Abstract
Placement instability for children in foster care is high, with children experiencing nearly 4.5 placement moves per 1,000 days in care on average. While prior research has demonstrated a predictive relationship between mental health problems and placement instability, few studies have examined the associations of specific mental health diagnoses or utilization of mental health (MH) services. To this end, this study seeks to investigate associations between MH service utilization, mental health diagnosis, and placement instability (rate of placement moves) for foster children. We analyzed statewide integrated administrative data to examine MH service utilization and mental health diagnosis on placement instability among foster children. We used SAS 9.4 to conduct descriptive, bivariate, and multiple linear regression models to address the objectives of the study. The retrospective cohort was composed of 1,002 children in foster care. The multivariable linear regression reveals that receiving in-patient services, receiving out-patient services, being diagnosed with conduct disorder, being Black children, older children, and female children, being placed in intensive case management, being sexually abused, having a single household family structure at time of removal, and having a high number of intakes significantly increased the rate of placement moves. The findings of this study have significant implications for the provision of mental health services to foster children and the promotion of placement stability, highlighting the role of child welfare professionals in fostering protective factors and mitigating risk factors to promote placement stability. Implications for practice and policy improvement are discussed.
Similar content being viewed by others
More than 400,000 children are in foster care placements in the United States (U.S.) each year, with over 270,000 children entering foster care in 2021 (U.S. Department of Health and Human Services [DHHS], 2022). The majority of these children have experienced some form of abuse or neglect (DHHS, 2022), placing them at increased risk of experiencing mental health problems (Del Vecchio et al., 2012), and negative experiences while in care may exacerbate this risk. One such experience is placement instability. Placement instability refers to foster children experiencing multiple placement moves while in care (Wedeles, 2016). Unfortunately, placement instability is a common experience for children in foster care, with the average child experiencing nearly 4.5 placement moves per 1,000 days in care (Capacity Building Center for States, 2022).
Placement instability receives a great deal of attention in research, practice, and policy due to the documented consequences of high rates of placement moves for foster children. For young children, placement instability is associated with lower scores on measures of socio-emotional, cognitive, and physical development (Asif et al., 2023). Unstable placement histories have also been found to predict low academic achievement, substance use, and delinquent behavior in older youth (Pecora, 2012; Ryan & Testa, 2005; Stott, 2012). Evidence suggests that these effects are mediated by the impact of placement instability on the development of the prefrontal cortex, a region of the brain that is heavily implicated in planning, decision making, personality, and social behavior (Fisher et al., 2013).
Great strides have been made in the attempt to identify factors that predict unstable placement histories in order to tailor interventions and policies to improve stability outcomes. Individual placement moves are often made due to systemic or policy-related reasons, such as the decision to place a child at a different level of care or to place them with family members, or foster family-related reasons, such as unpredictable life events, poor parenting practices, or maltreatment allegations (Koh et al., 2014). However, there are also a range of child- and family-level factors that predict which children are most likely to experience high placement instability throughout their time in care. These include being older, being placed separately from siblings, having a history of maltreatment, parental substance abuse, being placed voluntarily, and being in traditional foster care as compared to a kinship setting (Jedwab et al., 2019; Konijn et al., 2019). Finally, one of the strongest predictors of placement instability is the presence of mental, emotional, or behavioral health problems (Konijn et al., 2019). One study of placement instability found that child behavior-related reasons accounted for 37.5% of placement moves reviewed; in most of these cases, the foster parents initiated the placement change by requesting that the child be removed due to their behaviors (Koh et al., 2014). Jedwab et al. (2019) investigated the predictive value of a range of child and family demographic characteristics for placement instability, finding that the ability of child’s behavior problems to predict placement instability was surpassed only by child’s placement in an intensive care facility. In a study of over 3,000 children in kinship or foster care in Illinois, Koh and colleagues (2014) used propensity score matching to compare children who experienced stable placements to those who had multiple placements moves. Nearly one third of children in the multiple move group received a new mental health diagnosis during the study period, compared to just 3% of the stable placement group. Similarly, Eggertsen (2008) found that the presence of a mental health diagnosis increased children’s risk for placement instability.
One potential predictor of placement instability that has received significantly less attention is mental health service utilization. Ideally, the relationship between mental health symptoms and mental health service receipt would be one-to-one such that each child receives mental health services according to their needs; however, data suggests that many children in foster care do not receive adequate mental health services to address their needs. Gudiño et al. (2012) found that in a nationally representative sample of children who were subjects of child maltreatment investigations, while 24% met clinically significant criteria for internalizing mental health problems (e.g., depression, anxiety) and 35% met criteria for externalizing problems (e.g., impulsive behavior, aggression), only 19% received any outpatient mental health treatment in the 12 months following the investigation. Similarly, Garcia and Courtney (2011) found that among 17-18-year-old foster youth in three Midwest states, only 60% of those who had a lifetime mental health diagnosis of depression, dysthymia, generalized anxiety disorder, social phobia, and/or PTSD received any mental health services within the previous year. These discrepancies between services needed and services received are even wider for racial and ethnic minorities (Garcia & Courtney, 2011; Garcia et al., 2016; Gudiño et al., 2012; Pullmann et al., 2018).
