Abstract
Purpose
Breast cancer and its treatments may increase the risk of type 2 diabetes (T2D). We conducted a systematic review and meta-analysis to investigate the association between breast cancer and the incidence of T2D overall, and according to breast cancer treatments.
Methods
We searched PubMed, Embase and references of relevant papers for studies on breast cancer, breast cancer treatment, and subsequent T2D risk. Using random-effects models, we calculated effect estimates and associated 95% confidence intervals of the association between breast cancer, adjuvant breast cancer treatments (i.e., endocrine therapy (tamoxifen, aromatase inhibitors, and combined) and chemotherapy), and subsequent T2D. We used funnel plots to assess publication bias.
Results
Among 15 eligible studies, 10 reported on T2D risk after breast cancer, chemotherapy, or endocrine therapy; five studies investigated more than one association. Compared with patients without breast cancer, those with breast cancer and those who received any endocrine therapy had elevated risk of incident T2D (EE = 1.23, 95% CI = 1.13–1.33 and EE = 1.23, 95% CI = 1.16–1.32, respectively). Among breast cancer patients only, the risk of T2D was higher for those who received tamoxifen compared with those who did not receive tamoxifen (EE = 1.28, 95% CI = 1.18–1.38). Due to few studies, analyses investigating T2D risk after treatment with aromatase inhibitors or chemotherapy were inconclusive.
Conclusion
Our findings suggest an elevated risk of T2D in breast cancer survivors, particularly after tamoxifen therapy. Further research is needed to determine the impact of aromatase inhibitors, and chemotherapy on the incidence of T2D after breast cancer.
Similar content being viewed by others
Introduction
Breast cancer is the most frequently diagnosed malignancy in women. In 2023, ~ 2.3 million incident breast cancers will be diagnosed worldwide. Due to improvements in breast cancer diagnostics and treatment, the population of breast cancer survivors has increased. In 2020, there were about 7.8 million 5-year survivors of breast cancer globally [1]. This number is expected to continue to increase [2], highlighting the need for better understanding of the late effects of the disease and its treatments. One such late effect may be type 2 diabetes (T2D).
Observational studies point towards increased risk of T2D in breast cancer survivors [3,4,5,6,7]. Breast cancer and T2D share risk factors including obesity, inflammation, and altered endogenous hormones [8]. Still, T2D may also occur as a complication of breast cancer therapy [3, 4, 9, 10]. For example, glucocorticoid therapy given concomitantly with chemotherapy may increase T2D risk due to weight gain, reduced insulin synthesis, reduced insulin sensitivity, and hyperglycemia [3, 10]. Endocrine therapy modifies insulin sensitivity and may invoke a persistent excess risk of T2D [9]. Low estrogen levels in postmenopausal women are associated with increased risk of T2D [11, 12]. Yet, aromatase inhibitors—the endocrine therapy recommended for postmenopausal women—inhibit estrogen synthesis [13]. Evidence also suggests that tamoxifen impairs glucose homeostasis by promoting apoptosis of pancreatic β-cells [14]. Tamoxifen is also associated with reduced insulin sensitivity in premenopausal women with overweight [15]. If breast cancer is associated with elevated risk of developing T2D, it may be beneficial to screen breast cancer survivors for T2D to expedite diagnosis and improve prognosis. It may also prompt the initiation of preventive measures in subgroups of breast cancer survivors deemed at high risk of developing T2D.
A meta-analysis by Ye et al. aimed to investigate the incidence of T2D after breast cancer and endocrine therapy, suggesting elevated risk of T2D in breast cancer survivors [16]. Still, their study did not include all eligible studies. As such, the evidence to date on the impact of breast cancer and subsequent risk of T2D requires clarification.
We therefore conducted a systematic review and meta-analysis to collate evidence on the association between breast cancer and subsequent risk of T2D. We also evaluated this association according to the receipt of breast cancer treatments.
Methods
Search strategy and eligibility criteria
We conducted this study in accordance with The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [17] and the Conducting Systematic Reviews and Meta-Analyses of Observational Studies of Etiology (COSMOS-E) guidelines [18].
We performed a search for all eligible studies in MEDLINE (PubMed) and EMBASE from inception through May 2022. See Online Resource 1 for search terms. We also searched the reference lists of eligible articles.
We included all observational studies where (i) breast cancer or breast cancer treatment [chemotherapy or endocrine treatment (tamoxifen or aromatase inhibitors)] among breast cancer patients was included as an exposure and (ii) the outcome was incident T2D. We restricted to published papers written in English, Danish, Norwegian or Swedish.
Study selection and data extraction
Two investigators (medical student N.J. and PhD-student K.K.) independently screened all articles by title and abstract to remove irrelevant studies. The results from all searches were inserted into Covidence (Teamsquare, Melbourne, Australia) and duplicates were removed. The same two investigators performed independent unblinded eligibility assessment of the retrieved publications and evaluated their eligibility for inclusion based on the afore-mentioned eligibility criteria.
