Abstract
Aim
The COVID-19 disease primarily affects the respiratory system; however, cardiac involvement has been documented in the acute phase. We aimed to evaluate the cardiac autonomic function and subtle left ventricular dysfunction in those subjects recovered from mild to moderate acute COVID-19 patients but still symptomatic.
Methods and results
The study group was composed of 50 subjects with confirmed mild to moderate COVID-19. All subjects underwent routine 2D echocardiography assessment in addition to 2D speckle tracking and 24 h Holter monitoring for HRV analysis. The mean age of the study population was 42 ± 18 years; symptoms were reported as follows 27 (54%) had dyspnoea, 17 (34%) had palpitation, and 7 (14%) had dizziness. Time domain parameters Standard Deviation of NN intervals (SDNN), Standard Deviation of the Average NN intervals for each 5 min segment of a 24 h HRV recording (SDANN), and Root Mean Square of Successive RR interval Differences (rMSSD) were diminished with mean SDNN value being markedly impaired in 12 (24%) patients, while frequency domain parameters as assessed by the ratio of the Low-Frequency band power to the High-Frequency band power (LF/HF) with the mean of 1.837 with 8% of the patients being impaired. SDNN was significantly reduced in patients with impaired global longitudinal strain (p 0.000). The global longitudinal strain was diminished in 10 patients (20%); also, 80% of the patients with impaired GLS had decreased SDNN.
Conclusion
Our study targeted patients experiencing prolonged symptoms after COVID-19 illness. We detected a high incidence of GLS impairment using Speckle Tracking Echocardiography (STE) and a significant prevalence of diminished HRV. HRV (especially SDNN) and GLS were found to be significantly correlated.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the respiratory tract is the primary target of the Coronavirus disease 2019 (COVID-19), cardiovascular involvement has been documented in the acute stages of the disease [1]. cardiovascular involvement has been in the form of myocarditis, myocardial ischemia, heart failure, and thromboembolic manifestation [2]. Many patients recover entirely from COVID-19; however, some patients still complain of diverse symptoms such as palpitations, dyspnea on exertion, fatigue, dizziness, and headache, which goes with altered autonomic functions and underlying cardiac affection [3]. The acute manifestation of COVID-19 has been widely studied and researched; however, the post-COVID-19 sequela needs further investigation.
HRV indices
It has been suggested that this virus may affect the brain cells and the hypothalamic pituitary adrenal axis, which may cause altered autonomic functions [4]. Since then, we found that the heart rate variability with its indices has been a reliable and validated method for quantitatively assessing the sympathetic and parasympathetic nervous systems. It is also well known that decreased HRV correlates with an increased risk of cardiovascular death and all-cause mortality [5]. So, we aimed to study the HRV and the autonomic functions in recovered COVID-19 patients who had mild to moderate acute COVID-19 infection within 12 weeks from the active infection since most studies studied the autonomic dysfunction in the period of acute infection.
Echocardiographic evaluation
Since myocardial injury secondary to COVID-19 is associated with poor prognosis during acute COVID-19 infection [6], it is unclear whether this myocardial insult may have short-term or long-term sequelae, especially in patients who continue to be symptomatic despite the clearance of the viral infection [7]. Cardiac MRI revealed that up to 90% of the patients continue to have myocardial edema and inflammation after COVID-infection [8]. 2D-STE can detect subclinical myocardial dysfunction earlier than the conventional 2D echo in symptomatic post-COVID-19 patients. So, we aimed to study the subtle LV dysfunction in those patients, its correlation with the symptoms, and HRV indices as assessed by the 24-h Holter monitoring.
Patients and methods
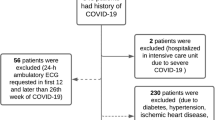
We included fifty consecutive subjects between 17 and 82 years of age who were symptomatic after three weeks up to three months of experiencing mild to moderate COVID-19 illness, according to the National Institutes of Health, United States (NIH). Patients enrolled were coming for follow-up clinic visits at Ain Shams University hospitals between June 2021–June 2022. [10].
