Abstract
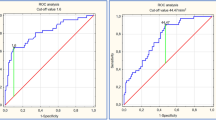
In patients with nonvalvular atrial fibrillation (NVAF), the impact of left ventricular diastolic function on the risk of left atrial appendage (LAA) thrombus has rarely been studied. This prospective study aimed to investigate the relationship between diastolic function and the risk of LAA thrombus in patients with NVAF. Seventy-six patients with NVAF admitted to receive radiofrequency catheter ablation were prospectively enrolled. All the patients underwent transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) in 24 h before ablation. Diastolic function was estimated by TTE including left atrial volume index (LAVI) and E/e', as well as invasive left atrial pressure (LAP) measured during the ablation procedure. LAA peak emptying velocity (LAA-PEV) and the intensity of spontaneous echo contrast (SEC) were determined by TEE. Average E/e', LAVI and mean LAP had a significant positive correlation with the intensity of SEC, the coefficient of correlation were 0.344 (p = 0.002), 0.416 (p < 0.001) and 0.402 (p < 0.001), respectively. After adjustment for CHA2DS2-VASc score and type of AF, multivariate regression analysis revealed that increased LAP (OR 1.144, 95% CI 1.012–1.293, p = 0.031) independently correlated with the risk of LAA thrombus (SEC ≥ Grade 2). LAA-PEV showed a significantly inverse relationship with mean LAP in patients with AF (r = − 0.525, p < 0.001), and in the assessment of elevated LAP with TEE, the LAA-PEV cut-off of 0.40 m/s had a sensitivity of 80%, specificity of 81%. Left ventricular diastolic dysfunction may constitute a potential risk for LAA thrombus and stroke. Furthermore, evaluation of LAA emptying with use of TEE is helpful for assessing the LAP status of patients with AF.




Similar content being viewed by others
Data availability
Data are available upon reasonable request by contacting the corresponding author.
References
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C et al (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42(5):373–498
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JJ et al (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a Report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation 140(2):e125–e151
Yoo J, Song D, Baek JH, Kim YD, Nam HS, Hong GR et al (2016) Poor outcome of stroke patients with atrial fibrillation in the presence of coexisting spontaneous echo contrast. Stroke 47(7):1920–1922
Bernhardt P, Schmidt H, Hammerstingl C, Luderitz B, Omran H (2005) Patients with atrial fibrillation and dense spontaneous echo contrast at high risk a prospective and serial follow-up over 12 months with transesophageal echocardiography and cerebral magnetic resonance imaging. J Am Coll Cardiol 45(11):1807–1812
Backhaus JF, Pflaumbaum A, Krogias C, Kreimer F, Mugge A, Gold R et al (2021) Short- and long-term outcome of patients with spontaneous echo contrast or thrombus in the left atrial appendage in the era of the direct acting anticoagulants. Clin Res Cardiol 110(11):1811–1821
Garshick MS, Mulliken J, Schoenfeld M, Riedy K, Guo Y, Zhong J et al (2018) Average e’ velocity on transthoracic echocardiogram is a novel predictor of left atrial appendage sludge or thrombus in patients with atrial fibrillation. Echocardiography 35(12):1939–1946
Doukky R, Garcia-Sayan E, Patel M, Pant R, Wassouf M, Shah S et al (2016) Impact of diastolic function parameters on the risk for left atrial appendage thrombus in patients with nonvalvular atrial fibrillation: a prospective study. J Am Soc Echocardiogr 29(6):545–553
Demircelik MB, Cetin M, Cicekcioglu H, Ucar O, Duran M (2014) Effect of left ventricular diastolic dysfunction on left atrial appendage function and thrombotic potential in nonvalvular atrial fibrillation. Anadolu Kardiyol Derg 14(3):256–260
Doukky R, Garcia-Sayan E, Gage H, Nagarajan V, Demopoulos A, Cena M et al (2014) The value of diastolic function parameters in the prediction of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Cardiovasc Ultrasound 12:10
Iwakura K, Okamura A, Koyama Y, Date M, Higuchi Y, Inoue K et al (2011) Effect of elevated left ventricular diastolic filling pressure on the frequency of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Am J Cardiol 107(3):417–422
Ayirala S, Kumar S, O’Sullivan DM, Silverman DI (2011) Echocardiographic predictors of left atrial appendage thrombus formation. J Am Soc Echocardiogr 24(5):499–505
Nagueh SF, Smiseth OA, Appleton CP, Byrd BR, Dokainish H, Edvardsen T et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr 29(4):277–314
Fatkin D, Herbert E, Feneley MP (1994) Hematologic correlates of spontaneous echo contrast in patients with atrial fibrillation and implications for thromboembolic risk. Am J Cardiol 73(9):672–676
Bergau L, Vollmann D, Luthje L, Sohns JM, Seegers J, Sohns C et al (2014) Measurement of left atrial pressure is a good predictor of freedom from atrial fibrillation. Indian Pacing Electrophysiol J 14(4):181–193
Linhart M, Lewalter T, Mittmann-Braun EL, Karbach NC, Andrie RP, Hammerstingl C et al (2013) Left atrial pressure as predictor for recurrence of atrial fibrillation after pulmonary vein isolation. J Interv Card Electrophysiol 38(2):107–114
Li YH, Tsai LM, Tsai WC, Chao TH, Lin LJ, Chen JH (1999) Decreased left atrial appendage function is an important predictor of elevated left ventricular filling pressure in patients with congestive heart failure. Int J Cardiol 68(1):39–45
Tabata T, Oki T, Fukuda N, Iuchi A, Manabe K, Kageji Y et al (1996) Influence of left atrial pressure on left atrial appendage flow velocity patterns in patients in sinus rhythm. J Am Soc Echocardiogr 9(6):857–864
Hwang SH, Roh SY, Shim J, Choi JI, Kim YH, Oh YW (2017) Atrial fibrillation: relationship between left atrial pressure and left atrial appendage emptying determined with velocity-encoded cardiac MR imaging. Radiology 284(2):381–389
Acknowledgements
There are no financial or other relationships that might lead to a conflict of interest of the present article. All authors have reviewed the final version of the manuscript and approve it for publication. We certify that this manuscript has not been published in whole or in part nor is it being considered for publication elsewhere.
Funding
This research did not receive any specific grant from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Gaigai Ma wrote the main manuscript text and participated the whole study, Ligang Fang and Xue Lin prepared data for echocardiography, Peng Gao provided invasive left atrial pressure measurements and Quan Fang was responsible for the design of the entire study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Peking Union Medical College Hospital NO. S-K1994.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, G., Fang, L., Lin, X. et al. Relationship between left ventricular diastolic function and the risk of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Int J Cardiovasc Imaging 39, 35–42 (2023). https://doi.org/10.1007/s10554-022-02690-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02690-0