differences depending on intervention duration and child involvement (Lee et al., 2012; Mulqueen et al., 2015). A systematic review focusing on the Incredible Years program showed there were no differences in effect sizes between studies that included the child-component and those that included the parent-component only (Murray et al., 2018). Notably however, one meta-analysis found that studies incorporating medication with behavioral based parenting interventions had significantly better effect sizes for ADHD symptoms than those without medication (Corcoran & Dattalo, 2006).
Behavioral, Cognitive, and Cognitive Behavioral Interventions for Children with ADHD
There were a total of 10 meta-analyses and one systematic review evaluating behavioral, cognitive and cognitive-behavioral interventions. Two recent high quality meta-analyses of RCTs investigated the efficacy of various behavioural treatments in ADHD (Groenman et al., 2022; Hornstra et al., 2023), demonstrating overall small to moderate improvements in ADHD symptoms, ODD and CD symptoms, and impairment (Groenman et al., 2022). Another moderate quality meta-analysis examined the efficacy of various behavioral interventions in managing ADHD that included parent, teacher and/or child sessions delivered across home, school and other contexts (Fabiano et al., 2009). A large effect size was reported. Behavior-based interventions were also found to be effective in reducing ADHD symptoms when delivered in a school setting in four very low to moderate quality studies (Gaastra et al., 2016; Harrison et al., 2019; Iznardo et al., 2020; Pyle & Fabiano, 2017). Two meta-analyses reported general improvements in outcomes for daily behavior report cards, with moderate to large effect sizes (Iznardo et al., 2020; Pyle & Fabiano, 2017). Two other meta-analyses showed behavioral interventions, instructional interventions and self-management interventions also had moderate efficacy. Mode of delivery was related to outcome, such that interventions implemented by a researcher were more effective than those implemented by a teacher (Harrison et al., 2019), and individual training led to larger effects than group training (Hornstra, 2023). Higher conduct or ADHD symptoms at baseline also led to greater intervention effects (Groenman, 2022). Notably, the addition of medication to behavioral-based interventions led to the largest effect sizes (Gaastra et al., 2016).
Other reviews have investigated specific behavioral interventions, including one moderate quality meta-analysis, which showed that behavior modification and neurofeedback interventions resulted in improvements in ADHD symptoms, such as hyperactivity, inattention, sociability and self-control (Hodgson et al., 2014). This effect was strongest for girls compared with boys, and for the combined subtype of ADHD compared with other subtypes. When examining the efficacy of cognitive behavioral interventions on ADHD and externalizing behaviors, Riise et al. (2021) found large but comparably smaller effects for ADHD than externalizing behaviors in a moderate to high quality study. Furthermore, Wilkes-Gillan et al. (2021) investigated video-modelling as an intervention technique for behavior change in ADHD. In this low/moderate quality review, Wilkes-Gillan et al. (2021) found overall improvements in social targets, such as social skills and friendship quality. Pauli-Pott et al. (2021) found in a high-quality meta-analysis that cognitive interventions targeting executive functioning led to positive outcomes on ADHD and ODD symptoms with small to moderate effect sizes in children with this dual diagnosis.
Mixed Psychosocial Interventions for Children with ADHD
One moderate quality meta-analysis, one high quality meta-meta-analysis, and one high quality systematic review evaluated the efficacy of psychosocial interventions on ADHD, but all three considered these in combination with medication (Arnold et al., 2015; Türk et al., 2023; Van der Oord et al., 2008). All three studies showed that psychosocial interventions were moderately efficacious in reducing ADHD symptoms, but when combined with medication larger effect sizes were achieved. Interestingly, two studies (Arnold et al., 2015; Van der Oord et al., 2008) showed that treatment duration did not influence the efficacy of combined psychosocial interventions with medication.
Child Social Skills Training for Children with ADHD
A meta-analysis conducted by Storebo et al. (2019) revealed that social skills interventions were associated with small to moderate effect sizes on teacher and parent reported ADHD symptoms, as well as on social skills, emotional competence, and general behavior. The meta-analysis by Storebo et al. (2019) was considered high quality. Two moderate quality systematic reviews similarly found child social skills training to be efficacious for ADHD (Fox et al., 2020; Willis et al., 2019).
Self-Regulation Interventions for Children with ADHD
ADHD was the only condition for which self-regulation interventions were specifically reviewed. One meta-analysis by Reid et al. (2005) on self-regulation interventions found that these interventions are efficacious for elementary age children (under 12 years of age) with ADHD. These interventions were conducted across a range of settings, including school, community, and clinic, and demonstrated efficacy in improving ADHD behaviors, such as an increase in on-task behavior and a decrease in inappropriate or disruptive behaviors. Notably, the findings reported by Reid et al. (2005) suggest that the effects of medication combined with self-regulation interventions may be more efficacious than the intervention or medication alone. However, conclusions should also be taken with caution as the quality of the review was considered low.
Child-Centered Play Therapy for Children with ADHD
Two small systematic reviews examined play-based interventions conducted by occupational therapists in school-based settings (Brooks & Bannigan, 2021; Cornell et al., 2018). Although both reviews reported positive intervention outcomes, including improved social play skills, empathy, and occupational performance, these interventions still cannot be considered an evidence-based practice for ADHD at the present time given an insufficient amount of high-quality evidence (Brooks & Bannigan, 2021; Cornell et al., 2018). Indeed, these reviews were rated as low (Brooks & Bannigan, 2021) and moderate (Cornell et al., 2018) quality.
Meditation and Mindfulness Interventions for Children with ADHD
One small systematic review on meditation for ADHD in the classroom found that there is insufficient evidence to support its efficacy for ADHD due to the limited number of RCTs conducted on this intervention type for children with ADHD and all reported inconsistent results (Krisanaprakornkit et al., 2010). Conversely, one meta-analysis by Vekety et al. (2021) denoted that mindfulness-based interventions reduced teacher-rated inattentive and hyperactive-impulsive behaviors with small effect sizes. However, these two reviews were also considered low to moderate quality. Overall, further evidence is required to understand the efficacy of meditation and mindfulness-based interventions (Krisanaprakornkit et al., 2010; Vekety et al., 2021).
Interventions for Children with Autism Spectrum Disorders (ASD)
Seventeen reviews investigated the efficacy of interventions for a range of emotional, behavioral or social problems in children with a diagnosis of ASD. These are evaluated below.
Behavioral-Based Interventions for Children with ASD
Two meta-analyses and one systematic review examined behavior-based interventions for children with ASD (Camargo et al., 2016; Tarver et al., 2019; Vetter et al., 2018). One high quality meta-analysis showed moderate effect-sizes following behavioral parent interventions on child disruptive behavior and hyperactivity (Tarver et al., 2019). Another meta-analysis showed that a broad range of behavioral-based interventions (incorporating prompting, modelling, reinforcement and imitation skills) were efficacious for improving social interaction skills in children with ASD, with similar gains across different age groups (Camargo et al., 2016). However, Camargo et al. (2016) had a low-quality rating, so interpretations should be cautious. Another low quality systematic review described nine non-controlled studies investigating the efficacy of Parent Child Interaction Therapy that had been extensively adapted for use with children with ASD (Vetter, 2018). Positive outcomes were reported for child problem behavior, ADHD-related disruptive behaviors, parental stress, parent–child interactions, and socialization.
Social Skills Interventions for Children with ASD
Ten reviews investigated social skills interventions for children with ASD. Six meta-analyses reported that social skills interventions led to positive outcomes with small to large effect-sizes (Reichow et al., 2013; Wahman et al., 2022; Whalon et al., 2015; Wang et al., 2011, 2013; Wang & Spillane, 2009). The only high quality meta-analysis evaluating RCTs provided evidence that social-skills groups improve social competence and friendship quality in this population (Reichow et al., 2013). The other five meta-analyses were of very low or low quality. Despite that, Whalon et al. (2015) demonstrated that children with ASD can benefit from social skills interventions implemented with peers in school settings, as well as from adult-mediated, child-specific and multi-component interventions, with large effect-sizes reported. One meta-analysis evaluated peer-mediated and video-modelling interventions, and concluded from 14 single case-studies that these interventions improved the social performance of children with ASD (Wang et al., 2011). Four systematic reviews of very low or low quality reported similar results that social skills interventions improved communication skills and parent–child interactions, with peer-related interventions for pre-school aged children with ASD showing generalization and maintenance of outcomes (Camargo et al., 2014; Gunning et al., 2019; Tan-MacNeill et al., 2021; Wright et al., 2016). Imitation interventions had inconsistent or non-significant effects (Tan-MacNeill et al., 2021).
Regarding notable moderators, there were mixed conclusions regarding the effect of age on the efficacy of social skills interventions. One meta-analysis of children aged 4- to 15-years reported that interventions were more efficacious for younger than older children (Wang et al., 2011). Conversely, two meta-analyses showed that age did not moderate outcomes with similar gains seen across the different age groups following intervention (Wang et al., 2013; Whalon et al., 2015).