COVID-19 diagnosis was confirmed using real-time reverse-transcriptase polymerase chain reaction assays on nasopharyngeal swabs or typical symptoms of COVID-19 in addition to high/very high suspicion (CO-RADS 4 or 5) of COVID-19 on High-Resolution Computed Tomography of the chest (HRCT Chest), or both [9].
Inclusion criteria
-
1.
Successive 50 symptomatic patients presented after mild to moderate COVID-19 illness, according to the NIH [10].
-
2.
The selected symptoms for inclusion were tiredness, fatigue, dizziness, palpitations, chest pain, and shortness of breath.
Exclusion criteria
-
1.
Patients with a history of severe or critical COVID-19 illness according to the NIH [10] or hospitalized in ICU, multiple organ failure, or needed domiciliary oxygen for the index COVID-19 infection or with active infection; within 14 days from symptom onset or PCR positive result.
-
2.
Those with a history of myocardial infarction, previous PCI, or coronary artery bypass graft (CABG),
-
3.
Those with known lung disease, LVEF < 55%, or segmental wall motion abnormalities.
-
4.
Those with arrhythmias, LBBB, RBBB, or cardiac pacemakers.
-
5.
Any known type of cardiomyopathies or valvular heart diseases.
-
6.
Those with thyroid dysfunction and chronic renal disease (GFR < 60 mL/min/1.73 m2), malignancy, or use of cardiotoxic-related medications.
-
7.
Patients with poor 2D image quality.
After written informed consent from the subjects or their guardians and approval of Ain Shams ethical committee was obtained.
Detailed history taking and full clinical examination were done, followed by 2D conventional echocardiography and 24-h Holter monitoring.
2D Echocardiographic image acquisition and analysis of the LV-GLS [11]
Transthoracic 2D echocardiography was done by an experienced cardiologist having the patient in a supine position using M5Sc-D [1.4–4.6 MHz] probe with a “GE Vivid E95” echocardiography machine.
Standard images were obtained in the parasternal (long- and short-axis views) and apical (2, 3,4, and 5-chamber images) views.
Standard 2D and color Doppler data were saved in cine-loop format and triggered to the QRS complex.
M-mode, 2D, and pulsed and continuous Doppler flow across the different heart valves in all the standard views were done according to the American Society of Echocardiography recommendations.
The following measurements were focused on: Assessment of LV systolic function by M mode, MAPSE (Mitral Annular Plane Systolic Excursion), and modified Simpson's Method (the endocardium was traced in the end diastole and end systole in the apical four chambers and two chambers views), LA/Ao dimension by M-mode, Wall motion abnormality (any patient with resting segmental wall motion abnormalities was excluded from the study), assessment of LV diastolic function using pulsed-wave Doppler and TDI on the mitral annulus.
Digital loops of multiple ECG- gated entire cardiac cycles of the LV were acquired from apical 2-, 3-, and 4-chambers.
Peak Global longitudinal strain (GLS) was analyzed using computer software for tissue tracking; EchoPAC Dimension [12.0, General Electrics (GE) Medical Systems GmbH, Germany].
This software recorded peak systolic longitudinal strain for each myocardial segment. The strain values for all the segments are recorded and averaged to obtain the global longitudinal strain (GLS). A topographic representation of the regional and global longitudinal strain of all 17 analyzed segments (Bull's eye configuration) was then automatically generated, Fig. 1.
According to the latest American Echocardiography Association guidelines, for LVGLS, above − 18% is defined as normal, − 16% − 18% as gray zone, and under − 16% as diminished. [11].
Twenty-seven patients underwent LVEF assessment before the COVID infection, using 2D and M-mode, and all had LVEF > 55%.
Holter monitoring & HRV parameters
Twenty-four hours of Holter monitoring was performed on all patients on the same day as the echocardiography, using the “CONTEC TLC9803” Dynamic 3-channel ECG Holter monitor. HRV was evaluated using time-domain and frequency-domain parameters.
