Abstract
Purpose
This study aims to assess the association between body mass index (BMI) and platelet reactivity in STEMI patients treated with oral 3rd generation P2Y12 inhibitors.
Methods
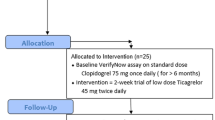
Overall, 429 STEMI patients were enrolled in this study. Patients were divided into two groups according to BMI (BMI < 25 vs ≥ 25 kg/m2). A propensity score matching (1:1) was performed to balance potential confounders in patient baseline characteristics. Platelet reactivity was assessed by VerifyNow at baseline and after 3rd generation P2Y12 inhibitor (ticagrelor or prasugrel) loading dose (LD). Blood samples were obtained at baseline (T0), 1 h (T1), 2 h (T2), 4–6 h (T3), and 8–12 h (T4) after the LD. High on-treatment platelet reactivity (HTPR) was defined as a platelet reactivity unit value ≥ 208 units.
Results
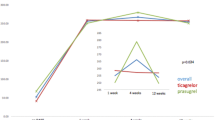
After propensity score matching, patients with BMI ≥ 25 had similar values of baseline platelet reactivity, while they had higher level of platelet reactivity at 1 and 2 h after the LD and higher rate of HRPT. Furthermore, multivariate analysis demonstrated that BMI ≥ 25 was an independent predictor of HTPR at 2 h (OR 2.01, p = .009). Conversely, starting from 4 h after the LD, platelet reactivity values and HRPT rates were comparable among the two study groups.
Conclusions
A BMI ≥ 25 kg/m2 is associated with delayed pharmacodynamic response to oral 3rd generation P2Y12 inhibitor LD, and it is a strong predictor of HTPR in STEMI patients treated by dual antiplatelet therapy with ticagrelor or prasugrel.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, GP, upon reasonable request.
References
Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213–60.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
van der Sangen NMR, Rozemeijer R, Chan P, Yin DRPP, et al. Patient-tailored antithrombotic therapy following percutaneous coronary intervention. Eur Heart J. 2021;42(10):1038–46.
Parodi G, Marcucci R, Valenti R, et al. High on treatment platelet reactivity after clopidogrel loading and long-term cardiovascu- lar events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215–23.
Scudiero F, Zocchi C, De Vito E, et al. Relationship between CHA2DS2-VASc score, coronary artery disease severity, residual platelet reactivity and long-term clinical outcomes in patients with acute coronary syndrome. Int J Cardiol. 2018;262:9–13.
Mourikis P, Zako S, Dannenberg L, et al. Aspirin antiplatelet effects are associated with body weight. Vascul Pharmacol. 2020;125–126:106635.
Norgard NB, Monte SV, Fernandez SF, Ma Q. Aspirin responsiveness changes in obese patients following bariatric surgery. Cardiovasc Ther. 2017;35(4). https://doi.org/10.1111/1755-5922.12268.
Parodi G, Valenti R, Bellandi B, et al. Comparison of prasugrel and ticagrelor loading doses in ST-segment elevation myocardial infarction patients: RAPID (Rapid Activity of Platelet Inhibitor Drugs) primary PCI study. J Am Coll Cardiol. 2013;61(15):1601–6.
Parodi G, Bellandi B, Valenti R, et al. Comparison of double (360 mg) ticagrelor loading dose with standard (60 mg) prasugrel loading dose in ST-elevation myocardial infarction patients: the Rapid Activity of Platelet Inhibitor Drugs (RAPID) primary PCI 2 study. Am Heart J. 2014;167(6):909–14.
Parodi G, Xanthopoulou I, Bellandi B, et al. Ticagrelor crushed tablets administration in STEMI patients: the MOJITO study. J Am Coll Cardiol. 2015;65(5):511–2.
Parodi G, Talanas G, Mura E, et al. Orodispersible ticagrelor in acute coronary syndromes: the TASTER study. J Am Coll Cardiol. 2021;78(3):292–4.
Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984–1010.
Canonico ME, Sanna GD, Siciliano R, et al. Not-high before-treatment platelet reactivity in patients with STEMI: prevalence, clinical characteristics, response to therapy and outcomes. Platelets. 2021;15:1–8. https://doi.org/10.1080/09537104.2021.1915973.
Garcia-Garcia HM, McFadden EP, Farb A, et al. Academic Research Consortium. Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. 2018;137(24):2635–50.
Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–64.
Burrai F, Sanna GD, Moccia E, et al. Beneficial effects of listening to classical music in patients with heart failure: a randomized controlled trial. J Card Fail. 2020;26(7):541–9.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105.
Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167(16):1720–8.
Tune JD, Goodwill AG, Sassoon DJ, Mather KJ. Cardiovascular consequences of metabolic syndrome. Transl Res. 2017;183:57–70.
Scudiero F, Valenti R, Marcucci R, et al. Platelet reactivity in hepatitis C virus-infected patients on dual antiplatelet therapy for acute coronary syndrome. J Am Heart Assoc. 2020;9(18):e016441.
Neergaard-Petersen S, Hvas AM, Kristensen SD, Grove EL. Platelets and antiplatelet therapy in patients with coronary artery disease and diabetes. Semin Thromb Hemost. 2016;42(3):234–41.
Badimon L, Hernández Vera R, Padró T, Vilahur G. Antithrombotic therapy in obesity. Thromb Haemost. 2013;110:681–8.
Janson B, Thursky K. Dosing of antibiotics in obesity. Curr Opin Infect Dis. 2012;25:634–49.
Schilling U, Dingemanse J, Ufer M. Pharmacokinetics and pharmacodynamics of approved and investigational P2Y12 receptor antagonists. Clin Pharmacokinet. 2020;59(5):545–66.
Butler K, Teng R. Pharmacokinetics, pharmacodynamics, and safety of ticagrelor in volunteers with severe renal impairment. J Clin Pharmacol. 2012;52:1388–98.
Small DS, Wrishko RE, Ernest CS, Ni L, Winters KJ, Farid NA, et al. Prasugrel pharmacokinetics and pharmacodynamics in subjects with moderate renal impairment and end-stage renal disease. J Clin Pharm Ther. 2009;34:585–94.
Pankert M, Quilici J, Loundou AD, et al. Impact of obesity and the metabolic syndrome on response to clopidogrel or prasugrel and bleeding risk in patients treated after coronary stenting. Am J Cardiol. 2014;113(1):54–9.
Mayer K, Orban M, Bernlochner I, et al. Predictors of antiplatelet response to prasugrel during maintenance treatment. Platelets. 2015;26(1):53–8.
Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–15.
Alexopoulos D, Xanthopoulou I, Storey RF, Bliden KP, Tantry US, Angiolillo DJ, Gurbel PA. Platelet reactivity during ticagrelor maintenance therapy: a patient-level data meta-analysis. Am Heart J. 2014;168(4):530–6.
Wells B, Gentry M, Ruiz-Arango A, Dias J, Landolfo CK. Relation between body mass index and clinical outcome in acute myocardial infarction. Am J Cardiol. 2006;98(4):474–7.
Schüpke S, Neumann FJ, Menichelli M, ISAR-REACT 5 Trial Investigators, et al. Ticagrelor or prasugrel in patients with acute coronary syndromes. N Engl J Med. 2019;381(16):1524–34.
Henrich A, Claussen CH, Dingemanse J, Krause A. Pharmacokinetic/pharmacodynamic modeling of drug interactions at the P2Y12 receptor between selatogrel and oral P2Y12 antagonists. CPT Pharmacometrics Syst Pharmacol. 2021;10(7):735–47.
Acknowledgements
The authors are indebted to the Cath Lab staff and the CCU fellows and nurses for their precious help in collecting and processing blood samples.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Fernando Scudiero, Mario Enrico Canonico, and Guido Parodi. The first draft of the manuscript was written by Fernando Scudiero and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
Prof. Guido Parodi reported receiving consulting or lecture fees from AstraZeneca, Bayer, Chiesi, Daiichi Sankyo/Eli Lilly, and Merck Sharp Dohme. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Supplementary Figure 1.
histogram of BMI distribution in the enrolled patients (PNG 574 KB)

Supplementary Figure 2.
Scattered plots depicting PRU values according to BMI (PNG 1.17 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Scudiero, F., Canonico, M.E., Sanna, G.D. et al. Dual Antiplatelet Therapy with 3rd Generation P2Y12 Inhibitors in STEMI Patients: Impact of Body Mass Index on Loading Dose–Response. Cardiovasc Drugs Ther 37, 695–703 (2023). https://doi.org/10.1007/s10557-022-07322-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-022-07322-2