Social Stories for Children with ASD
The two meta-analyses examining social stories yielded conflicting findings. A meta-analysis of single cases-studies demonstrated that social stories had low to questionable overall efficacy (Kokina & Kern, 2010). There was some evidence that stories were more efficacious when addressing inappropriate behavior than when teaching social skills to children with ASD, and when delivered to primary school age children (6- to 11-years) rather than younger children. In contrast, a second meta-analysis of case series designs reported a moderate effect-size and concluded social stories were efficacious interventions for reducing inappropriate and increasing appropriate social behavior in children with ASD (Aldabas, 2019). However, social stories at this stage cannot be considered evidence-based interventions for ASD, as both meta-analyses were considered of very low quality.
Sensory-Based Interventions for Children with ASD
There was one moderate quality systematic review examining the efficacy of sensory-based interventions in children with ASD (Weitlauf et al., 2017). The authors reported modest short-term positive effects of these approaches on sensory and motor skills/challenges, ASD symptoms, receptive language, verbal and nonverbal communication, nonverbal cognitive skills, joint-attention and social engagement. However, these conclusions relied on small, short-term studies incorporating different protocols and addressing different outcomes.
Interventions to Improve Anxiety in Children with an ASD Diagnosis
One low quality systematic review into effective treatments for anxiety in children with an ASD diagnosis indicated that CBT interventions were the most well-researched and had the most support. In contrast, the authors of this review stated that there was little evidence for social stories, sensory-integrative interventions, or standalone exposure as being effective in targeting anxiety in this population (Slaughter et al., 2020).
Discussion
On the basis of synthesized review findings, there are several available interventions, mostly, behavioral- and/or CBT-based interventions, which have an overwhelmingly substantial body of evidence in support of their efficacy in supporting social, emotional, and behavioral needs, and can thus be recommended for wide-spread implementation for children ages 4- to 9-years-old. Currently, there is less evidence to recommend wide-scale implementation of non-behavioral or non-cognitive-behavioral interventions for programs targeting children ages 4- to 9-years, though there are various other interventions that seem promising for specific mental health difficulties. The discussion below will include a synthesis of the evidence base that primarily focuses on papers of moderate to high quality.
When targeting mental health difficulties broadly in children, papers of moderate to high quality suggested that behavioral based parenting interventions had the strongest evidence and were efficacious in reducing externalizing symptoms and disruptive behaviors, as well as improving social skills. Across these reviews, smaller, yet significant effect sizes were also found for the improvement of internalizing symptoms for behavioral-based parenting interventions. Furthermore, there was promising evidence across another eight reviews for the efficacy of socio-emotional interventions, in particular, for interventions focusing on emotion understanding, emotion socialization, or attachment. Regarding other interventions, there were a few reviews of art therapy, and positive psychology interventions for managing general distress in young children. These interventions showed improvements in target outcomes, however, conclusions are limited by the small number of studies on these interventions. Overall, this suggests that CBT-based parenting interventions have the strongest evidence base for child mental health difficulties broadly.
Substantial evidence (44 reviews) emerged regarding specific interventions for externalizing symptoms in children. For such children, 24 moderate to high quality reviews concluded that individual and group behavioral and CBT parent-training programs, as well as mixed psychosocial interventions were shown to be efficacious with, on average, small to moderate effect-sizes found at post-intervention and follow-up. Evidence was also found for the efficacy of behavioral and cognitive-behavioral-based interventions overall in four moderate to high quality reviews, with behavioral interventions shown to be effective also when delivered with the child or in a school setting. Beyond this, individual reviews of moderate to high quality demonstrated preliminary evidence that CBT-based social skills training programs, and music interventions reduced externalizing problems.
Regarding internalizing difficulties, one high quality meta-analysis found that CBT-based programs were efficacious in reducing internalizing symptoms in children with on average moderate to large effect-sizes. Despite a small number of studies investigating interventions for internalizing symptoms, of the internalizing disorders, there was substantial evidence (18 reviews) evaluating the effect of CBT programs on anxiety disorders. Across six of seven meta-analyses of moderate to high quality, CBT was also shown to lead to moderate to large effect sizes. One meta-analysis indicated small effect sizes, with the smaller effect size potentially related to methodological differences, such as the inclusion of unpublished papers and this study including only prevention programs. Furthermore, one moderate quality meta-analysis similarly found a parent-based behavioral intervention (PCIT) was efficacious on internalizing symptoms with large effects. However, other interventions that were not behavioral or cognitive-behavioral showed small to minimal effects.
There were a small number of reviews that investigated interventions for children experiencing depressive symptoms (7 reviews) or those exposed to trauma (8 reviews). There is provisional evidence from moderate to high quality papers that psychosocial interventions, notably CBT programs, contribute to a reduction in depressive symptoms in children. A stronger evidence base is required to determine which specific components of CBT are effective and which specific formats and duration of treatments are most beneficial for the reduction of depressive symptoms in children. There are also two high-quality papers suggesting that psychosocial interventions overall are efficacious for trauma symptoms, though more studies are needed to understand which interventions are best. Individual moderate quality reviews also showed preliminary evidence for the efficacy of behavioral-based parenting interventions, trauma-focused CBT, and child-centered play therapy for trauma symptoms.
Beyond that, there was substantial evidence (35 reviews) for interventions supporting children with ADHD symptoms. Across 12 reviews, behavioral parent-training interventions improved ADHD symptoms and comorbid externalizing and internalizing symptoms, with small to large effect-sizes at post-intervention and follow-up. Notably, the quality of reviews for ADHD interventions varied from low to high, though the higher quality reviews (of moderate to high quality) reported moderate to large effect sizes of behavioral parent-training. In addition, a smaller number of moderate quality reviews reported that interventions based on behavioral therapy and CBT more broadly also appeared efficacious in improving ADHD symptoms and one high quality meta-analysis indicated that social skills interventions were promising. Some studies also suggested that combined medication and psychosocial treatments may be superior to either behavioral parent-training or medication alone.
The only two high quality studies in ASD demonstrated the efficacy of behavior-based parent-training and social skills interventions in reducing mental health difficulties in children with ASD. However, the current evidence base is limited as it primarily relies on single case-study designs.
We utilized an exploratory and narrative synthesis of evidence regarding moderators of efficacy. There was heterogeneity on types of moderators examined as well as insufficient power across many reviews to conduct quantitative moderator analyses. However, multiple reviews suggested that children with greater baseline symptom severity tended to benefit more so from interventions, including externalizing (Baumel et al., 2016; de Graaf et al., 2008; Leijten et al., 2020; Riise et al., 2021) and anxiety symptoms (Grist et al., 2019; Howes Vallis et al., 2020). There was also consistent evidence that treatment and selective or indicated prevention interventions yield greater efficacy, compared to universal interventions (2019b; Gardner et al., 2019a; Lösel & Beelmann, 2003; Sanchez et al., 2018; Yap et al., 2016). However, there was mixed evidence for other moderators. For example, there was some evidence to suggest that including both child and parental sessions may be more beneficial in managing externalizing symptoms than parents only interventions (Battagliese et al., 2015) and also more beneficial for anxiety in children than child only interventions (Comer et al., 2019; Grist et al., 2019). Conversely, no clear evidence emerged that including children in interventions for ADHD symptoms increased intervention efficacy over including parents alone (Lee et al., 2012; Mulqueen et al., 2015).
There was also inconsistency in the findings from reviews regarding the impact of treatment length on intervention efficacy. For broad mental health interventions, one review found longer treatments more effective (Carr et al., 2017), whereas another found that number of session hours did not moderate outcome (Buchanan-Pascall et al., 2018). Similarly, for interventions for externalizing symptoms, one review found that treatment length did not moderate response (Comer et al., 2013), another found that brief parenting interventions were effective in reducing child externalizing behaviors (Tully & Hunt, 2016), while others still found that number or intensity of intervention sessions positively predicted intervention effects (Carr et al., 2017; Dretzke et al., 2005; Florean et al., 2020; Menting et al., 2013). Findings for anxiety interventions were similarly mixed, with some papers showing that greater treatment length predicted stronger effects (McGuire et al., 2015; Reynolds et al., 2012), while others showed no effect of treatment length (Ale et al., 2015; Fisak et al., 2011; Krebs et al., 2018). Conversely, for interventions for ADHD symptoms, duration of intervention was not found to influence efficacy (Arnold et al., 2015; Hodgson et al., 2014; Mulqueen et al., 2015; Van der Oord et al., 2008). Thus, the current research base does not at present provide a ‘gold standard’ for treatment length in terms of managing childhood emotional, behavioral, and social problems.