Time-domain parameters included were: SDNN (Standard Deviation of NN intervals), SDANN (Standard Deviation of Average of NN intervals), and RMSSD (Root Mean Square of Successive Differences between adjacent NNs), all measured in milliseconds (msec).
Frequency-domain parameters included were: LF (Low Frequency) measured in squared milliseconds (msec " HRV data analysis in the study population :"), HF (High Frequency) measured in msec "HRV data analysis in the study population :", and LF/HF ratio.
The SDNN, SDANN, and SDNN Index are obtained from long-term records and represent the sympathetic and parasympathetic activity, but they do not allow distinguishing when changes in HRV are due to increased sympathetic tone or the withdrawal of vagal tone. The rMSSD represents the parasympathetic activity as they are found from the analysis of adjacent RR intervals.
SDNN values predict both morbidity and mortality. Based on 24 h monitoring, patients with SDNN values below 50 ms are classified as unhealthy, 50–100 ms have compromised health, and those above 100 ms are healthy [12]. RMSSD > 40 indicates parasympathetic predominance [13].
On the other hand, the High-Frequency component (HF) corresponds to respiratory modulation and is an indicator of the performance of the parasympathetic vagal innervation in the heart. In comparison, the Low-Frequency component (LF) is due to the combined action of the vagal and sympathetic components on the heart, with a predominance of the sympathetic ones.
The LF/HF ratio reflects the absolute and relative changes between the sympathetic and parasympathetic components of the autonomic nervous system by characterizing the sympathetic vagal balance on the heart.
LF/HF below 1.5 indicates parasympathetic predominance, while above 2 indicates sympathetic predominance [12, 13].
24-h Holter data were also evaluated for arrhythmias, including atrial fibrillation, atrial flutter, supraventricular tachycardia, frequent premature ventricular contractions (defined as ≥ 10% premature ventricular contractions on 24-h Holter recording), ventricular tachycardia, ventricular fibrillation, and atrioventricular block (second degree or higher).
Most patients were not on specific medications; however, 12 patients were hypertensive, taking angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB).
Statistics
Data were collected, revised, coded, and entered into the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations, and ranges when parametric and median, and inter-quartile range (IQR) when data was found non-parametric. Also, qualitative variables were presented as numbers and percentages.
The comparison between groups regarding qualitative data was done using the Chi-square test and/or Fisher exact test when the expected count in any cell was less than 5.
One way ANOVA (analysis of variance) test was used to compare more than two groups regarding quantitative variables. Spearman correlation coefficients were used to assess the correlation between two quantitative parameters in the same group. The receiver operating characteristic curve (ROC) was used to determine the best cut-off point with its sensitivity, specificity, positive predictive value, negative predictive value, and area under the curve (AUC) of the studied marker.
Results
Our study included a total of 50 patients with a mean age of 42, and 76% were male as opposed to 24% females, where the most common symptom was fatigue (82%) followed by Dyspnea (54%). Table 1 includes demographic data, cardiovascular risk factors, post-COVID symptoms, and echocardiographic data, including global longitudinal strain in the study population.
Left ventricle Global Longitudinal Strain by Speckle Tracking Echocardiography and its correlation with the Holter parameters:
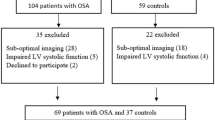
Twenty-nine of our patients (58%) had normal GLS, eleven patients (22%) were in the grey zone with a GLS between − 18 to–16%, ten patients (20%) had a diminished GLS below -16% as shown in Fig. 2.
Regarding post-COVID symptoms, Only dyspnea was found to be statistically significant in patients with impaired GLS (P value = 0.029), also GLS value was found to be significantly lower in the elderly patients (p-value = 0.001), diabetics (p-value 0.003) and hypertensive patients (p-value 0.002) as shown in Table 2.