Presumably, receipt of mental health services should help to address the symptoms that increase the risk of placement disruption, decreasing the likelihood of placement instability. However, some research suggests that the mental health treatment that foster children receive is often ineffective (Bellamy et al., 2010). Furthermore, mental health service receipt may act as a proxy variable for the severity of mental health symptoms (Burns et al., 2004). Accordingly, Fawley-King and Snowden (2012) found evidence of a bi-directional association between mental health services and placement instability: placement change predicts subsequent emergency mental healthcare usage, and emergency mental healthcare usage also predicts subsequent placement change.
In order to inform strategies to increase placement stability and thus improve outcomes for foster children, it is imperative that more research is done to elucidate these associations. Additionally, while prior research has sufficiently demonstrated the existence of a predictive relationship between mental health problems and placement instability, these studies tend to consider all mental, emotional, and behavioral problems as a single predictor. The relationships between specific mental health diagnoses and placement instability are not yet well understood. Furthermore, the relationship between mental health service utilization and placement instability is understudied. The present study aims to investigate associations between mental health service utilization and mental health diagnosis on placement instability (rate of placement moves) for foster children.
Method
Data Sources
The present study used data which were integrated from three administrative data sources in a southeastern state: (1) foster care data and services from the Department of Social Services (DSS), (2) medical claims from the Department of Health and Human Services (DHHS) and Medicaid and pharmacy data from the DHHS, (3) mental health data from the Department of Mental Health (DMH). All administrative data were de-identified.
Sample Selection
A retrospective cohort of children in foster care was selected. The foster care cohort includes children: (1) who entered foster care for the first time between January 1st 2018 and December 31st 2019, (2) were between two and 17 years old at the time of entering foster care, and (3) stayed in foster care for at least 30 days.
Measures
Dependent Variable
Placement instability was constructed according to the Child and Family Services Review’s (2015) national standards. Rate of placement moves was defined as a total number of placements experienced during their time in care divided by the cumulative number of days spent in FC in 12 months. The rate of placement moves is shown by 1000 days in care.
Independent Variables
Mental health service utilization was defined as the use of various facilities, including inpatient, outpatient, school-based, and other services, number of visits, and whether the child was receiving psychotropic medications (American Psychological Association, 2023).
Mental health diagnoses were obtained from ICD9 codes (Commission on Professional and Hospital Activities, 1988). Dummy variables were created for the following mental health categories: ADHD, anxiety or depression, adjustment disorder, conduct disorder, PTSD, and other mental health disorders. Other mental health disorders may include social phobia, psychosis, bipolar disorders, and intellectual disabilities.
Covariates
Child’s sociodemographic predictors include child’s age at entry into FC (years), sex (female, male), and race/ethnicity (Black/African American, Hispanic, more than one race, Other, White/Caucasian). Other predictors related to child welfare include family of origin composition at the time of removal (Married Couple, Single [including female and male], Unmarried Couple), foster home composition at entry into care (Married Couple, Single [including female and male], Unmarried Couple), number of investigations of child abuse and neglect (continuous), children placed in intensive case management (yes, no), and region of origin (rural, urban). Dummy variables (0,1) were constructed for maltreatment types (physical abuse, neglect, abandonment, sex abuse, medical factor, Threat of Harm [TOH] factor, other maltreatment). Other maltreatment includes Contributing to the Delinquency of a Minor and Mental Injury. Threat of Harm to children in the home factors may include a prior history of domestic violence or other abuse in the home, alcohol or drug abuse if known or evident at the time of the initial contact, or other circumstances indicative of danger to the children.
Data Analysis
SAS version 9.4 (SAS Institute, Cary, NC, USA) was used to conduct descriptive (frequency, percent, median), bivariate, and multiple linear regression models to address the objectives of the study. Median values are shown instead of mean values since data for key variables is skewed. For bivariate analysis, Kruskal-Wallis Test was applied to test any significant difference between predictors and the rate of placement moves. Cohen’s d effect sizes and 95% confidence intervals were determined. For the multivariate analyses, a GENMOD procedure with a log link function and Poisson distribution was used. Log-linear modelling was used to test the association of mental health service utilization and mental health diagnosis with rate of placement moves, after adjusting for control variables. The GENMOD procedure fits a generalized linear model to the data by maximum likelihood estimation of the parameter vector β. All confounders were simultaneously entered as indicator variables into the log-linear model. A backward elimination process was used to identify confounders; those that changed the association of interest by 10% or more were retained in the final model. For instance, SNAP benefits and TANF benefits did not change the main association, hence were eliminated from the final regression model. Adjusted estimated effects of rate of placement moves were obtained. A p-value of less than 0.05 was considered statistically significant. All estimates are displayed in Rate Ratios.