Mixed findings also emerged regarding intervention format. For example, interventions for externalizing symptoms appeared to be efficacious regardless of format of therapy (Comer et al., 2013; de Graaf et al., 2008; Riise et al., 2021); however, one meta-analysis favored individual formats (Fossum et al., 2016). Similarly, for anxiety interventions, some reviews showed no difference between individual and group delivery (Ale et al., 2015; Howes Vallis et al., 2020), while another showed that individual interventions delivered stronger effects on child-reported symptoms (Reynolds et al., 2012). For ADHD interventions, two reviews showed no difference between individual and group delivery of behavioral parent-training interventions (Lee et al., 2012; Rimestad et al., 2019), whereas one recent high quality study found individual behavioral interventions led to larger effects than group delivery (Hornstra, 2023). Collectively, these findings indicate that individual and group-based programs may both have benefits for reducing emotional, behavioral, and social problems in children.
The limitations of the current review must be acknowledged. We limited our search to published meta-analyses and systematic reviews. The emerging literature regarding new approaches would not have been detected by our review if the new approach had not yet accumulated sufficient original research papers to warrant a review paper. We also did not include grey literature in our review. We did not distinguish between symptom reporter in our summary of findings, meaning that we cannot say with confidence whether the current results will hold across child, parent, or observer/clinician reports. Furthermore, we did not consider cost-effectiveness within this review, however would encourage future reviews to do so, given its importance for implementation and policy makers. Lastly, given the heterogeneity of interventions and outcomes within early childhood interventions, we could not conduct any quantitative syntheses of results across studies. Meta-analytic methods are required to make firmer conclusions about the efficacy of various interventions.
Conclusion
Mental disorders are prevalent in children, cause significant distress and lead to significant lifetime burden. Children who experience clinically significant mental health problems do not receive adequate treatment compared to older individuals. An overwhelmingly substantial body of quality evidence was collected as part of this review showing convincingly that we can alter this trend immediately through widespread implementation of targeted intervention programs in the early schooling years. The data showed that targeted interventions lead to better outcomes than universal intervention. Thus, targeted intervention programs should be made available to young children and their families. Parent-based behavioral and cognitive-behavioral interventions had the strongest evidence base, with many moderate to high quality papers supporting its efficacy, for broad mental health difficulties, externalizing issues, and ADHD. There was also substantial support for CBT-based programs for internalizing difficulties, especially in anxiety disorders.
The bulk of the evidence so far has not led to the identification of robust moderators that would allow us to conclude that interventions should definitely be modified for different children. The evidence suggests that children with greater symptom severity benefit more than children with less severity. Behavioral and cognitive behavioral interventions can be delivered in either in group or individual format, with the exception of ADHD, where individual treatment may lead to stronger outcomes. This does not suggest that group treatment is not effective for ADHD, just that individual treatment leads to stronger effects. If resources are not limited in a particular setting offering ADHD treatment, then individual treatment is recommended but if resources are limited, group treatments should still be offered. There is no conclusive evidence regarding whether these treatments should be delivered to the child, parent, or to both the parent and child; with the exception of programs specifically targeting externalizing symptoms or specifically targeting anxiety symptoms. For these problem types, there is evidence that including both parents and children delivers better outcomes than parent or child alone. Taken together, when resources are not limited, parents and children should be included when targeting externalizing and anxiety symptoms. Finally, at present, there is no indication to consistently determine an ideal treatment length, with brief treatments and longer treatments producing similar effects.
We identified a number of gaps for future research. There is less literature on internalizing disorders compared to externalizing disorders in children, and interventions that focus on broad mental health concerns led to smaller effects specifically for internalizing symptoms. This is due to the greater historical focus on externalizing disorders, potentially representing scope for further research to improve efficacy in interventions that target broad mental health symptoms. Of note, reviewing both broad and disorder-specific interventions allowed for a better understanding of how broader interventions can be improved to target specific subgroups. For example, one core component of anxiety interventions is exposure, yet this tends not to be included in broad-based mental health interventions. This may partially contribute to the smaller effect sizes of broad mental health interventions in internalizing difficulties. Lastly, although some interventions seemed promising, there is still an insufficient number of high-quality studies to make strong conclusions regarding recommended interventions for depression, trauma, and ASD in children from 4 to 9 years old.
The current review provides a valuable contribution to the mental health intervention field, by reviewing interventions for not just one, but a constellation of mental health problems in children. We anticipate this review will be useful for those delivering interventions for children (and parents/carers) struggling with their mental health in the initial years of primary school. For governments, schools and practitioners, there is a substantial body of evidence supporting the efficacy of behavioral- and/or CBT-based interventions, for childhood emotional, behavioral, and social problems, which can and should be, as a matter of urgency, implemented with 4–9-year-old children. When selecting broad-based interventions that target mental health, that is, interventions designed to reduce both internalizing and externalizing symptoms, we propose that these interventions should also include specific strategies that target internalizing symptoms such as anxiety. Future research endeavors should focus on increasing implementation and access for young children struggling with their mental health as well as building the evidence base for depression, trauma, and ASD.
Notes
Although this range appears contrary to the defined developmental focus of this paper, studies outside the early schooling years were only included if mean age of the study was within the 4–9 age range and/or specific synthesis occurred for this target age group.
References
Aldabas, R. (2019). Effectiveness of social stories for children with autism: A comprehensive review. Technology & Disability, 31(1/2), 1–13. https://doi.org/10.3233/TAD-180218
Ale, C. M., McCarthy, D. M., Rothschild, L. M., & Whiteside, S. P. H. (2015). Components of cognitive behavioral therapy related to outcome in childhood anxiety disorders. Clinical Child & Family Psychology Review, 18(3), 240–251. https://doi.org/10.1007/s10567-015-0184-8
Arnold, L. E., Hodgkins, P., Caci, H., Kahle, J., & Young, S. (2015). Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: A systematic review. PLoS ONE, 10(2), e0116407. https://doi.org/10.1371/journal.pone.0116407
Bakker, M. J., Greven, C. U., Buitelaar, J. K., & Glennon, J. C. (2017). Practitioner review: Psychological treatments for children and adolescents with conduct disorder problems—A systematic review and meta-analysis. Journal of Child Psychology & Psychiatry, 58(1), 4–18. https://doi.org/10.1111/jcpp.12590
Barlow, J., & Stewart-Brown, S. (2000). Behavior problems and group-based parent education programs. Journal of Developmental and Behavioral Pediatrics, 21(5), 356–370.
Battagliese, G., Caccetta, M., Luppino, O. I., Baglioni, C., Cardi, V., Mancini, F., & Buonanno, C. (2015). Cognitive-behavioral therapy for externalizing disorders: A meta-analysis of treatment effectiveness. Behavior Research & Therapy, 75, 60–71. https://doi.org/10.1016/j.brat.2015.10.008
Bauer, A., Stevens, M., Purtscheller, D., Knapp, M., Fonagy, P., Evans-Lacko, S., & Paul, J. (2021). Mobilising social support to improve mental health for children and adolescents: A systematic review using principles of realist synthesis. PLoS ONE, 16(5), e0251750. https://doi.org/10.1371/journal.pone.0251750
Baumel, A., Pawar, A., Kane, J. M., & Correll, C. U. (2016). Digital parent training for children with disruptive behaviors: Systematic review and meta-analysis of randomized trials. Journal of Child and Adolescent Psychopharmacology, 26(8), 740–749. https://doi.org/10.1089/cap.2016.0048
Baumel, A., Pawar, A., Mathur, N., Kane, J. M., & Correll, C. U. (2017). Technology-assisted parent training programs for children and adolescents with disruptive behaviors: A systematic review. Journal of Clinical Psychiatry, 78(8), e957–e969. https://doi.org/10.4088/JCP.16r11063
Bayer, J., Hiscock, H., Scalzo, K., Mathers, M., McDonald, M., Morris, A., Birdseye, J., & Wake, M. (2009). Systematic review of preventive interventions for children’s mental health: What would work in Australian contexts? Australian & New Zealand Journal of Psychiatry, 43(8), 695–710. https://doi.org/10.1080/00048670903001893
Beames, J. R., Kikas, K., O’Gradey-Lee, M., Gale, N., Werner-Seidler, A., Boydell, K. M., & Hudson, J. L. (2021). A new normal: Integrating lived experience into scientific data syntheses. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2021.763005
Benarous, X., Consoli, A., Guilé, J.-M., Garny Rivière, S., Cohen, D., & Olliac, B. (2017). Evidence-based treatments for youths with severely dysregulated mood: A qualitative systematic review of trials for SMD and DMDD. European Child & Adolescent Psychiatry, 26(1), 5–23. https://doi.org/10.1007/s00787-016-0907-5
Bennett, K., Manassis, K., Walter, S. D., Cheung, A., Wilansky-Traynor, P., Diaz-Granados, N., Duda, S., Rice, M., Baer, S., Barrett, P., Bodden, D., Cobham, V. E., Dadds, M. R., Flannery-Schroeder, E., Ginsburg, G., Heyne, D., Hudson, J. L., Kendall, P. C., Liber, J., & Wood, J. J. (2013). Cognitive behavioral therapy age effects in child and adolescent anxiety: An individual patient data metaanalysis. Depression and Anxiety, 30(9), 829–841. https://doi.org/10.1002/da.22099
Benoit, V., & Gabola, P. (2021). Effects of positive psychology interventions on the well-being of young children: A systematic literature review. International Journal of Environmental Research and Public Health, 18(22), 12065.