Regarding Holter parameters, there is a statistical significance between SDNN, SDANN, and GLS, as 80% of the patients with impaired GLS have decreased SDNN, and 79% of the patients with impaired GLS have decreased SDANN (Table 2). The ROC curve analysis failed to point out a significant relation between LVGLS and the other HRV parameters except for SDNN and SDANN. However, using Spearman's correlation coefficient analysis, GLS values were plotted against the values of all HRV parameters. GLS was positively correlated to rMSSD, LF, and LF/HF ratio with p values 0.031, 0.013, and 0.029, respectively (Figs. 3, 4 & 5). GLS showed a positive correlation with SDNN with a p-value of 0.003 (Fig. 6).
P-value > 0.05: Non significant (NS); P-value < 0.05: Significant (S); P-value < 0.01: highly significant (HS) *: Chi-square test; •: One Way ANOVA test; ‡: Kruskal Wallis test.
HRV indices and its correlation with risk factors, symptoms, and global longitudinal strain
SDNN: SDNN was below 100 ms in 12 patients (24%), while 38 had an SDNN above 100. No patients were reported to have an SDNN below 50; therefore, there were no patients with severely impaired HRV, as illustrated in Fig. 7.
In the study population, SDNN was significantly impaired in the elderly and diabetic patients, p values 0.001 and 0.007, respectively. There was a statistically significant increase in the percentage of female patients with SDNN < 100 ms (50%) than with SDNN > 100 ms (only 15.8%). The correlation of presenting post-COVID symptoms to HRV measured by SDNN was highly significant to palpitation as the presenting symptom. However, no other symptom was correlated to SDNN, as shown in Table 3.
Analysis of SDNN and echocardiographic data showed a highly significant relation between impaired SDNN and impaired GLS with a p-value of 0.001, as shown in (Table 3). SDNN values were also plotted against GLS values showing a positive correlation between both, as shown in Fig. 8. Other echocardiographic parameters were not significantly related to SDNN.
While analysis of rMSSD with a value below 40 ms was not significantly correlated with any of the echocardiographic data.
Analysis of the LF/HF ratio showed that 38% of the study population had LF/HF ratio below 1.5, as shown in Fig. 9. There was no association between LF/HF and post-COVID symptoms. However, DM and increased age were statistically significant as none of the diabetic patients had an LF/HF ratio > 2 with a p-value of 0.006. Also, there was a negative linear correlation between the LF/HF ratio and age, i.e., the older the age, the lower the LF/HF ratio, as seen in Fig. 10. There was no statistical significance between the LF/HF ratio and any 2D echocardiographic data or the GLS. However, Spearman’s correlation coefficient analysis revealed a positive correlation between LF/HF ratio and GLS, as illustrated in Fig. 11.
Discussion
Our study included fifty consecutive symptomatic patients with a history of mild to moderate COVID-19 illness after four weeks up to 3 months from the symptom onset with positive PCR results. Severe and critically ill patients were excluded as well as patients who were admitted to the ICU or needed non-invasive or invasive ventilation.
Prevalence of post-COVID symptoms in the study population
We found that the most common symptom was fatigue followed by dyspnea, then palpitations. With the least reportesd symptoms chest pain and dizziness respectively.
Like our study, Pavli et al. reported that fatigue was the most commonly experienced symptom, with an incidence ranging from 17.5 to 63%. The second most common symptom was dyspnea and exercise intolerance, with an incidence rate of 10 to 40%. Chest pain affected up to 22% of patients [14].
Moreover, a systemic review held by Alhumayn et al. revealed similar results. Fatigue and sleep disturbances were reported in two-thirds of the patients, with an incidence of 73% and 85%, respectively, followed by dyspnea, with an incidence of 64% [15].
The main findings in our study are as follows (1) impaired LVGLS was detected in one-fifth of the symptomatic post-COVID patients; however, they had normal baseline LV systolic functions. (2) HRV data analysis using time and frequency domains showed that autonomic dysfunction was prevalent, as 24% of the patients had decreased SDNN. This autonomic dysfunction was related to decreased parasympathetic activity, as there was a higher rMSSD < 40 ms prevalence and LF/HF ratio > 2 in the study population. (3) There was a significant correlation between impaired SDNN and impaired GLS as patients with decreased SDNN had lower LVGLS -15.74 ± 2.61% compared to those with normal SDNN with LVGLS -18.81 ± 1.95.