We hypothesize that (1) mental health service utilization such as inpatient and outpatient mental health services is associated with placement moves in foster care; (2) mental health diagnoses are associated with a higher rate of placement moves in foster care.
Results
Descriptive and Bivariate Results
Cohort Characteristics
The retrospective cohort was composed of 1,002 children in foster care, of which 48% were female and 52% male (Table 1). The average youth’s age when entering foster care was 9 years (range: 2–17). About 33% were Black/African American children, 48% were White/Caucasian, and 7% were Hispanics. Youth in foster care were predominantly from non-rural counties (84%). Most of the foster children were removed from single female households (46%), followed by married couple units (23%). Once these children entered foster care, the primary foster home structure assigned to these children was a single female foster parent (59%), followed by unmarried couple (17%) and married couple (15%). These children experienced on average two intakes prior to entering foster care. More often these children experienced neglect (84%), TOH factor (71%), and physical abuse (50%).
Mental Health Service Utilization
About 64% of the children received any MH services, with an average of 13 mental health visits, in an average period of 35 months. Mental health services include inpatient (n = 22, 2.2%), outpatient (n = 610, 60.8%), and school-based (n = 383, 32.1%) services. Among those who received MH services, only 34% Black/African American children received MH services, while 48% were White/Caucasian.
Mental Health Diagnoses
The most common diagnosis was adjustment disorder (25.5%), followed by ADHD (16.4%). About 11% of the youth in our cohort were diagnosed with a conduct disorder and 8% were diagnosed with anxiety or depression. Seven percent were diagnosed with PTSD, and 11% were diagnosed with other mental health disorders.
Placement Instability
Youth in foster care experienced on average five different placements with a range of 1 to 44 placement moves. The rate of placement moves (5.06 moves/1000 days in care) was higher than national levels (4.48 moves/1000 days, Capacity Building Center for States, 2022).
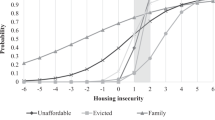
Bivariate analyses indicated that youth who have higher rates of placement moves while in foster care were significantly more likely to be older (β = 0.047, p < 0.001, data not shown). Black/African American children experienced a higher median rate of placement moves (5.78 moves/1000 days) than White/Caucasian children (4.86 moves/1000 days, p = 0.015) (Table 2). Regarding the use of MH services, those who received inpatient MH services had a higher rate of placement moves (10.64/1000 days) than those who received other MH services/none (4.93 moves/1000 days, p < 0.001). Likewise, those receiving outpatient services experienced a high rate of placement moves (6.06 moves/1000 days, p < 0.001), as well as those who received school-based services (6.16 moves/1000 days, p < 0.001). Overall, children who received any type of mental health services were more likely to experience a high rate of placement moves while in foster care (5.88 moves/1000 days, p < 0.001) than those who did not receive any mental health services.
Youth who were diagnosed with conduct disorders were more likely to experience a high rate of placement moves while in foster care (9.08 moves/1000 days, p < 0.001) than those who were not diagnosed with a conduct disorder. Likewise, those who were diagnosed with PTSD experienced a high rate of placement moves (6.43 moves/1000 days, p = 0.018), as well as those who were diagnosed with depression or anxiety (6.36 moves/1000 days, p = 0.002), adjustment disorder (5.77 moves/1000 days, p = 0.006), ADHD (6.32 moves/1000 days, p < 0.001), and other mental health diagnoses (8.21 moves/1000 days, p < 0.001).
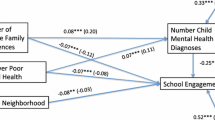
Multivariate Regression Results
Results from the log linear regression model indicated that outpatient mental health utilization was significantly associated with an increased rate of placement moves, with a rate ratio (RR) 1.12 times greater than not receiving outpatient mental health (β = 0.117, p = 0.011), after adjusting for other covariates (see results in Table 3). Likewise, receiving inpatient mental health services was also associated with higher rates of placement moves (β = 0.140, p = 0.046, RR = 1.14). However, the use of psychotropic drugs (β = -0.147, p = 0.05, RR = 0.86) was associated with reduced rates of placement moves among youth in foster care, compared to youth not using psychotropic drugs.