Bjornstad, G. J., & Montgomery, P. (2005). Family therapy for attention-deficit disorder or attention-deficit/hyperactivity disorder in children and adolescents. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD005042.pub2
Blewitt, C., O’Connor, A., Morris, H., May, T., Mousa, A., Bergmeier, H., & Skouteris, H. (2021). A systematic review of targeted social and emotional learning interventions in early childhood education and care settings. Early Child Development and Care, 191(14), 2159–2187. https://doi.org/10.1080/03004430.2019.1702037
Bratton, S. C., Ray, D., Rhine, T., & Jones, L. (2005). The efficacy of play therapy with children: A meta-analytic review of treatment outcomes. Professional Psychology: Research and Practice, 36(4), 376–390.
Brooks, R., & Bannigan, K. (2021). Occupational therapy interventions in child and adolescent mental health to increase participation: A mixed methods systematic review. British Journal of Occupational Therapy, 84(8), 474–487. https://doi.org/10.1177/03080226211008718
Buchanan-Pascall, S., Gray, K. M., Gordon, M., & Melvin, G. A. (2018). Systematic review and meta-analysis of parent group interventions for primary school children aged 4–12 years with externalizing and/or internalizing problems. Child Psychiatry & Human Development, 49(2), 244–267. https://doi.org/10.1007/s10578-017-0745-9
Burkey, M. D., Hosein, M., Morton, I., Purgato, M., Adi, A., Kurzrok, M., Kohrt, B. A., & Tol, W. A. (2018). Psychosocial interventions for disruptive behavior problems in children in low- and middle-income countries: A systematic review and meta-analysis. Journal of Child Psychology & Psychiatry, 59(9), 982–993. https://doi.org/10.1111/jcpp.12894
Cai, Q., Chan, A. C., Lee, S. K., Marsalis, S., & Gewirtz, A. H. (2022). Effectiveness of generation PMTO to promote parenting and child adjustment: A meta-analytic review. Clinical Child and Family Psychology Review. https://doi.org/10.1007/s10567-022-00400-9
Caldwell, D. M., Davies, S. R., Hetrick, S. E., Palmer, J. C., Caro, P., López-López, J. A., Gunnell, D., Kidger, J., Thomas, J., French, C., Stockings, E., Campbell, R., & Welton, N. J. (2019). School-based interventions to prevent anxiety and depression in children and young people: A systematic review and network meta-analysis. Lancet Psychiatry, 6(12), 1011–1020. https://doi.org/10.1016/s2215-0366(19)30403-1
Camargo, S. P. H., Rispoli, M., Ganz, J., Hong, E. R., Davis, H., & Mason, R. (2014). A review of the quality of behaviorally-based intervention research to improve social interaction skills of children with ASD in inclusive settings. Journal of Autism and Developmental Disorders, 44, 2096–2116. https://doi.org/10.1007/s10803-014-2060-7
Camargo, S. P. H., Rispoli, M., Ganz, J., Hong, E. R., Davis, H., & Mason, R. (2016). Behaviorally based interventions for teaching social interaction skills to children with ASD in inclusive settings: A meta-analysis. Journal of Behavioral Education, 25(2), 223–248. https://doi.org/10.1007/s10864-015-9240-1
Carr, A., Hartnett, D., Brosnan, E., & Sharry, J. (2017). Parents plus systemic, solution-focused parent training programs: Description, review of the evidence base, and meta-analysis. Family Process, 56(3), 652–668. https://doi.org/10.1111/famp.12225
Coates, J., Taylor, J. A., & Sayal, K. (2015). Parenting interventions for ADHD: A systematic literature review and meta-analysis. Journal of Attention Disorders, 19(10), 831–843. https://doi.org/10.1177/1087054714535952
Comer, J. S., Chow, C., Chan, P. T., Cooper-Vince, C., Wilson, L. A., Comer, J. S., Chow, C., Chan, P. T., Cooper-Vince, C., & Wilson, L. A. S. (2013). Psychosocial treatment efficacy for disruptive behavior problems in very young children: A meta-analytic examination. Journal of the American Academy of Child & Adolescent Psychiatry, 52(1), 26–36. https://doi.org/10.1016/j.jaac.2012.10.001
Comer, J. S., Hong, N., Poznanski, B., Silva, K., & Wilson, M. (2019). Evidence base update on the treatment of early childhood anxiety and related problems. Journal of Clinical Child & Adolescent Psychology, 48(1), 1–15. https://doi.org/10.1080/15374416.2018.1534208
Connor, D. F., Carlson, G. A., Chang, K. D., Daniolos, P. T., Ferziger, R., Findling, R. L., Hutchinson, J. G., Malone, R. P., Halperin, J. M., Plattner, B., Post, R. M., Reynolds, D. L., Rogers, K. M., Saxena, K., & Steiner, H. (2006). Juvenile maladaptive aggression: A review of prevention, treatment, and service configuration and a proposed research agenda. Journal of Clinical Psychiatry, 67(5), 808–820.
Corcoran, J., & Dattalo, P. (2006). Parent involvement in treatment for ADHD: A meta-analysis of the published studies. Research on Social Work Practice, 16(6), 561–570. https://doi.org/10.1177/1049731506289127
Cornell, H. R., Lin, T. T., & Anderson, J. A. (2018). A systematic review of play-based interventions for students with ADHD: Implications for school-based occupational therapists. Journal of Occupational Therapy, Schools & Early Intervention, 11(2), 192–211. https://doi.org/10.1080/19411243.2018.1432446
Cuijpers, P., Karyotaki, E., Ciharova, M., Miguel, C., Noma, H., Stikkelbroek, Y., & Furukawa, T. A. (2023). The effects of psychological treatments of depression in children and adolescents on response, reliable change, and deterioration: A systematic review and meta-analysis. European Child & Adolescent Psychiatry, 32(1), 177–192. https://doi.org/10.1007/s00787-021-01884-6
Dalgaard, N. T., Filges, T., Viinholt, B. C., & Pontoppidan, M. (2022). Parenting interventions to support parent/child attachment and psychosocial adjustment in foster and adoptive parents and children: A systematic review. Campbell Systematic Reviews, 18(1), e1209. https://doi.org/10.1002/cl2.1209
de Graaf, I., Speetjens, P., Smit, F., de Wolff, M., & Tavecchio, L. (2008). Effectiveness of the triple P positive parenting program on behavioral problems in children: A meta-analysis. Behavior Modification, 32(5), 714–735. https://doi.org/10.1177/0145445508317134
Dedousis-Wallace, A., Drysdale, S. A., McAloon, J., & Ollendick, T. H. (2021). Parental and familial predictors and moderators of parent management treatment programs for conduct problems in youth. Clinical Child & Family Psychology Review, 24(1), 92–119. https://doi.org/10.1007/s10567-020-00330-4
Dretzke, J., Davenport, C., Frew, E., Barlow, J., Stewart-Brown, S., Bayliss, S., Taylor, R. S., Sandercock, J., & Hyde, C. (2009). The clinical effectiveness of different parenting programmes for children with conduct problems: A systematic review of randomised controlled trials. Child & Adolescent Psychiatry & Mental Health, 3, 1–10. https://doi.org/10.1186/1753-2000-3-7
Dretzke, J., Frew, E., Davenport, C., Barlow, J., Stewart-Brown, S., Sandercock, J., Bayliss, S., Raftery, J., Hyde, C., & Taylor, R. (2005). The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children. Health Technology Assessment [winchester, England], 9(50), iii.
England-Mason, G., Andrews, K., Atkinson, L., & Gonzalez, A. (2023). Emotion socialization parenting interventions targeting emotional competence in young children: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review. https://doi.org/10.1016/j.cpr.2023.102252
Everett, Y., Martin, C. G., & Zalewski, M. (2021). A systematic review focusing on psychotherapeutic interventions that impact parental psychopathology, child psychopathology and parenting behavior. Clinical Child and Family Psychology Review, 24, 579–598. https://doi.org/10.1007/s10567-021-00355-3
Fabiano, G. A., Pelham, W. E., Coles, E. K., Gnagy, E. M., Chronis-Tuscano, A., & O’Connor, B. C. (2009). A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review, 29(2), 129–140. https://doi.org/10.1016/j.cpr.2008.11.001
Fisak, B. J., Jr., Richard, D., & Mann, A. (2011). The prevention of child and adolescent anxiety: A meta-analytic review. Prevention Science, 12(3), 255–268. https://doi.org/10.1007/s11121-011-0210-0
Florean, I. S., Dobrean, A., Păsărelu, C. R., Georgescu, R. D., & Milea, I. (2020). The efficacy of internet-based parenting programs for children and adolescents with behavior problems: A meta-analysis of randomized clinical trials. Clinical Child & Family Psychology Review, 23(4), 510–528. https://doi.org/10.1007/s10567-020-00326-0
Forster, M., Kling, Å., & Sundell, K. (2012). Clinical significance of parent training for children with conduct problems. International Journal of Conflict & Violence, 6(2), 188–200.