Prevalence of impaired GLS in the study population:
LVGLS was significantly impaired in elderly patients and those with DM&HTN in our post-COVID cohort. This could be explained by the relation between LVGLS impairment, and these factors irrelevant to COVID-19 or that COVID-19-induced subtle LV dysfunction was more evident in these subgroups.
Consistent with the data in the current study, Mahajan et al. reported that Impaired LVGLS was recorded in 1 (7.7%), 8 (13.1%), and 22 (44%) subjects with asymptomatic, mild, and moderate COVID-19 illness respectively. They concluded that one-third of the study population had impaired GLS. However, in contrast to our study, Mahajan included patients with severe COVID-19 illness, and 99% of the ten patients had impaired GLS, thus significantly contributing to the high incidence of impaired GLS among this study group [16].
In addition, Özer et al. found that one of third of the patients had impaired LVGLS after one month of acute COVID-19 illness using a cut-off value of < − 18%. Seventy-four out of 124 patients were selected after applying the exclusion criteria [17].
Turan et al. found that the absolute value of LVGLS was significantly lower in the COVID-19 group than in healthy controls (19.17 ± 2.65 vs. 20.07 ± 2.19, p = 0.03) [18].
Contrary to the data in our study, LVGLS was found to be normal by Caiado et al., who conducted a case–control study of 100 post-COVID patients. However, there was an affection of the basal segments' longitudinal strain with a mean of − 16.48 ± 5.41%. Most of them were asymptomatic and mildly symptoms (83%), five patients only had moderate symptoms needing hospitalization, and only 46% of the enrolled populations had post-COVID symptoms [19].
The underlying mechanisms of impaired GLS in post-COVID patients may be attributed to the following mechanisms:- First, direct myocardial cell injury caused by direct viral invasion as described in Lindner et al. [20] research, which identified the SARS-COV2 virus in the myocardium of COVID-19 patients after autopsy. ACE2 receptor-mediated myocardial injury and an increase in cardiometabolic demand due to systemic infection and hypoxia can also be suggested. Second, systemic inflammation and catecholamines release can cause plaque rupture in atherosclerotic coronaries and increase thrombosis liability in COVID-19 patients. Third, the cytokine storms with the surge of numerous interleukins (e.g., IL 2,6,8,10) and tumor necrosis factor (TNF) can cause myocardial injury. Fourth, the medications used in the Egyptian COVID-19 treatment protocol, such as corticosteroids, antivirals, and immune suppressive agents, can cause myocardial damage. [21,22,23,24].
HRV data analysis in the study population
In our study, autonomic dysfunction was prevalent as time domain indices SDNN was decreased in 24%, and rMSSD was > 40 ms in 42% of the population, while the frequency domain indices expressed in our study as LF/HF ratio was > 2 in 42% of the patients indicating sympathetic predominance.
In alignment with the data in the current study, Kurtoğlu et al. stated similar results. He conducted a case–control study of 50 patients after mild to moderate COVID-19 with no history of hospitalization, oxygen therapy, or severe respiratory or other significant organ involvement. They found that SDNN, SDANN, and SDNN index were significantly lower in the study group compared to the control group (p < 0.0001 for all). Also, rMSSD was depressed in the study group with a p-value = 0.001. Only the HF band in nu was depressed in the study group compared to the control group. Kurtoğlu et al. proposed three potential mechanisms for the sympathetic overdominance post-COVID. First, due to the effect of the constitutional symptoms of the acute COVID illness (e.g., fever, sleep disorders, sweating …. etc.). Second, brainstem or medullary mediated increase in sympathetic firing through the binding of the virus to ACE2 receptors found in the glial cells and the neurons. And finally, toxin or immune-mediated mechanism [25].
In opposition to our research, there was an increase in HRV explained by the parasympathetic predominance in COVID-19 patients enrolled in Kaliyaperumal et al. [26] study. However, patients included in the study were in active COVID-19 illness, unlike our research which mainly targeted the post-COVID population.