Regarding youth’s mental health diagnoses, those diagnosed with conduct disorder (β = 0.093, p = 0.040, RR = 1.09) experienced higher rates of placement moves, compared with those not diagnosed with a conduct disorder. A similar trend was found for children who were diagnosed with other mental health disorders (β = 0.201, p < 0.001, RR = 1.22).
Black/African Americans experienced a higher rate of placement moves (β = 0.155, p < 0.001, RR = 1.16) when compared with White/Caucasians. On the other hand, Hispanics experienced a lower rate of placement moves (β = -0.254, p < 0.001, RR = 0.77) than White/Caucasians.
Regarding youth’s characteristics, being female (β = 0.106, p < 0.001, RR = 1.11) and older (β = 0.020, p < 0.001, RR = 1.02) significantly increased the rate of placement moves. Other predictors found to be associated with increased rate of placement moves include youth placed in intensive case management (β = 0.382, p < 0.001, RR = 1.46), being sexually abused (β = 0.180, p < 0.001, RR = 1.19) and increased number of investigations of child abuse and neglect within child welfare services (β = 0.126, p < 0.001, RR = 1.13). Youth whose caregiver family structure at the time of the removal was a single household (β = 0.100, p = 0.019, RR = 1.10) or other (β = 0.136, p = 0.006, RR = 1.14) were associated with increased rate of placement moves than those with a married couple household structure.
Discussion
Overall, our findings suggest that children who received in-patient or out-patient mental health services and were diagnosed with conduct disorders were more likely to experience more placement moves. Also, this study further identified some risk and protective factors associated with placement moves. Youth in foster care in the present study experienced on average five placement moves, a placement higher than the national level of 4.48 moves/1000 days. Many foster children who were urban dwellers and removed from single-female households were assigned majorly to similar single-female household structures which increased their odds of experiencing placement instability. Foster parents’ psycho-socioeconomic status provides a major framework for psychophysiological nurturing needed for foster child placement stability (Maaskant et al., 2014). Our findings showed a range of maltreatment types (such as physical abuse and neglect) experienced by foster children upon entering foster care. This is in keeping with a study that shows many enter foster care based on a similar pattern of trauma frequency (James et al., 2004).
Over two-thirds of the foster children in our study received one or more MH service. MH service utilization is higher compared to some other studies, which show only about a third to a quarter of the foster children received mental health services; however, many of these studies only considered outpatient or inpatient MH services, while our study assessed all forms of mental health services (Larsen et al., 2018; Solerdelcoll et al., 2024). However, one of the studies corroborated an increase in MH inpatients (Solerdelcoll et al., 2024). As hypothesized, MH service utilization was associated with placement stability in our study. Foster children receiving inpatient MH services had a higher rate of placement moves than those who received any other type of MH services or no services. This finding reinforces available evidence by showing higher placement instability among those who received inpatient MH services compared to those who received other MH services or no services at all (Fawley-King & Snowden, 2012). The use of inpatient MH services or hospitalization is associated with increased placement moves; although this evidence also revealed a bidirectional relationship with placement change influencing the increased rate of inpatient MH service use (Fawley-King & Snowden, 2012). Our above findings show children who received any of the mental health services had higher chances of experiencing significant placement moves while in foster care than those who did not receive any mental health services. This could be explained by the fact that children who use mental services have more mental health problems hence leading to placement instability (Leathers et al., 2021).
Our current study has been able to establish a concurrent relationship between frequent in-patient, out-patient, and school mental health utilization and increased rate of placement moves. However, we found the use of psychotropic drugs was in keeping with reduced rates of placement moves among youth in foster care, compared to youth not using psychotropic drugs. It could be established that foster children in need of aggressive MH care may benefit more from psychotropic drugs due to their mental health comorbidities requiring pharmacotherapy (Solerdelcoll et al., 2024). However, experts recommend that a multidisciplinary approach to MH services should be applied rather than reliance on medication alone (Huefner et al., 2014).
The White/Caucasians were the major beneficiaries of MH service utilization with the Hispanic group being the least beneficiaries. This is supported by a study where White foster children received the highest annualized number of visits to outpatient services compared to the minority groups, with the lowest use found among Hispanic foster children (James et al., 2004). Lack of mental health services in Hispanic groups is further impeded by the social value, language, and immigration status of the foster children (Davidson et al., 2019). This could explain in this study why placement moves are higher in the minority cohort race compared to the majority.
Our study exposed a minority racial disparity with Hispanics experiencing the lowest placement instability while children of Black/African Americans experienced the highest rate of placement moves despite their lower population in the child welfare system compared with White/Caucasians. It is logical for the Hispanic placement move rate to be low given their low entry statistics into the child welfare system in this study; and generally, for various factors ranging from non-citizenship to cultural belief. In general, groups from the minoritized population are prone to clusters of risk factors that reduce their chances of placement stability (Davidson et al., 2019).