Forti-Buratti, M., Saikia, R., Wilkinson, E., & Ramchandani, P. (2016). Psychological treatments for depression in pre-adolescent children (12 years and younger): Systematic review and meta-analysis of randomised controlled trials. European Child & Adolescent Psychiatry, 25(10), 1045–1054. https://doi.org/10.1007/s00787-016-0834-5
Fossum, S., Handegård, B., Adolfsen, F., Vis, S., & Wynn, R. (2016). A meta-analysis of long-term outpatient treatment effects for children and adolescents with conduct problems. Journal of Child & Family Studies, 25(1), 15–29. https://doi.org/10.1007/s10826-015-0221-8
Fossum, S., Handegård, B. H., Martinussen, M., & Mørch, W. T. (2008). Psychosocial interventions for disruptive and aggressive behavior in children and adolescents: A meta-analysis. European Child & Adolescent Psychiatry, 17(7), 438–451. https://doi.org/10.1007/s00787-008-0686-8
Fox, A., Dishman, S., Valicek, M., Ratcliff, K., & Hilton, C. (2020). Effectiveness of social skills interventions incorporating peer interactions for children with attention deficit hyperactivity disorder: A systematic review. American Journal of Occupational Therapy, 74(2), 1–19. https://doi.org/10.5014/ajot.2020.040212
Furlong, M., McGilloway, S., Bywater, T., Hutchings, J., Smith, S. M., & Donnelly, M. (2012). behavioral and cognitive-behavioral group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD008225.pub2
Gaastra, G. F., Groen, Y., Tucha, L., & Tucha, O. (2016). The effects of classroom interventions on off-task and disruptive classroom behavior in children with symptoms of attention-deficit/hyperactivity disorder: A meta-analytic review. PLoS ONE, 11(2), e0148841. https://doi.org/10.1371/journal.pone.0148841
Gardner, F., Leijten, P., Harris, V., Mann, J., Hutchings, J., Beecham, J., Bonin, E. M., Berry, V., McGilloway, S., Gaspar, M., João Seabra-Santos, M., Orobio de Castro, B., Menting, A., Williams, M., Axberg, U., Morch, W. T., Scott, S., & Landau, S. (2019a). Equity effects of parenting interventions for child conduct problems: A pan-European individual participant data meta-analysis. Lancet Psychiatry, 6(6), 518–527. https://doi.org/10.1016/s2215-0366(19)30162-2
Gardner, F., Leijten, P., Melendez-Torres, G. J., Landau, S., Harris, V., Mann, J., Beecham, J., Hutchings, J., Scott, S., & Melendez-Torres, G. J. (2019b). The earlier the better? Individual participant data and traditional meta-analysis of age effects of parenting interventions. Child Development, 90(1), 7–19. https://doi.org/10.1111/cdev.13138
Ghuman, J. K., Arnold, L. E., & Anthony, B. J. (2008). Psychopharmacological and other treatments in preschool children with attention-deficit/hyperactivity disorder: Current evidence and practice. Journal of Child and Adolescent Psychopharmacology, 18(5), 413–447.
Grist, R., Stallard, P., Croker, A., & Denne, M. (2019). Technology delivered interventions for depression and anxiety in children and adolescents: A systematic review and meta-analysis. Clinical Child & Family Psychology Review, 22(2), 147–171. https://doi.org/10.1007/s10567-018-0271-8
Groenman, A. P., Hornstra, R., Hoekstra, P. J., Steenhuis, L., Aghebati, A., Boyer, B. E., & van den Hoofdakker, B. J. (2022). An individual participant data meta-analysis: behavioral treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 61(2), 144–158. https://doi.org/10.1016/j.jaac.2021.02.024
Gunning, C., Holloway, J., Fee, B., Breathnach, Ó., Bergin, C. M., Greene, I., & Ní Bheoláin, R. (2019). A systematic review of generalization and maintenance outcomes of social skills intervention for preschool children with autism spectrum disorder. Review Journal of Autism and Developmental Disorders, 6(2), 172–199. https://doi.org/10.1007/s40489-019-00162-1
Guthold, R., Johansson, E. W., Mathers, C. D., & Ross, D. A. (2021). Global and regional levels and trends of child and adolescent morbidity from 2000 to 2016: An analysis of years lost due to disability (YLDs). BMJ Global Health, 6(3), e004996. https://doi.org/10.1136/bmjgh-2021-004996
Guyatt, G., Oxman, A. D., Akl, E. A., Kunz, R., Vist, G., Brozek, J., & Schünemann, H. J. (2011). GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology, 64(4), 383–394.
Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., & Schünemann, H. J. (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 336(7650), 924–926.
Hambrick, E. P., & Oppenheim-Weller, S. (2016). Mental health interventions for children in foster care: A systematic review. Children & Youth Services Review, 70, 65–77. https://doi.org/10.1016/j.childyouth.2016.09.002
Harrison, J. R., Soares, D. A., Rudzinski, S., & Johnson, R. (2019). Attention deficit hyperactivity disorders and classroom-based interventions: Evidence-based status, effectiveness, and moderators of effects in single-case design research. Review of Educational Research, 89(4), 569–611. https://doi.org/10.3102/0034654319857038
Hodgson, K., Hutchinson, A. D., & Denson, L. (2014). Nonpharmacological treatments for ADHD: A meta-analytic review. Journal of Attention Disorders, 18(4), 275–282. https://doi.org/10.1177/1087054712444732
Hornstra, R., Groenman, A. P., van der Oord, S., Luman, M., Dekkers, T. J., van der Veen-Mulders, L., & van den Hoofdakker, B. J. (2023). Which components of behavioral parent and teacher training work for children with ADHD?—A metaregression analysis on child behavioral outcomes. Child and Adolescent Mental Health, 28(2), 258–268. https://doi.org/10.1111/camh.12561
Howes Vallis, E., Zwicker, A., Uher, R., & Pavlova, B. (2020). Cognitive-behavioral interventions for prevention and treatment of anxiety in young children: A systematic review and meta-analysis. Clinical Psychology Review. https://doi.org/10.1016/j.cpr.2020.101904
Humble, J. J., Summers, N. L., Villarreal, V., Styck, K. M., Sullivan, J. R., Hechler, J. M., & Warren, B. S. (2019). Child-centered play therapy for youths who have experienced trauma: A systematic literature review. Journal of Child & Adolescent Trauma, 12(3), 365–375. https://doi.org/10.1007/s40653-018-0235-7
Iznardo, M., Rogers, M. A., Volpe, R. J., Labelle, P. R., & Robaey, P. (2020). The effectiveness of daily behavior report cards for children with ADHD: A meta-analysis. Journal of Attention Disorders, 24(12), 1623–1636. https://doi.org/10.1177/1087054717734646
John-Baptiste Bastien, R., Jongsma, H. E., Kabadayi, M., & Billings, J. (2020). The effectiveness of psychological interventions for post-traumatic stress disorder in children, adolescents and young adults: A systematic review and meta-analysis. Psychological Medicine, 50(10), 1598–1612. https://doi.org/10.1017/S0033291720002007
Jugovac, S., O’Kearney, R., Hawes, D. J., & Pasalich, D. S. (2022). Attachment-and emotion-focused parenting interventions for child and adolescent externalizing and internalizing behaviors: A meta-analysis. Clinical Child and Family Psychology Review. https://doi.org/10.1007/s10567-022-00401-8
Kokina, A., & Kern, L. (2010). Social story interventions for students with autism spectrum disorders: A meta-analysis. Journal of Autism & Developmental Disorders, 40(7), 812–826. https://doi.org/10.1007/s10803-009-0931-0
Krebs, G., Pile, V., Grant, S., Degli Esposti, M., Montgomery, P., & Lau, J. Y. F. (2018). Research review: Cognitive bias modification of interpretations in youth and its effect on anxiety: A meta-analysis. Journal of Child Psychology and Psychiatry, 59(8), 831–844. https://doi.org/10.1111/jcpp.12809
Krisanaprakornkit, T., Ngamjarus, C., Witoonchart, C., & Piyavhatkul, N. (2010). Meditation therapies for attention-deficit/hyperactivity disorder (ADHD). Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD006507.pub2
Lane, C., Hogg, E., Karwatowska, L. A., French, L., Ranieri, V. F., Jesnick, L. G., & Kennedy, E. M. (2023). Personalised interventions for subgroups of children with conduct problems. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD012746.pub2
Laurens, K. R., Graham, L. J., Dix, K. L., Harris, F., Tzoumakis, S., Williams, K. E., & Green, M. J. (2022). School-based mental health promotion and early intervention programs in new south wales, Australia: mapping practice to policy and evidence. School Mental Health, 14(3), 582–597. https://doi.org/10.1007/s12310-021-09482-2
Law, J., Plunkett, C. C., & Stringer, H. (2012). Communication interventions and their impact on behaviour in the young child: A systematic review. Child Language Teaching and Therapy, 28(1), 7–23. https://doi.org/10.1177/0265659011414214
Lawrence, D., Hafekost, J., Johnson, S. E., Saw, S., Buckingham, W. J., Sawyer, M. G., Ainley, J., & Zubrick, S. R. (2016). Key findings from the second Australian child and adolescent survey of mental health and wellbeing. Australian & New Zealand Journal of Psychiatry, 50(9), 876–886. https://doi.org/10.1177/0004867415617836
Ledford, J. R., & Pustejovsky, J. E. (2023). Systematic review and meta-analysis of stay-play-talk interventions for improving social behaviors of young children. Journal of Positive Behavior Interventions, 25(1), 65–77. https://doi.org/10.1177/1098300720983521