Correlation between GLS and HRV in the study group
Our research pointed out an association between impaired GLS and decreased SDNN. This could be explained as a mere co-existence of both phenomena in post-COVID patients or autonomic dysfunction-induced myocardial affection as proposed by Snelder et al. [27] in a sub-analysis of the CARDIOBESE study. They elaborated that the SDNN index and GLS were not only impaired in obese patients, but also, there was an evident difference in SDNN between obese patients with and without subclinical cardiac dysfunction, and thereby, SDNN was identified as an independent risk factor for cardiac dysfunction. Also the correlation between the GLS and SDNN could be explained by the myocardial injury caused by the cornovirus which may last even after recovery causing subtle LV affection which could be detected by speckle tracking, in addition to this inflammatory response and myocardial injury, the Covid 19 affection can induce sympathetic and parasympathetic imblances causing HRV dysfunction as measured by decreased SDNN.
Limitations
The small number of patients included and being a single hospital-based study precluded the generalization of the results to all COVID-19 patients. The absence of follow-up was a significant limitation of the current study. The study subjects were examined at a point of time “cross-sectional design”, and thus no data about LVGLS and HRV before the COVID-19 acute infection could be obtained. Increased age, DM, hypertension, and smoking may be confounding factors in our study that may have affected the GLS and HRV parameters' values.
Conclusion
In patients with prolonged symptoms after COVID-19 illness, GLS and HRV were assessed to try to explain the cardiac involvement. We found a high incidence of GLS impairment using STE and a significant prevalence of diminished HRV. HRV (especially SDNN) and GLS were significantly correlated, as 80% of the patients with impaired GLS had decreased SDNN (p-value < 0.01).
References
Alareedh M, Nafakhi H, Shaghee F, Nafakhi A (2020) Electrocardiographic markers of increased risk of sudden cardiac death in patients with COVID-19 pneumonia. Ann Non-invasive Electrocardiol 26(3):e12824. https://doi.org/10.1111/anec.12824
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O (2020) Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 5(7):831–840. https://doi.org/10.1001/jamacardio.2020.1286
Goldstein DS (2021) The possible association between COVID-19 and postural tachycardia syndrome. Heart Rhythm 18(4):508–509. https://doi.org/10.1016/j.hrthm.2020.12.007
Raj SR, Arnold AC, Barboi A, Claydon VE, Limberg JK, Lucci VM et al (2021) Long-COVID postural tachycardia syndrome: an American autonomic society statement. Clin Auton Res. https://doi.org/10.1007/s10286-021-00798-2
Fang SC, Wu YL, Tsai PS (2020) Heart rate variability and risk of all cause death and cardiovascular events in patients with cardiovascular disease: a meta-analysis of cohort studies. Biol Res Nurs 22(1):45–56. https://doi.org/10.1177/1099800419877442
Guo T, Fan Y, Chen M (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.1017
Akbarshakh A, Marban E (2020) COVID-19 and the heart. Circ Res 126(10):1443–1455
Huang L, Zhao P, Tang D et al (2020) Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2020.05.004
Liu J, Yang X, Zhu Y et al (2021) Diagnostic value of chest computed tomography imaging for COVID-19 based on reverse transcription-polymerase chain reaction: a meta-analysis. Infect Dis Poverty 10:126. https://doi.org/10.1186/s40249-021-00910-8
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available https://www.covid19treatmentguidelines.nih.gov/. Li X, Ma X.