As stated at the beginning of our findings, our study established that slightly above a quarter of our sample was diagnosed with an adjustment disorder, followed in prevalence by ADHD diagnosis, conduct disorder, anxiety/depression, and PTSD. Our study established a high rate of placement moves among youth diagnosed with a conduct disorder compared to those without conduct disorder or another form of behavioral diagnosis while in the foster care system. Some risk factors identified as contributing to the increased amount of placement moves include the wide range of behavioral challenges at times presented by youth labeled with conduct disorders (Leathers et al., 2021). Older foster youth in who have been in foster care for a long time have a higher prevalence of conduct disorder, further bringing to bear reasons for stability among the younger foster children compared to the older age group (McMillen et al., 2005; Solerdelcoll et al., 2024). It is also notable that conduct disorder is a highly pejorative diagnosis with many clinicians avoiding this diagnosis related to negative impacts on those receiving it, including self- and other-stigmatization and exacerbation of problems related to this stigmatization (Hefflinger & Hinshaw, 2010; Jacobs et al., 2016; Weist et al., 2019).
We hypothesized that mental health diagnoses would be associated with a higher rate of placement moves in foster care. While bivariate analysis revealed that those diagnosed with PTSD, depression/anxiety, and adjustment disorder have a high rate of placement moves, these diagnoses were not related to placement stability in our multivariate analysis. However, mental health diagnoses of conduct disorder and ADHD were predictive of a higher rate of placement moves. Conduct disorder is associated with externalizing symptoms, such as disruptive and aggressive behaviors, while depression, anxiety, and adjustment disorders are more closely associated with internalizing symptoms, such as feelings of sadness or fear, decreased positive affect, and social withdrawal. Externalizing behaviors may place a higher level of strain on foster placements compared to internalizing behaviors, leading to an increased likelihood of placement disruption. Accordingly, Newton et al. (2000) found that initial externalizing behaviors, but not internalizing behaviors, predicted future placement disruption. Furthermore, in a study of placement instability for foster children in Illinois, Zinn et al. (2006) found that children with a diagnosed “pre-adult mental health disorder,” a category which they specified includes conduct disorder and ADHD, had higher odds of experiencing a placement change, while “affective disorders” and “anxiety, somatoform, dissociative, and personality disorders” were not significantly related to placement change. These findings suggest that child externalizing behaviors, and the ability and willingness of foster parents to manage these behaviors, are a driving factor in placement instability, more so than the mere presence or absence of mental health problems.
Our study contributed to the body of evidence by showing a high level of placement instability especially among older youth. Other researchers have also explained that older foster children were found to be the most affected by MH and behavioral conditions due to their long-term history of exposure to trauma (Leathers et al., 2021; McMillen et al., 2005). Another rare finding of our study is the high occurrence of placement moves in the southeastern state - an approximately 1 move/1000 days increase compared to national levels; unfortunately, there is a paucity of studies that can help explain this finding. Youths in intensive case management, a history of sexual abuse, those with another form of abuse, those neglected within the child welfare services, and with single-parent households were associated with an increased rate of placement moves. Foster child socioecological characteristics such as poor and unpredictable nurturing, and guardian’s psychological and/or drug history provide a major impact on a child’s mental health and occurrence of movement in and out of foster homes (Maaskant et al., 2014).
Strengths and Limitations
This study has several strengths to note. To begin with, we used linked administrative data from multiple state agencies to examine the association between foster children’s mental health diagnosis, use of mental health services and their placement moves. In addition, we distinguished different types of mental health services (e.g., in-patient, out-patient, and school-based mental health services) and further examined associations between the different types of mental health services and placement moves. Despite these significant strengths, this study has some limitations for consideration. Primarily, it did not establish a definitive temporal sequence in the association between mental health diagnosis, mental health service utilization and foster children’s placement moves. As prior research has indicated (Fawley-King & Snowden, 2012; McGuire et al., 2018), the link between mental health service utilization and placement stability is bidirectional. This study did not assess the influence of prior mental health service usage on subsequent placement stability in follow-up periods. Also, youth’s diagnoses were determined at entry or added over youth’s tenure in foster care. However, exact dates of the diagnoses could not be ascertained based on our data. In addition, with this current data, study design, and analyses we could not answer whether mental health services are effective at reducing mental health problems and placement instability. Another limitation is that the study’s data were solely drawn from administrative data in a specific southeastern state. Given the unique landscape of child welfare in this region, the generalizability of our findings to other states may be limited.