Lee, P., Niew, W., Yang, H., Chen, V. C., & Lin, K. (2012). A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Research in Developmental Disabilities: A Multidisciplinary Journal, 33(6), 2040–2049. https://doi.org/10.1016/j.ridd.2012.05.011
Leijten, P., Melendez-Torres, G. J., Gardner, F., van Aar, J., Schulz, S., & Overbeek, G. (2018). Are relationship enhancement and behavior management “the golden couple” for disruptive child behavior? Two Meta-Analyses. Child Development, 89(6), 1970–1982. https://doi.org/10.1111/cdev.13051
Leijten, P., Melendez-Torres, G. J., Knerr, W., & Gardner, F. (2016). Transported versus homegrown parenting interventions for reducing disruptive child behavior: A multilevel meta-regression study. Journal of the American Academy of Child & Adolescent Psychiatry, 55(7), 610–617. https://doi.org/10.1016/j.jaac.2016.05.003
Leijten, P., Raaijmakers, M. A. J., de Castro, B. O., & Matthys, W. (2013). Does socioeconomic status matter? A meta-analysis on parent training effectiveness for disruptive child behavior. Journal of Clinical Child and Adolescent Psychology, 42(3), 384–392. https://doi.org/10.1080/15374416.2013.769169
Leijten, P., Scott, S., Landau, S., Harris, V., Mann, J., Hutchings, J., Beecham, J., & Gardner, F. (2020). Individual participant data meta-analysis: Impact of conduct problem severity, comorbid attention-deficit/hyperactivity disorder and emotional problems, and maternal depression on parenting program effects. Journal of the American Academy of Child & Adolescent Psychiatry, 59(8), 933–943. https://doi.org/10.1016/j.jaac.2020.01.023
Lindstrom Johnson, S., Elam, K., Rogers, A. A., & Hilley, C. (2018). A meta-analysis of parenting practices and child psychosocial outcomes in trauma-informed parenting interventions after violence exposure. Prevention Science, 19(7), 927–938. https://doi.org/10.1007/s11121-018-0943-0
Lösel, F., & Beelmann, A. (2003). Effects of child skills training in preventing antisocial behavior: A systematic review of randomized evaluations. Annals of the American Academy of Political and Social Science, 587, 84–109. https://doi.org/10.1177/0002716202250793
Maughan, D. R., Christiansen, E., Jenson, W. R., Olympia, D., & Clark, E. (2005). behavioral parent training as a treatment for externalizing behaviors and disruptive behavior disorders: A meta-analysis. School Psychology Review, 34(3), 267–286.
McDonald, A., & Drey, N. S. (2018). Primary-school-based art therapy: A review of controlled studies. International Journal of Art Therapy: Inscape, 23(1), 33–44. https://doi.org/10.1080/17454832.2017.1338741
McGoey, K. E., Eckert, T. L., & DuPaul, G. J. (2002). Early intervention for preschool-age children with ADHD: A literature review. Journal of Emotional & Behavioral Disorders, 10(1), 14–28. https://doi.org/10.1177/106342660201000103
McGuire, A., Steele, R. G., & Singh, M. N. (2021). Systematic review on the application of trauma-focused cognitive behavioral therapy (TF-CBT) for preschool-aged children. Clinical Child & Family Psychology Review, 24(1), 20–37. https://doi.org/10.1007/s10567-020-00334-0
McGuire, J. F., Piacentini, J., Lew, A. B., Brennan, E. A., Murphy, T. K., & Storch, E. A. (2015). A meta-analysis of cognitive behavior therapy and medication for child obsessive-compulsive disorder: Moderators of treatment efficacy, response, and remission. Depression and Anxiety, 32(8), 580–593. https://doi.org/10.1002/da.22389
Menting, A. T. A., de Castro, B. O., & Matthys, W. (2013). Effectiveness of the incredible years parent training to modify disruptive and prosocial child behavior: A meta-analytic review. Clinical Psychology Review, 33(8), 901–913. https://doi.org/10.1016/j.cpr.2013.07.006
Michael, K. D., & Crowley, S. L. (2002). How effective are treatments for child and adolescent depression? A Meta-Analytic Review. Clin Psychol Rev, 22(2), 247–269. https://doi.org/10.1016/s0272-7358(01)00089-7
Mingebach, T., Kamp-Becker, I., Christiansen, H., & Weber, L. (2018). Meta-meta-analysis on the effectiveness of parent-based interventions for the treatment of child externalizing behavior problems. PLoS ONE, 13(9), e0202855. https://doi.org/10.1371/journal.pone.0202855
Money, R., Wilde, S., & Dawson, D. (2021). The effectiveness of theraplay for children under 12–a systematic literature review. Child and Adolescent Mental Health, 26(3), 238–251. https://doi.org/10.1111/camh.12416
Moula, Z. (2020). A systematic review of the effectiveness of art therapy delivered in school-based settings to children aged 5–12 years. International Journal of Art Therapy: Inscape, 25(2), 88–99. https://doi.org/10.1080/17454832.2020.1751219
Moula, Z., Aithal, S., Karkou, V., & Powell, J. (2020). A systematic review of child-focused outcomes and assessments of arts therapies delivered in primary mainstream schools. Children & Youth Services Review. https://doi.org/10.1016/j.childyouth.2020.104928
Mulqueen, J. M., Bartley, C. A., & Bloch, M. H. (2015). Meta-analysis: Parental interventions for preschool ADHD. Journal of Attention Disorders, 19(2), 118–124. https://doi.org/10.1177/1087054713504135
Murray, D. W., Lawrence, J. R., & LaForett, D. R. (2018). The incredible years® programs for ADHD in young children: A critical review of the evidence. Journal of Emotional & Behavioral Disorders, 26(4), 195–208. https://doi.org/10.1177/1063426617717740
Nogueira, S., Canário, A. C., Abreu-Lima, I., Teixeira, P., & Cruz, O. (2022). Group triple P intervention effects on children and parents: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(4), 2113. https://doi.org/10.3390/ijerph19042113
Nye, E., Melendez-Torres, G. J., & Gardner, F. (2019). Mixed methods systematic review on effectiveness and experiences of the incredible years teacher classroom management programme. Review of Education, 7(3), 631–669. https://doi.org/10.1002/rev3.3145
Odgers, K., Dargue, N., Creswell, C., Jones, M. P., & Hudson, J. L. (2020). The limited effect of mindfulness-based interventions on anxiety in children and adolescents: A meta-analysis. Clinical Child & Family Psychology Review, 23(3), 407–426. https://doi.org/10.1007/s10567-020-00319-z
Østergaard, K. R. (2018). Treatment of selective mutism based on cognitive behavioral therapy, psychopharmacology and combination therapy—A systematic review. Nordic Journal of Psychiatry, 72(4), 240–250. https://doi.org/10.1080/08039488.2018.1439530
Parker, M. M., Hergenrather, K., Smelser, Q., & Kelly, C. T. (2021a). Exploring child-centered play therapy and trauma: A systematic review of literature. International Journal of Play Therapy, 30(1), 2–13. https://doi.org/10.1037/pla0000136
Parker, M. M., Hunnicutt Hollenbaugh, K. M., & Kelly, C. T. (2021b). Exploring the impact of child-centered play therapy for children exhibiting behavioral problems: A meta-analysis. International Journal of Play Therapy, 30(4), 259. https://doi.org/10.1037/pla0000128
Pauli-Pott, U., Mann, C., & Becker, K. (2021). Do cognitive interventions for preschoolers improve executive functions and reduce ADHD and externalizing symptoms? A meta-analysis of randomized controlled trials. European Child & Adolescent Psychiatry, 30, 1503–1521. https://doi.org/10.1007/s00787-020-01627-z
Pester, D., Lenz, A. S., & Dell’Aquila, J. (2019). Meta-analysis of single-case evaluations of child-centered play therapy for treating mental health symptoms. International Journal of Play Therapy, 28(3), 144–156. https://doi.org/10.1037/pla0000098
Phillips, S., & Mychailyszyn, M. (2021). A review of parent-child interaction therapy (PCIT): Applications for youth anxiety. Children and Youth Services Review, 125, 105986. https://doi.org/10.1016/j.childyouth.2021.105986
Pilling, S., Fonagy, P., Allison, E., Barnett, P., Campbell, C., Constantinou, M., Gardner, T., Lorenzini, N., Matthews, H., Ryan, A., Sacchetti, S., Truscott, A., Ventura, T., Watchorn, K., Whittington, C., & Kendall, T. (2020). Long-term outcomes of psychological interventions on children and young people’s mental health: A systematic review and meta-analysis. PLoS ONE, 15(11), 28. https://doi.org/10.1371/journal.pone.0236525
Purgato, M., Gross, A. L., Betancourt, T., Bolton, P., Bonetto, C., Gastaldon, C., Gordon, J., O’Callaghan, P., Papola, D., Peltonen, K., Punamaki, R. L., Richards, J., Staples, J. K., Unterhitzenberger, J., van Ommeren, M., de Jong, J., Jordans, M. J. D., Tol, W. A., & Barbui, C. (2018). Focused psychosocial interventions for children in low-resource humanitarian settings: A systematic review and individual participant data meta-analysis. The Lancet Global Health, 6(4), e390–e400. https://doi.org/10.1016/s2214-109x(18)30046-9
Pyle, K., & Fabiano, G. A. (2017). Daily report card intervention and attention deficit hyperactivity disorder: A meta-analysis of single-case studies. Exceptional Children, 83(4), 378–395. https://doi.org/10.1177/0014402917706370
Reichow, B., Steiner, A. M., & Volkmar, F. (2013). Cochrane review: Social skills groups for people aged 6 to 21 with autism spectrum disorders (ASD). Evidence-Based Child Health: A Cochrane Review Journal, 8, 266–315. https://doi.org/10.1002/ebch.1903
Reid, R., Trout, A. L., & Schartz, M. (2005). Self-regulation interventions for children with attention deficit/hyperactivity disorder. Exceptional Children, 71(4), 17–361.