Research to Practice (2018) Assessment of left ventricular global longitudinal strain for surveillance of cancer chemotherapeutic-related cardiac dysfunction. JACC Cardiovasc Imaging 11:1196–1201
Nunan D, Sandercock GR, Brodie DA (2010) A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin Electrophysiol 33(11):1407–1417
Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ (1987) Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 59:256–262. https://doi.org/10.1016/0002-9149(87)90795-8
Pavli A, Theodoridou M, Maltezou HC (2021) Post-COVID Syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res 52(6):575–581
Alhumayn A, Alsaif I, Enabi J, Bin NS (2022) A systematic review of the systematic review of post COVID-19 syndrome. J Med Law Public Health 2(1):64–69
Mahajan S, Kunal S, Shah B, Garg S, Palleda GM, Bansal A, Batra V, Yusuf J, Mukhopadhyay S, Kumar S, Tyagi S, Gupta A, Gupta MD (2021) Left ventricular global longitudinal strain in COVID-19 recovered patients. Echocardiography 38(10):1722–1730
Özer S, Candan L, Özyıldız AG, Turan OE (2021) Evaluation of left ventricular global functions with speckle tracking echocardiography in patients recovered from COVID-19. Int J Cardiovasc Imaging 37(7):2227–2233
Turan T, Özderya A, Şahin S et al (2021) Left ventricular global longitudinal strain in low cardiac risk outpatients who recently recovered from coronavirus disease 2019. Int J Cardiovasc Imaging 37:2979–2989
Caiado LDC, Azevedo NC, Azevedo RRC, Caiado BR (2022) Cardiac involvement in patients recovered from COVID-19 identified using left ventricular longitudinal strain. J Echocardiogr 20(1):51–56
Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, Scherschel K, Kirchhof P, Escher F, Schultheiss HP, Blankenberg S, Püschel K, Westermann D (2020) Association of cardiac infection with SARS-CoV-2 in CONFIRMED COVID-19 autopsy cases. JAMA Cardiol 5(11):1281–1285
- Basu-Ray I, Almaddah Nk, Adeboye A, et al. Cardiac Manifestations Of Coronavirus (COVID-19) [Updated 2022 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, Bucci E, Piacentini M, Ippolito G, Melino G (2020) COVID-19 infection: the perspectives on immune responses. Cell Death Differ 27(5):1451–1454
Xiong TY, Redwood S, Prendergast B, Chen M (2020) Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 41(19):1798–1800
Schoenhagen P, Tuzcu EM, Ellis SG (2002) Plaque vulnerability, plaque rupture, and acute coronary syndromes: (multi)-focal manifestation of a systemic disease process. Circulation 106(7):760–762
Kurtoğlu E, Afsin A, Aktaş İ, Aktürk E, Kutlusoy E, Çağaşar Ö (2022) Altered cardiac autonomic function after recovery from COVID-19. Ann Non-invasive Electrocardiol 27:e12916
Kaliyaperumal D, Rk K, Alagesan M, Ramalingam S (2021) Characterization of cardiac autonomic function in COVID-19 using heart rate variability: a hospital based preliminary observational study. J Basic Clin Physiol Pharmacol 32(3):247–253
Snelder SM, de Groot-de Laat LE, Biter LU, Castro Cabezas M, Pouw N, Birnie E, Boxma-de Klerk BM, Klaassen RA, Zijlstra F, van Dalen BM (2020) Subclinical cardiac dysfunction in obesity patients is linked to autonomic dysfunction: findings from the CARDIOBESE study. ESC Heart Fail 7(6):3726–3737
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research was carried out without funding.
Author information
Authors and Affiliations
Contributions
The authors listed below have contributed significantly to the submitted work : AN : Has took part in: conception and design of the study, performing the echocardiographic analysis , catheter intervention , interpretation of the data, drafting of the manuscript and final approval of the manuscript submitted MB: Has took part in: conception and design of the study, echocardiographic analysis of the data, performing catheter intervention , interpretation of the data submitted for the patients included in the study group, revision and acceptance of the manuscript. ZA: Has took part in: conception and design of the study, echocardiographic analysis of the data, performing catheter intervention , interpretation of the data submitted for the patients included in the study group, revision and acceptance of the manuscript. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nour, A., Fouad, M. & Salam, Z.A. Evaluation of cardiovascular autonomic dysfunction in symptomatic post-COVID-19 patients using the heart rate variability (HRV) and detection of subtle LV dysfunction using 2D global longitudinal strain (GLS). Int J Cardiovasc Imaging 39, 2107–2118 (2023). https://doi.org/10.1007/s10554-023-02915-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02915-w