Abstract
Purpose
Postpartum breast cancer (PPBC) is a not well-established subset of breast cancer, and only few studies address its poorer prognosis. However, previous studies show that PPBC is associated with worse outcome with higher rates of metastasis than in young women’s breast cancer (YWBC). We aimed to analyze the clinical characteristics and prognosis of PPBC based on the diagnosis period of PPBC.
Methods
We retrospectively reviewed 208,780 patients with breast cancer from the Korean Breast Cancer Society registry (KBCSR) database between January 2000 and December 2014. We included premenopausal women aged 20–50 years who underwent breast cancer surgery. The patients were classified by 5-year intervals according to the diagnosis period of breast cancer, from the first birth to the breast cancer diagnosis.
Results
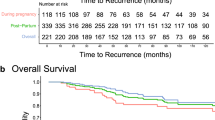
Compared with patients in the other groups, patients diagnosed within postpartum 5 years (PPBC < 5 years) group were younger, had a more advanced stage, had lower estrogen receptor (ER) and progesterone receptor (PR) expression, and had a higher human epidermal growth factor receptor 2 (HER2) positive rate. Further, PPBC < 5 years group had a worse survival rate than the nulliparous and other groups (5-year cumulative survival: PPBC < 5 years group, 89%; nulliparous group, 97.3%; 5 ≤ PPBC < 10 years group, 93%). In the multivariate analysis, the PPBC < 5 years group was associated with a worse survival rate (hazard ratio 1.55, 95% confidence interval [CI] 1.148–2.094, p 0.004) after adjustment for age at diagnosis, breast cancer stage, ER and HER2 status, Ki-67 level, and chemotherapy.
Conclusion
Our findings indicated that patients diagnosed with breast cancer within the first 5 years after delivery had aggressive characteristics and a poor survival rate. It is important to elucidate the pathophysiology of PPBC and establish novel therapeutic strategies to improve the survival rate.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the KBCS registry, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, data are available from the authors upon reasonable request and with the permission of the KBCS registry.
Change history
14 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10549-023-07189-3
References
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Anderson WF et al (2006) Comparison of age distribution patterns for different histopathologic types of breast carcinoma. Cancer Epidemiol Biomark Prev 15(10):1899–1905
Thomas A et al (2019) Incidence and survival among young women with stage I-III breast cancer: SEER 2000–2015. JNCI Cancer Spectr 3(3):pkz040
Bharat A et al (2009) Patient and tumor characteristics associated with increased mortality in young women (< or =40 years) with breast cancer. J Surg Oncol 100(3):248–251
Callihan EB et al (2013) Postpartum diagnosis demonstrates a high risk for metastasis and merits an expanded definition of pregnancy-associated breast cancer. Breast Cancer Res Treat 138(2):549–559
Stensheim H et al (2009) Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol 27(1):45–51
Lyons TR, Schedin PJ, Borges VF (2009) Pregnancy and breast cancer: when they collide. J Mammary Gland Biol Neoplasia 14(2):87–98
Amant F et al (2013) Prognosis of women with primary breast cancer diagnosed during pregnancy: results from an international collaborative study. J Clin Oncol 31(20):2532–2539
Schedin P (2006) Pregnancy-associated breast cancer and metastasis. Nat Rev Cancer 6(4):281–291
Liu Q et al (2002) Transient increase in breast cancer risk after giving birth: postpartum period with the highest risk (Sweden). Cancer Causes Control 13(4):299–305
Van den Rul N et al (2011) Postpartum breast cancer behaves differently. Facts Views Vis Obgyn 3(3):183–188
Goddard ET et al (2019) Association between postpartum breast cancer diagnosis and metastasis and the clinical features underlying risk. JAMA Netw Open 2(1):e186997
Bae SY et al (2018) Neoadjuvant chemotherapy and prognosis of pregnancy-associated breast cancer: a time-trends study of the korean breast cancer registry database. J Breast Cancer 21(4):425–432
Kroman N et al (1997) Time since childbirth and prognosis in primary breast cancer: population based study. BMJ 315(7112):851–855
Albrektsen G et al (2005) Breast cancer risk by age at birth, time since birth and time intervals between births: exploring interaction effects. Br J Cancer 92(1):167–175
Barnett GC et al (2008) Risk factors for the incidence of breast cancer: do they affect survival from the disease? J Clin Oncol 26(20):3310–3316
Butt S et al (2009) Parity and age at first childbirth in relation to the risk of different breast cancer subgroups. Int J Cancer 125(8):1926–1934
Nixon AJ et al (1994) Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. J Clin Oncol 12(5):888–894
Anders CK et al (2009) Breast cancer before age 40 years. Semin Oncol 36(3):237–249
Desreux JAC (2018) Breast cancer screening in young women. Eur J Obstet Gynecol Reprod Biol 230:208–211
Jørgensen KJ, Zahl PH, Gøtzsche PC (2010) Breast cancer mortality in organised mammography screening in Denmark: comparative study. BMJ 340:c1241
Bae SY et al (2018) Clinical characteristics and prognosis of pregnancy-associated breast cancer: poor survival of Luminal B subtype. Oncology 95(3):163–169
Shoemaker ML et al (2018) Differences in breast cancer incidence among young women aged 20–49 years by stage and tumor characteristics, age, race, and ethnicity, 2004–2013. Breast Cancer Res Treat 169(3):595–606
Jindal S et al (2021) Postpartum breast cancer has a distinct molecular profile that predicts poor outcomes. Nat Commun 12(1):6341
Strange R et al (1992) Apoptotic cell death and tissue remodelling during mouse mammary gland involution. Development 115(1):49–58
Schedin PJ et al (1996) Programmed cell death and mammary neoplasia. Cancer Treat Res 83:3–22
Mantovani A et al (2007) Inflammation and cancer: breast cancer as a prototype. Breast 16(Suppl 2):S27-33
Goddard ET et al (2016) Quantitative extracellular matrix proteomics to study mammary and liver tissue microenvironments. Int J Biochem Cell Biol 81(Pt A):223–232
Lyons TR et al (2014) Cyclooxygenase-2-dependent lymphangiogenesis promotes nodal metastasis of postpartum breast cancer. J Clin Invest 124(9):3901–3912
Bingle L, Brown NJ, Lewis CE (2002) The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol 196(3):254–265
Acknowledgements
This article was supported by the Korean Breast Cancer Society (KBCS). We thank all members of the KBCS who participated in the KBCS online registry.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation was performed by JEC, SWL, YJL, Y-JK, HJL. Data collection and analysis were performed by PSP and SYB. The first draft of the manuscript was written by PSP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In the original publication of the article, the affiliation of corresponding author Soo Youn Bae and coauthor Young Joo Lee were published incorrectly as “Department of Surgery, incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea”. The correct affiliation of Soo Youn Bae and Young Joo Lee is Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paik, P.S., Choi, J.E., Lee, S.W. et al. Clinical characteristics and prognosis of postpartum breast cancer. Breast Cancer Res Treat 202, 275–286 (2023). https://doi.org/10.1007/s10549-023-07069-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07069-w