Reynolds, S., Wilson, C., Austin, J., & Hooper, L. (2012). Effects of psychotherapy for anxiety in children and adolescents: A meta-analytic review. Clinical Psychology Review, 32(4), 251–262. https://doi.org/10.1016/j.cpr.2012.01.005
Riise, E. N., Wergeland, G. J. H., Njardvik, U., & Öst, L.-G. (2021). Cognitive behavior therapy for externalizing disorders in children and adolescents in routine clinical care: A systematic review and meta-analysis. Clinical Psychology Review. https://doi.org/10.1016/j.cpr.2020.101954
Rimestad, M. L., Lambek, R., Zacher Christiansen, H., & Hougaard, E. (2019). Short- and long-term effects of parent training for preschool children with or at risk of ADHD: A systematic review and meta-analysis. Journal of Attention Disorders, 23(5), 423–434. https://doi.org/10.1177/1087054716648775
Rosner, R., Kruse, J., & Hagl, M. (2010). A meta-analysis of interventions for bereaved children and adolescents. Death Studies, 34(2), 99–136. https://doi.org/10.1080/07481180903492422
Sanchez, A. L., Cornacchio, D., Poznanski, B., Golik, A. M., Chou, T., & Comer, J. S. (2018). The effectiveness of school-based mental health services for elementary-aged children: A meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 57(3), 153–165. https://doi.org/10.1016/j.jaac.2017.11.022
Savaglio, M., Yap, M. B., O’Donnell, R., & Skouteris, H. (2023). Targeted community-based programmes for children’s mental health: A systematic review and meta-analysis of the Australian literature. Australian & New Zealand Journal of Psychiatry, 57(2), 197–212. https://doi.org/10.1177/00048674221124506
Sawyer, M. G., Reece, C. E., Sawyer, A. C. P., Johnson, S. E., & Lawrence, D. (2018). Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? Journal of the American Academy of Child & Adolescent Psychiatry, 57(5), 343-350.e5. https://doi.org/10.1016/j.jaac.2018.02.012
Schleider, J. L., & Weisz, J. R. (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56(2), 107–115. https://doi.org/10.1016/j.jaac.2016.11.007
Sheridan, S. M., Smith, T. E., Moorman Kim, E., Beretvas, S. N., & Park, S. (2019). A meta-analysis of family-school interventions and children’s social-emotional functioning: Moderators and components of efficacy. Review of Educational Research, 89(2), 296–332. https://doi.org/10.3102/0034654318825437
Shucksmith, J., Jones, S., & Summerbell, C. (2010). The role of parental involvement in school-based mental health interventions at primary (elementary) school level. Advances in School Mental Health Promotion, 3(1), 18–29. https://doi.org/10.1080/1754730X.2010.9715671
Slaughter, A. M., McNeel, M. M., Storch, E. A., & Mire, S. S. (2020). Where should we go from here? Identified gaps in the literature in psychosocial interventions for youth with autism spectrum disorder and comorbid anxiety. Children’s Health Care, 49(4), 435–471. https://doi.org/10.1080/02739615.2020.1756818
Smith, S., Barajas, K., Ellis, B., Moore, C., McCauley, S., & Reichow, B. (2021). A meta-analytic review of randomized controlled trials of the good behavior game. Behavior Modification, 45(4), 641–666. https://doi.org/10.1177/0145445519878670
Solomon, D. T., Niec, L. N., & Schoonover, C. E. (2017). The impact of foster parent training on parenting skills and child disruptive behavior: A meta-analysis. Child Maltreatment, 22(1), 3–13. https://doi.org/10.1177/1077559516679514
Sprung, M., Münch, H. M., Harris, P. L., Ebesutani, C., & Hofmann, S. G. (2015). Children’s emotion understanding: A meta-analysis of training studies. Developmental Review, 37, 41–65. https://doi.org/10.1016/j.dr.2015.05.001
Steains, S. Y., Malouff, J. M., & Schutte, N. S. (2021). Efficacy of psychological interventions for selective mutism in children: A meta-analysis of randomized controlled trials. Child: Care, Health and Development, 47(6), 771–781. https://doi.org/10.1111/cch.12895
Stoltz, S., van Londen, M., Dekovic, M., de Castro, B. O., & Prinzie, P. (2012). Effectiveness of individually delivered indicated school-based interventions on externalizing behavior. International Journal of Behavioral Development, 36(5), 381–388. https://doi.org/10.1177/0165025412450525
Storebø, O. J., Elmose Andersen, M., Skoog, M., Joost Hansen, S., Simonsen, E., Pedersen, N., Tendal, B., Callesen, H. E., Faltinsen, E., & Gluud, C. (2019). Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD008223.pub3
Sun, M., Rith-Najarian, L. R., Williamson, T. J., & Chorpita, B. F. (2019). Treatment features associated with youth cognitive behavioral therapy follow-up effects for internalizing disorders: A meta-analysis. Journal of Clinical Child & Adolescent Psychology, 48, S269–S283. https://doi.org/10.1080/15374416.2018.1443459
Sun, Y., Lamoreau, R., O’Connell, S., Horlick, R., & Bazzano, A. N. (2021). Yoga and mindfulness interventions for preschool-aged children in educational settings: A systematic review. International Journal of Environmental Research and Public Health, 18(11), 6091. https://doi.org/10.3390/ijerph18116091
Tan-MacNeill, K. M., Smith, I. M., Johnson, S. A., Chorney, J., & Corkum, P. (2021). A systematic review of online parent-implemented interventions for children with neurodevelopmental disorders. Children’s Health Care, 50(3), 239–277. https://doi.org/10.1080/02739615.2021.1886934
Tarver, J., Daley, D., Lockwood, J., & Sayal, K. (2014). Are self-directed parenting interventions sufficient for Externalizing behavior problems in childhood? A systematic review and meta-analysis. European Child & Adolescent Psychiatry, 23(12), 1123–1137. https://doi.org/10.1007/s00787-014-0556-5
Tarver, J., Palmer, M., Webb, S., Scott, S., Slonims, V., Simonoff, E., & Charman, T. (2019). Child and parent outcomes following parent interventions for child emotional and behavioral problems in autism spectrum disorders: A systematic review and meta-analysis. Autism the International Journal of Research and Practice, 23(7), 1630–1644. https://doi.org/10.1177/1362361319830042
Thongseiratch, T., Leijten, P., & Melendez-Torres, G. J. (2020). Online parent programs for children’s behavioral problems: A meta-analytic review. European Child and Adolescent Psychiatry, 29(11), 1555–1568. https://doi.org/10.1007/s00787-020-01472-0
Tse, J. (2006). Research on day treatment programs for preschoolers with disruptive behavior disorders. Psychiatric Services, 57(4), 477–486. https://doi.org/10.1176/ps.2006.57.4.477
Tully, L., & Hunt, C. (2016). Brief parenting interventions for children at risk of externalizing behavior problems: A systematic review. Journal of Child & Family Studies, 25(3), 705–719. https://doi.org/10.1007/s10826-015-0284-6
Türk, S., Korfmacher, A. K., Gerger, H., van der Oord, S., & Christiansen, H. (2023). Interventions for ADHD in childhood and adolescence: A systematic umbrella review and meta-meta-analysis. Clinical Psychology Review, 102, 102271.