Directions for Future Research
Limitations of this study point to some future research directions. Future research needs to utilize longitudinal data and establish the temporal order in the association between the use of mental health services and placement stability. In addition, it would be necessary to consider the effectiveness of these mental health services (i.e., whether these mental health services reduced foster children’s mental health problems) when investigating the association between mental health service utilization and placement stability. Moreover, a crucial area for further inquiry is to investigate the underlying causes of placement moves. Conducting interviews with foster parents, foster children, and child welfare workers can offer valuable insights into the root causes of placement instability within the foster care system. This qualitative approach may help uncover systemic factors contributing to placement instability and provide a foundation for targeted interventions and policy improvements in the realm of child welfare.
Implications for Practice
The findings of this study have significant implications for the provision of mental health services to foster children and the promotion of placement stability. To begin with, our results indicate that foster children who utilize in-patient and out-patient mental health services are more likely to experience placement moves than those receiving alternative mental health interventions, such as school-based mental health services. The utilization of in-patient and out-patient mental health services suggests that these children may be grappling with more severe mental health symptoms, emphasizing the critical need to prioritize mental health services for foster children with more severe mental health needs. This correlation is further substantiated by our findings, which demonstrate a significant association between having conduct disorder and other diagnoses (e.g., bipolar disorder, alcohol use disorder) and an increased frequency of placement moves. However, it is important to note that the positive association between the use of mental health services and placement moves raises questions about the effectiveness of these services in addressing children’s mental health problems. Indeed, mental health services may have iatrogenic influences on youth, related to faulty diagnoses, inappropriate treatment (including inappropriate use of psychopharmacologic intervention), stigmatization (as reviewed earlier) and other issues (e.g., lack of empathy/respect from providers; Hefflinger & Hinshaw, 2010; Jacobs et al., 2016; Weist et al., 2019).
Furthermore, our study reveals disparities, with Black and older foster children experiencing more frequent placement moves compared to their White and younger counterparts, respectively. Additionally, children from single-parent or non-traditional household structures such as substitute care homes/facilities are more likely to undergo multiple placement moves than those from married households. Moreover, our results suggest that children receiving intensive case management are associated with a higher frequency of placement moves, implying that children with more significant trauma and needs are at an elevated risk of placement instability. These findings underscore the necessity of addressing placement moves with a specific focus on more vulnerable foster children, including Black/African American children, older children, those from single-parent or alternative household structures, and children with intensive case management experiences.
Turning to the type of child maltreatment and the number of investigations related to child maltreatment, our results indicate that children who undergo more investigations are at a heightened risk of placement moves. Furthermore, child sexual abuse and the threat of harm factor emerge as risk factors for placement moves, while experiencing other category types of child maltreatment is associated with a lower likelihood of placement moves. These findings emphasize the importance of prioritizing mental health services for children who have undergone multiple child maltreatment investigations, particularly those who have experienced sexual abuse and threats of harm. Additionally, there is an urgent need for providing trauma-informed mental health services to address the adverse effects of child maltreatment on the mental health symptoms of these children.
In our present study, we also identified that Hispanic children compared to White and children residing in married foster families, as opposed to other family arrangements, experience fewer placement moves. Further exploration is needed to understand the underlying reasons for these associations. Child welfare practitioners in our state could benefit from focusing more attention on children in these foster families and identifying protective mechanisms that promote placement stability.
Conclusion
This study examines the association between the use of mental health services, mental health diagnosis, and placement moves among foster children using linked administrative data in a southeastern state. Results first suggest using in-patient and out-patient mental health services is positively associated with more placement moves, and further identify some risk and protective factors associated with placement moves. While the results may question the effectiveness of current mental health services provided to foster children, they underscore the importance of providing effective and tailored mental health services to foster children to enhance placement stability. Furthermore, these results highlight the role of child welfare professionals in fostering protective factors and mitigating risk factors to promote placement stability in practice and policymaking.
References
American Psychological Association. APA dictionary of psychology Retrieved September 10 (2023). from https://dictionary.apa.org/mental-health-services.
Asif, N., Breen, C., & Wells, R. (2023). Influence of placement stability on developmental outcomes of children and young people in out-of-home care: Findings from the pathways of Care longitudinal study. Child Abuse & Neglect. https://doi.org/10.1016/j.chiabu.2023.106145.
Bellamy, J. L., Gopalan, G., & Traube, D. E. (2010). A national study of the impact of outpatient mental health services for children in long-term foster care. Clinical Child Psychology and Psychiatry, 15(4), 467–479. https://doi.org/10.1177/1359104510377720.
Burns, B. J., Phillips, S. D., Wagner, H. R., Barth, R. P., Kolko, D. J., Campbell, Y., & Landsverk, J. (2004). Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child & Adolescent Psychiatry, 43(8), 960–970. https://doi.org/10.1097/01.chi.0000127590.95585.65.