The two investigators used a predefined data extraction form to extract the following data from the eligible studies: author, title, journal, publication year, study design, study period, study size, length of follow-up, inclusion criteria, exclusion criteria, data source, methods, age and sex distribution, exposure (treatment), comparator group, outcome(s), risk estimate used, main results, and potential confounders adjusted for. When effect estimates (EEs) were not available, the investigators extracted the raw data. We also retrieved 95% confidence intervals (CI) as measures of precision.
Diabetes mellitus outcome definition
Diabetes mellitus in the studies was ascertained via diagnostic codes, prescriptions for antidiabetic medication, and/or blood glucose testing. For studies that did not specify which type of diabetes mellitus was examined, we assumed it was T2D if the women were diagnosed with diabetes mellitus as adults (at age 18 years or older).
Study quality and risk of bias assessment
Since there is no consensus regarding how to assess study quality and risk of bias, we followed the COSMOS-E guidelines [18]. Consequently, we evaluated the studies qualitatively by considering how thoroughly the authors reported methods and results as well as considering the potential for selection and information bias, and confounding within the studies.
Statistical analyses
EEs for each outcome were pooled using a random-effects model with the Restricted Maximum Likelihood (REML) method and illustrated using forest plots. Statistical heterogeneity was assessed using I2 statistics.
Measures of relative risk [risk ratios (RR), odds ratios (OR), and hazard ratios (HR)] were considered equivalent. As the outcome is rare, and the studies investigated the same exposure and outcome, we considered it reasonable to compare the ratios [19]. In studies where no relative risk estimate was provided, RR and 95% CIs were calculated from raw data.
The estimates for breast cancer and risk of developing T2D were pooled in one analysis, while the effects of endocrine therapy overall, tamoxifen and aromatase inhibitors were examined in separate analyses. For each of these treatments, breast cancer patients were compared to breast cancer patients who did not use the treatment and/or non-cancer referents, depending on the data available from the articles.
Last, we used funnel plots to visually assess publication bias across studies.
Statistical analyses were performed using R Statistical Software [version 4.1.3 (2022-03-10); The R Foundation for Statistical Computing].
Results
Systematic literature search
Our systematic search in PubMed and EMBASE yielded 2699 studies, of which 756 were duplicates and 1900 were excluded based on title or abstract alone. The full text of the remaining 43 studies was examined. Of these, 28 studies did not meet the eligibility criteria and were thus discarded (Fig. 1). When searching reference lists, we found no additional studies. Our systematic review therefore included a total of 15 studies [3,4,5,6,7, 9, 20,21,22,23,24,25,26,27,28].
Study characteristics and risk of bias
Among the 15 eligible studies, 10 reported on T2D risk after either breast cancer, chemotherapy, or endocrine therapy [4, 6, 9, 21,22,23, 25,26,27,28]; five studies investigated more than one association [3, 5, 7, 20, 24]. The total number of breast cancer patients followed in cohort studies was 93,974; the size of the individual studies ranged from 114 to 24,976 patients [3,4,5, 7, 20,21,22,23,24,25,26,27,28]. The only case-control study included 1,445 breast cancer patients with T2D [6], while the only case-cohort study included 324 breast cancer patients with T2D [9]. Of the 15 studies, five were restricted to postmenopausal women—two studies based this on a study population of breast cancer patients aged over 55 years [3, 5], two restricted to breast cancer patients aged over 65 years [6, 28], and one restricted to breast cancer patients aged over 66 years [20]. Only four of the studies included information on weight in the adjusted analyses, either adjusting for overweight or body mass index, the latter as a continuous variable [4, 20, 23, 24]. For study characteristics, please see Table 1.
Breast cancer and subsequent risk of T2D
Study characteristics and risk of bias
Eight studies investigated the association between breast cancer and subsequent risk of T2D; all eight were cohort studies [3,4,5, 7, 20, 22,23,24]. Follow-up time ranged from three months [22] to a maximum of 15 years [5]. The study with three months follow-up included 114 patients and was excluded from the meta-analysis since it lacked a referent group. For the studies deemed eligible for inclusion in the meta-analysis, follow-up was therefore between two and 15 years. Referent groups in all studies were women without any previous cancer or T2D diagnosis, except for the study by Juanjuan where controls could potentially have another type of cancer [23]. Therefore, the study by Juanjuan was excluded from the meta-analytic models.
In all, 80,683 breast cancer patients were followed in the six studies included in the meta-analysis (Fig. 2). One study followed all types of cancer, but provided sparse information on their breast cancer cohort [4]. The remaining five studies acquired information on both cases and non-cancer controls from large registries with information on T2D diagnosis based on international classification of disease (ICD) diagnostic codes and/or from prescription claims for diabetes medications [3, 5, 7, 20, 24].
