Abstract
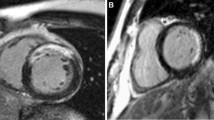
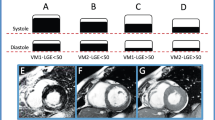
Late gadolinium enhancement (LGE) is widely used to precisely localize and determine the extent and transmurality of myocardial scarring. Performing LGE imaging at end-systole may reduce motion artefacts. It is therefore important to know whether end-systolic imaging influences infarct transmurality in patients with ischemic scar. 107 dysfunctional segments were studied in 20 consecutive patients with established coronary artery disease. Patient specific trigger delays were used to obtain end-diastolic and end-systolic LGE images (LGEed, LGEes). Wall thickness (WTed, WTes), thickness of the remaining viable rim (RIMed, RIMes) and end-diastolic scar thickness were measured manually. There was LGE in 84% of all dysfunctional segments with a mean scar of 3.4 ± 2.5 mm. Total wall thickness and the thickness of the remaining viable rim increased from diastole to systole (WTed 7.8 ± 1.9 vs. WTes 8.4 ± 2.2; P < 0.001; RIMed 4.4 ± 3.1 vs. RIMes 5 ± 3.4; P < 0.001). Transmurality of scar decreased from end-diastole to end-systole (LGEed 46 ± 33% vs. LGEes 44 ± 33%; P < 0.001). This was most pronounced in a subgroup of segments (n = 15) with visual scar transmurality between 50 and 75% (LGEed 75 ± 15% vs. LGEes 70 ± 16%; P < 0.001). The change in transmurality was inversely correlated with the change of the thickness of the remaining viable rim between diastole and systole (r = −0.7; P < 0.001). Scar transmurality was reduced by up to 12% in the individual patient. Scar transmurality changes due to thickening of the remaining viable rim. Whereas these differences might not impact on clinical decision-making in most patients, there will be an occasional misclassification if cut-off values are used (e.g. scar <50 or >50%) or if exact data is required for research studies.







Similar content being viewed by others
References
Morton G, Schuster A, Perera D, Nagel E (2010) Cardiac magnetic resonance imaging to guide complex revascularization in stable coronary artery disease. Eur Heart J 31(18):2209–2215
Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM (2000) The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 343(20):1445–1453
Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S et al (2010) Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 31(20):2501–2555
Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E (2008) Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: board of trustees task force on standardized protocols. J Cardiovasc Magn Reson 10:35
Matsumoto H, Matsuda T, Miyamoto K, Shimada T, Hayashi A, Mikuri M, Hiraoka Y (2010) Late gadolinium-enhanced cardiovascular MRI at end-systole: feasibility study. Am J Roentgenol 195(5):1088–1094
Thiele H, Schuster A, Erbs S, Linke A, Lenk K, Adams V, Hambrecht R, Schuler G (2009) Cardiac magnetic resonance imaging at 3 and 15 months after application of circulating progenitor cells in recanalised chronic total occlusions. Int J Cardiol 135(3):287–295
Kato S, Kitagawa K, Ishida N, Ishida M, Nagata M, Ichikawa Y, Katahira K, Matsumoto Y, Seo K, Ochiai R (2010) Assessment of coronary artery disease using magnetic resonance coronary angiography a national multicenter trial. J Am Coll Cardiol 56(12):983–991
Chiribiri A, Kelle S, Götze S, Kriatselis C, Thouet T, Tangcharoen T, Paetsch I, Schnackenburg B, Fleck E, Nagel E (2008) Visualization of the cardiac venous system using cardiac magnetic resonance. Am J Cardiol 101(3):407–412
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Thiele H, Kappl MJE, Conradi S, Niebauer J, Hambrecht R, Schuler G (2006) Reproducibility of chronic and acute infarct size measurement by delayed enhancement-magnetic resonance imaging. J Am Coll Cardiol 47(8):1641–1645
Ichikawa Y, Sakuma H, Suzawa N, Kitagawa K, Makino K, Hirano T, Takeda K (2005) Late gadolinium-enhanced magnetic resonance imaging in acute and chronic myocardial infarction. Improved prediction of regional myocardial contraction in the chronic state by measuring thickness of nonenhanced myocardium. J Am Coll Cardiol 45(6):901–909
Kirschbaum SW, Rossi A, van Domburg RT, Gruszczynska K, Krestin GP, Serruys PW, Duncker DJ, de Feyter PJ, van Geuns R-JM (2010) Contractile reserve in segments with nontransmural infarction in chronic dysfunctional myocardium using low-dose dobutamine CMR. J Am Coll Cardiol Img 3(6):614–622
Wellnhofer E, Olariu A, Klein C, Gräfe M, Wahl A, Fleck E, Nagel E (2004) Magnetic resonance low-dose dobutamine test is superior to SCAR quantification for the prediction of functional recovery. Circulation 109(18):2172–2174
Allman KC, Shaw LJ, Hachamovitch R, Udelson JE (2002) Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol 39(7):1151–1158
Nagel E, Schuster A (2010) Shortening without contraction: new insights into hibernating myocardium. J Am Coll Cardiol Img 3(7):731–733
Peel S, Jansen C, Toussaint N, Schaeffter T, Botnar RM (2010) Non-selective double inversion recovery pre-pulse for flow-independent black blood myocardial viability imaging. J Cardiovasc Magn Reson 12(Suppl 1):104
Acknowledgments
Andreas Schuster receives grant support from the British Heart Foundation (BHF) (RE/08/003 and FS/10/029/28253) and the Biomedical Research Centre (BRC-CTF 196).
Conflict of interest
Eike Nagel received minor consultancy fees from Philips Healthcare and major grant support from Philips Healthcare and Bayer Schering Pharma. The other authors declare that they have no competing interests’.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schuster, A., Chiribiri, A., Ishida, M. et al. End-systolic versus end-diastolic late gadolinium enhanced imaging for the assessment of scar transmurality. Int J Cardiovasc Imaging 28, 773–781 (2012). https://doi.org/10.1007/s10554-011-9877-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-011-9877-3