Capacity Building Center for States (2022). Placement stability: CFSR round 4 statewide data indicator series Children’s Bureau, Administration for Children and Families, U.S. Department of Health and Human Services. Retrieved September 10, 2023, from https://capacity.childwelfare.gov/states/resources/cfsr-r4-swdi-placement-stability.
Commission on Professional and Hospital Activities. (1988). The international classification of diseases, ninth revision, clinical modification. Medicode Inc.
Davidson, R., Morrissey, M., & Beck, C. (2019). The hispanic experience of the child welfare system. Family Court Review, 57(2), 201–221. https://doi.org/10.1111/fcre.12404.
Del Vecchio, T., Slep, A. M. S., & Heyman, R. E. (2012). Psychological, physical, and economic consequences of child maltreatment. In S. R. H. Beach, R. E. Heyman, A. S. Slep, H. M. Foran, & M. Z. Wamboldt (Eds.), Family problems and family violence: Reliable assessment and the ICD-11 (pp. 149–157). Springer.
Department of Health and Human Services (2022). The AFCARS reporthttps://www.acf.hhs.gov/sites/default/files/documents/cb/afcars-report-29.pdf.
Eggertsen, L. (2008). Primary factors related to multiple placements for children in out-of-home care. Child Welfare, 87, 71–90. https://www.jstor.org/stable/48623138.
Fawley-King, K., & Snowden, L. R. (2012). Relationship between placement change during foster care and utilization of emergency mental health services. Children and Youth Services Review, 34(2), 348–353. https://doi.org/10.1016/j.childyouth.2011.11.002.
Fisher, P. A., Mannering, A. M., Van Scoyoc, A., & Graham, A. M. (2013). A translational neuroscience perspective on the importance of reducing placement instability among foster children. Child Welfare, 92(5), 9–36. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4396742/.
Garcia, A., & Courtney, M. (2011). Prevalence and predictors of service utilization among racially and ethnically diverse adolescents in foster care diagnosed with mental health and substance abuse disorders. Journal of Public Child Welfare, 5(5), 521–545.
Garcia, A. R., Kim, M., & DeNard, C. (2016). Context matters: The state of racial disparities in mental health services among youth reported to child welfare in 1999 and 2009. Children and Youth Services Review, 66, 101–108. https://doi.org/10.1016/j.childyouth.2016.05.005.
Gudiño, O. G., Martinez, J. I., & Lau, A. S. (2012). Mental health service use by youths in contact with child welfare: Racial disparities by problem type. Psychiatric Services, 63(10), 1004–1010. https://doi.org/10.1176/appi.ps.201100427.
Hefflinger, C. A., & Hinshaw, S. P. (2010). Stigma in child and adolescent mental health services research: Understanding professional and institutional stigmatization of youth with mental health problems. Administration and Policy in Mental Health and Mental Health Services Research, 37(1–2), 61–70. https://doi.org/10.1007/s10488-010-0294-z.
Huefner, J. C., Grifth, A. K., Smith, G. L., Vollmer, D. G., & Leslie, L. K. (2014). Reducing psychotropic medications in an intensive residential treatment center. Journal Child Family Studies, 23, 675–685. https://doi.org/10.1007/s10826-012-9628-7.
Jacobs, M., Downie, H., Kidd, G., Fitzsimmons, L., Gibbs, S., & Melville, C. (2016). Mental health services for children and adolescents with learning disabilities: A review on experiences of service users and providers. British Journal of Learning Disabilities, 44(3), 225–232. https://doi.org/10.1111/bld.12141.
James, S., Landsverk, J., Slymen, D. J., & Leslie, L. K. (2004). Predictors of outpatient mental health service use—the role of foster care placement change. Mental Health Services Research, 6(3), 127–141. https://doi.org/10.1023%2Fb%3Amhsr.0000036487.39001.51.
Jedwab, M., Xu, Y., Keyser, D., & Shaw, T. V. (2019). Children and youth in out-of-home care: What can predict an initial change in placement? Child Abuse & Neglect, 93, 55–65. https://doi.org/10.1016/j.chiabu.2019.04.009.
Koh, E., Rolock, N., Cross, T. P., & Eblen-Manning, J. (2014). What explains instability in foster care? Comparison of a matched sample of children with stable and unstable placements. Children and Youth Services Review, 37, 36–45. https://doi.org/10.1016/j.childyouth.2013.12.007.
Konijn, C., Admiraal, S., Baart, J., van Rooij, F., Stams, G., Colonnesi, C., Lindauer, R., & Assink, M. (2019). Foster care placement instability: A meta-analytic review. Children and Youth Services Review, 96, 483–499. https://doi.org/10.1016/j.childyouth.2018.12.002.