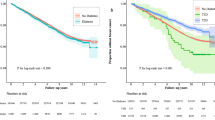
Meta-analyses
The overall pooled EE for T2D among patients with breast cancer compared to non-cancer controls was 1.23 (95% CI: 1.13–1.33). There was evidence of statistical heterogeneity, as indicated by an overall I2 statistic of 97%. Nevertheless, because the studies consistently pointed in the same direction, we pooled the results using the REML. The small number of studies in the analysis weakened the validity of the funnel plot, but we did observe some evidence of publication bias (Fig. 3).
Endocrine therapy and subsequent risk of T2D
Study characteristics and risk of bias
Nine studies reported on the association between endocrine therapy and subsequent T2D among breast cancer patients [5,6,7, 9, 21, 24,25,26, 28]. Of these, three reported on endocrine therapy in general without specifying tamoxifen or aromatase inhibitors [5, 24, 26], two reported on tamoxifen only [7, 21], two reported on tamoxifen and aromatase inhibitors separately [6, 28], and two reported on all three categories separately [9, 25]. Seven of these studies were cohort studies [5, 7, 21, 24,25,26, 28], one was a nested case-cohort study [9], and one was a case-control study [6].
Mean follow-up time in all but one study by Santorelli et al. [28], ranged from five to seven years. The study by Santorelli et al. had a maximum follow-up of two years which may not be a sufficient period of time for development of T2D attributable to endocrine therapy.
Except for one study, which included propensity score-matched controls [21], the studies standardized for age and baseline comorbidities, either by matching or adjusting. One study adjusted for smoking status [24].
Meta-analysis
Our findings on the incidence of T2D associated with the receipt of the various endocrine therapies are summarized in Figs. 4 and 5. One sub-analysis included four studies, two sub-analyses included three studies, and three sub-analyses included two studies. The low number of included studies impacts the precision of the pooled estimates. However, most of the included studies reported an increased risk of developing T2D, regardless of treatment and the type of comparison cohort (breast cancer patients who did not receive endocrine therapy, or non-cancer comparators). Breast cancer patients who received any endocrine therapy had an EE of 1.23 (95% CI = 1.16–1.32) compared with controls without cancer. In a sub-analysis of tamoxifen-treated breast cancer patients compared with breast cancer patients who had not received tamoxifen, pooling of the four included studies yielded an EE of 1.28 (95% CI: 1.18–1.38) with an I2 statistic of 0%.
Breast cancer-directed chemotherapy and subsequent risk of T2D
Study characteristics and risk of bias
Four studies evaluated the association between chemotherapy and subsequent risk of T2D: all were cohort studies [3, 20, 24, 27]. Two included a comparison cohort of non-cancer controls [3, 24], one compared breast cancer patients treated with versus without chemotherapy [20]. One study did not include a reference group and instead investigated T2D incidence among the breast cancer patients examined at their clinic [27]. Still, none of the studies adjusted for concomitant glucocorticoid use which is prescribed with chemotherapy to counteract side effects, and can be associated with hyperglycemia [29]. Additionally, none of the studies adjusted for endocrine therapy. Because of the heterogeneity of the studies, we did not pool the results.
Results
Overall, the three studies with a comparison cohort showed an increased risk of T2D after chemotherapy, regardless of whether the controls were breast cancer patients or non-cancer referents. The study by Accordino et al. showed an adjusted OR of 1.19 (95% CI: 1.08–1.31) after at least two years follow-up [20]; in Lipscombe et al., the adjusted HR was 1.24 (95% CI: 1.12–1.38) after two years follow-up, which attenuated over 10-years of follow-up [3]. Kwan et al. had an adjusted HR of 1.23 (95% CI: 1.11–1.38) with a mean follow-up of seven years [24].
Discussion
Our findings suggest that breast cancer survivors have increased risk of developing T2D compared with women without cancer. The elevated risk of T2D was particularly evident in the first few years after chemotherapy, dissipating in some studies with longer follow-up. Breast cancer patients who received tamoxifen therapy had higher risk of developing T2D compared with those who did not receive tamoxifen and compared with non-cancer referents.
Our study builds on the previous evidence presented in the meta-analysis by Ye et al. [16]. Yet, they restricted their meta-analysis to studies that examined the association between endocrine therapy and T2D and did not report associations for other breast cancer therapies. Furthermore, Ye and colleagues pooled data from one study on tamoxifen with data from studies investigating endocrine therapy in general, omitting other potentially eligible studies from their analysis [6, 28].