Uretsky, M. C., & Hoffman, J. A. (2017). Evidence for group-based foster parent training programs in reducing externalizing child behaviors: A systematic review and meta-analysis. Journal of Public Child Welfare, 11(4/5), 464–486. https://doi.org/10.1080/15548732.2017.1326360
Vacher, C., Goujon, A., Romo, L., & Purper-Ouakil, D. (2020). Efficacy of psychosocial interventions for children with ADHD and emotion dysregulation: A systematic review. Psychiatry Research. https://doi.org/10.1016/j.psychres.2020.113151
van der Oord, S., Prins, P. J. M., Oosterlaan, J., & Emmelkamp, P. M. G. (2008). Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: A meta-analysis. Clinical Psychology Review, 28(5), 783–800.
Veenman, B., Luman, M., & Oosterlaan, J. (2018). Efficacy of behavioral classroom programs in primary school. A meta-analysis focusing on randomized controlled trials. PLoS ONE, 13(10), e0201779. https://doi.org/10.1371/journal.pone.0201779
Vekety, B., Logemann, H. A., & Takacs, Z. K. (2021). The effect of mindfulness-based interventions on inattentive and hyperactive–impulsive behavior in childhood: A meta-analysis. International Journal of Behavioral Development, 45(2), 133–145. https://doi.org/10.1177/0165025420958192
Vetter, J. A. (2018). Parent-child interaction therapy for autism spectrum and attention-deficit/hyperactivity disorders: A review of the literature. Child & Family Behavior Therapy, 40(3), 204–232. https://doi.org/10.1080/07317107.2018.1487740
Viswanathan, M., Wallace, I. F., Middleton, J. C., Kennedy, S. M., McKeeman, J., Hudson, K., & Kahwati, L. (2022). Screening for anxiety in children and adolescents: Evidence report and systematic review for the US preventive services task force. JAMA, 328(14), 1445–1455. https://doi.org/10.1007/s00787-020-01627-z
Wahman, C. L., Pustejovsky, J. E., Ostrosky, M. M., & Santos, R. M. (2022). Examining the effects of social stories™ on challenging behavior and prosocial skills in young children: A systematic review and meta-analysis. Topics in Early Childhood Special Education, 41(4), 267–279.
Wang, P., & Spillane, A. (2009). Evidence-based social skills interventions for children with autism: A meta-analysis. Education and Training in Developmental Disabilities, 44, 318–342.
Wang, S.-Y., Cui, Y., & Parrila, R. (2011). Examining the effectiveness of peer-mediated and video-modeling social skills interventions for children with autism spectrum disorders: A meta-analysis in single-case research using HLM. Research in Autism Spectrum Disorders, 5(1), 562–569. https://doi.org/10.1016/j.rasd.2010.06.023
Wang, S.-Y., Parrila, R., & Cui, Y. (2013). Meta-analysis of social skills interventions of single-case research for individuals with autism spectrum disorders: Results from three-level HLM. Journal of Autism & Developmental Disorders, 43(7), 1701–1716. https://doi.org/10.1007/s10803-012-1726-2
Ward, M., Theule, J., & Cheung, K. (2016). Parent-child interaction therapy for child disruptive behavior disorders: A meta-analysis. Child & Youth Care Forum, 45(5), 675–690. https://doi.org/10.1007/s10566-016-9350-5
Weitlauf, A. S., Sathe, N., McPheeters, M. L., & Warren, Z. E. (2017). Interventions targeting sensory challenges in autism spectrum disorder: A systematic review. Pediatrics, 139(6), 1–22. https://doi.org/10.1542/peds.2017-0347
Werner-Seidler, A., Perry, Y., Calear, A. L., Newby, J. M., & Christensen, H. (2017). School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clinical Psychology Review, 51, 30–47. https://doi.org/10.1016/j.cpr.2016.10.005
Werner-Seidler, A., Spanos, S., Calear, A. L., Perry, Y., Torok, M., O’Dea, B., Christensen, H., & Newby, J. M. (2021). School-based depression and anxiety prevention programs: An updated systematic review and meta-analysis. Clinical Psychology Review, 89, 102079.
Whalon, K., Conroy, M., Martinez, J., & Werch, B. (2015). School-based peer-related social competence interventions for children with autism spectrum disorder: A meta-analysis and descriptive review of single case research design studies. Journal of Autism & Developmental Disorders, 45(6), 1513–1531. https://doi.org/10.1007/s10803-015-2373-1
Wilkes-Gillan, S., Cordier, R., Chen, Y. W., Swanton, R., Mahoney, N., Trimboli, C., & Tam, E. (2021). A systematic review of video-modelling interventions for children and adolescents with attention-deficit hyperactivity disorder. Australian Occupational Therapy Journal, 68(5), 454–471. https://doi.org/10.1111/1440-1630.12747
Willis, D., Siceloff, E. R., Morse, M., Neger, E., & Flory, K. (2019). Stand-alone social skills training for youth with ADHD: A systematic review. Clinical Child & Family Psychology Review, 22(3), 348–366. https://doi.org/10.1007/s10567-019-00291-3
Wright, B., Marshall, D., Adamson, J., Ainsworth, H., Ali, S., Allgar, V., & Williams, C. (2016). Social Stories™ to alleviate challenging behaviour and social difficulties exhibited by children with autism spectrum disorder in mainstream schools: Design of a manualised training toolkit and feasibility study for a cluster randomised controlled trial with nested qualitative and cost-effectiveness components. Health Technology Assessment (winchester, England), 20(6), 1.
Yap, M. B. H., Morgan, A. J., Cairns, K., Jorm, A. F., Hetrick, S. E., & Merry, S. (2016). Parents in prevention: A meta-analysis of randomized controlled trials of parenting interventions to prevent internalizing problems in children from birth to age 18. Clinical Psychology Review, 50, 138–158. https://doi.org/10.1016/j.cpr.2016.10.003
Ye, P., Huang, Z., Zhou, H., & Tang, Q. (2021). Music-based intervention to reduce aggressive behavior in children and adolescents: A meta-analysis. Medicine (baltimore), 100(4), e23894. https://doi.org/10.1097/md.0000000000023894
Yin, B., Teng, T., Tong, L., Li, X., Fan, L., Zhou, X., & Xie, P. (2021). Efficacy and acceptability of parent-only group cognitive behavioral intervention for treatment of anxiety disorder in children and adolescents: A meta-analysis of randomized controlled trials. BMC Psychiatry, 21(1), 29. https://doi.org/10.1186/s12888-020-03021-0
Zarakoviti, E., Shafran, R., Papadimitriou, D., & Bennett, S. D. (2021). The efficacy of parent training interventions for disruptive behavior disorders in treating untargeted comorbid internalizing symptoms in children and adolescents: A systematic review. Clinical Child and Family Psychology Review, 24(3), 542–552. https://doi.org/10.1007/s10567-021-00349-1
Zwi, M., Jones, H., Thorgaard, C., York, A., & Dennis, J. A. (2011). Parent training interventions for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD003018.pub
Acknowledgements
Thank you to Sharon Haarsma (NSW Dept of Health) and the “Got It!” clinicians on the Clinical Advisory Group from NSW Ministry of Health who provided input on the identification of search terms and on the results of the review.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was funded by the New South Wales Ministry of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: AM, JH, MK, LT, LR; Methodology: JH, SM, TC, AM, MK, LT, LR; Data curation: SM, TC, AM, JH, MK, LT, LR, EM, WC, YW, TS; Writing – original draft: SM; Writing – review and editing: JH: TC, AM, MK, LT, LR, EM, WC, YW, TS; Project administration: TC; Funding acquisition: AM, JH, MK, LT, LR.
Corresponding author
Ethics declarations
Conflict of interest
JH, and LT are authors on research included in the review. JH has authored treatment programs for children with anxiety and although she does not receive royalties from the sale of these programs, she received royalties from the sale of a related book. LT is an author of freely available parenting programs for children with conduct problems. MK is an author of several psychological treatment programs for children. LR and AM have previously designed and delivered group treatment programs for children and adolescents for NSW Health. No royalties have been, are currently, or will be received from these programs. AM and JH are currently funded by Australian National Health and Medical Research Council (NHMRC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hudson, J.L., Minihan, S., Chen, W. et al. Interventions for Young Children’s Mental Health: A Review of Reviews. Clin Child Fam Psychol Rev 26, 593–641 (2023). https://doi.org/10.1007/s10567-023-00443-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-023-00443-6