Larsen, M., Baste, V., Bjørknes, R., Myrvold, T., & Lehmann, S. (2018). Services according to mental health needs for youth in foster care? A multi-informant study. BMC Health Services Research, 18, 634. https://doi.org/10.1186/s12913-018-3365-6.
Leathers, S. J., Voort, V., B. L., & Melka-Kafer, C. (2021). Mental health services and psychotropic medications provided to children at risk for placement instability in foster care. Developmental Child Welfare, 3, 256–281. https://doi.org/10.1177/25161032211034255.
Maaskant, A. M., van Rooij, F. B., & Hermanns, J. M. A. (2014). Mental health and associated risk factors of Dutch school aged foster children placed in long-term foster care. Child and Youth Services Review, 44, 207–216.
McGuire, A., Cho, B., Huffhines, L., Gusler, S., Brown, S., & Jackson, Y. (2018). The relation between dimensions of maltreatment, placement instability, and mental health among youth in foster care. Child Abuse and Neglect, 86, 10–21. https://doi.org/10.1016/j.chiabu.2018.08.012.
McMillen, C. J., Zima, B. T., Scott, L. D., Auslander, W. F., Munson, M. R., Ollie, M. T., & Spitznagel, E. L. (2005). Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child and Adolescent Psychiatry, 44(1), 88–95. https://doi.org/10.1097/01.chi.0000145806.24274.d2.
Newton, R. R., Litrownik, A. J., & Landsverk, J. A. (2000). Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse & Neglect, 24(10), 1363–1374. https://doi.org/10.1016/S0145-2134(00)00189-7.
Pecora, P. (2012). Maximizing educational achievement of youth in foster care and alumni: Factors associated with success. Children and Youth Services Review, 34(6), 1121–1129. https://doi.org/10.1016/j.childyouth.2012.01.044.
Pullmann, M. D., Jacobson, J., Parker, E., Cevasco, M., Uomoto, J. A., Putnam, B. J., & Kerns, S. E. (2018). Tracing the pathway from mental health screening to services for children and youth in foster care. Children and Youth Services Review, 89, 340–354. https://doi.org/10.1016/j.childyouth.2018.04.038.
Ryan, J. P., & Testa, M. F. (2005). Child maltreatment and juvenile delinquency: Investigating the role of placement and placement instability. Children and Youth Services Review, 27(3), 227–249. https://doi.org/10.1016/j.childyouth.2004.05.007.
Solerdelcoll, M., Ilzarbe, D., Fortea, A., Morer, A., Lazaro, L., Sugranyes, G., & Baeza, I. (2024). Psychopathology and mental health service use among youth in foster care admitted to a psychiatric inpatient unit: A 4-year retrospective controlled study. European Child and Adolescent Psychiatry, 33, 39–50. https://doi.org/10.1007/s00787-022-02104-5.
Stott, T. (2012). Placement instability and risky behavior of youth aging out of foster care. Child and Adolescent Social Work Journal, 29(1), 61–83. https://doi.org/10.1007/s10560-011-0247-8.
Wedeles, J. (2016). Ontario Association of Children’s Aid Societies. Placement stability in child welfare Retrieved October 1, 2023, from https://www.oacas.org/wp-content/uploads/2016/08/PARTicle-Placement-Stability-in-Child-Welfare-FINAL.pdf.
Weist, M. D., Shapiro, C., Hartley, S., Bode, A., Miller, E., Huebner, S., & Terry, J., Hills, K., & Osher, D. (2019). Assuring strength- and evidence-based approaches in child, adolescent, and school mental health. In D. Osher, R. Jagers, K. Kendziora, M. Mayer, & L. Wood (Eds.), Keeping students safe and helping them thrive: A collaborative handbook for education, safety and justice professionals, families, and communities (Vol. 2, pp. 54–79). Praeger.
Zinn, A., DeCoursey, J., Goerge, R. M., & Courtney, M. E. (2006). A study of placement stability in Illinois Chapin Hall Center for Children. Retrieved September 12, 2023, from https://eric.ed.gov/?id=ED501018.
Funding
This research was supported by the University of South Carolina, the Office of the Vice President for Research Advanced Support for Innovative Research Excellence I: Innovation Fund (Grant number: USCIP 80,004,413).
Open access funding provided by the Carolinas Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soto-Ramírez, N., Xu, Y., Martin, T. et al. Associations of Mental Health Service Utilization and Mental Health Diagnosis with Placement Instability Among Foster Children in a Southeastern State. Child Adolesc Soc Work J (2024). https://doi.org/10.1007/s10560-024-00962-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s10560-024-00962-3