Our observed elevated risk of T2D associated with chemotherapy may be partly attributable to the afore-mentioned glucocorticoid-associated transient hyperglycemia [30]. We note that the studies investigating chemotherapy showed consistently increased risk of T2D, but the risk attenuated after treatment completion in at least one study [3]. This could be due to discontinuation of the chemotherapy-associated concomitant steroid use. However, none of the included studies incorporated information on glucocorticoid use, precluding the distinction of steroid-induced T2D from the effect of chemotherapy and chemotherapy-associated weight-gain per se [31]. Nonetheless, almost all breast cancer patients receive concomitant glucocorticoids during chemotherapy, so it is challenging to distinguish the effects of chemotherapy and glucocorticoids separately. Additionally, the results are potentially confounded by the receipt of endocrine therapy since none of the studies adjusted for this.
The increased risk of T2D in breast cancer survivors who received tamoxifen may be attributable to several factors. Tamoxifen has been associated with lower insulin sensitivity in premenopausal women with overweight, rendering them susceptible to developing T2D [15]. Mouse models suggest that tamoxifen exacerbates insulin deficiency by reversing estradiol-mediated protection of β-cells [14]. Accordingly, tamoxifen may increase the risk of T2D by reducing insulin sensitivity, and could also worsen the clinical course of T2D by promoting apoptosis in pancreatic β-cells. This may have clinical implications when selecting appropriate endocrine therapy for breast cancer patients with pre-existing T2D. Unfortunately, due to few studies, it was not possible to evaluate if the risk of T2D was higher after use of aromatase inhibitors as distinct from endocrine therapy in general.
Several issues warrant consideration when interpreting our findings. Most studies had small sample size, which impacted the sub-analyses investigating specific treatments. This is reflected in the wide confidence intervals in the forest plots illustrating the association of tamoxifen and aromatase inhibitor use with the risk of T2D. Another issue is the use of databases to obtain information on diabetes mellitus. Preclinical diabetes can remain undiagnosed for years; thus, the likelihood of testing and diagnosing T2D in a population of cancer survivors may be higher compared with their non-cancer counterparts. This would yield differential misclassification since breast cancer survivors may have more frequent health care contact and therefore be more likely to go to a hospital or primary care physician given their pre-existing condition. This may have inflated our observed risk of developing T2D in cancer survivors compared with their non-cancer counterparts. Another limitation is the lack of information on diabetes type which we assumed to be type 2 if not stated otherwise. We therefore set the age limit to 18 years, but some individuals aged above 18 years might still have been diagnosed with type 1 diabetes. Still, we expect this to be few women and to have negligible impact on our findings.
None of the included studies differentiated between breast cancer in pre- and postmenopausal women. This is important given the distinct disease courses and endocrine therapies recommended for pre- and postmenopausal women with breast cancer. Use of aromatase inhibitors became standard treatment for postmenopausal women in 2004 [32]. Yet, none of the studies overlapping this time period accounted for the updated clinical guidelines. Furthermore, no studies were restricted to premenopausal breast cancer patients. If the increased risk of T2D after breast cancer is a result of the anti-estrogen mechanisms of endocrine therapy, risk may be differential in premenopausal versus postmenopausal women due to the inherently higher estrogen-levels in premenopausal women. Such women receive tamoxifen therapy as guideline treatment for estrogen receptor-positive tumors and have the longest time at risk for subsequent development of T2D.
Although some of the studies adjusted for patient weight at baseline, no studies incorporated information on weight changes during follow-up. Breast cancer treatment leads to weight gain, which in turn, can also increase the risk of T2D [33]. Because of this, we cannot dismiss the possibility that our findings may be partly attributable to weight gain rather than a direct effect of breast cancer or its treatment on the risk of T2D.
Overall, our findings highlight the limited data on the association between breast cancer and subsequent risk of T2D. The statistical power varied across the studies and our meta-analyses. Moreover, we observed considerable heterogeneity across all our meta-analyses, precluding definitive conclusions.
Still, our findings provide insights into the potential impact of breast cancer and its treatments on the subsequent risk of T2D. Additional research is needed to fully understand these associations, particularly, the risk of T2D among premenopausal women with breast cancer, and the risk of T2D according to type of endocrine therapy—i.e., tamoxifen therapy or aromatase inhibitors. Our study highlights that more research is needed on the effects of radiation and anti-human epidermal growth factor receptor-2 (anti-HER2) therapies, which were not a focus in our study. We note that a single study suggested that left-sided radiation therapy was associated with increased risk of T2D, hypothesizing that the elevated risk was due to the proximity of the pancreas to the radiation field [24]. Anti-HER2 therapy is associated with heightened risk of cardiac toxicity, which is also associated with T2D [34]. Breast cancer patients at risk of both cardiovascular disease and T2D may have higher long-term morbidity, stressing the need for studies clarifying the impact of anti-HER2 therapy on the risk of T2D.
Conclusion
In conclusion, this systematic review supports an association between breast cancer and an increased risk of T2D. Nonetheless, our review was limited by the low number of published studies and the potential for surveillance bias regarding T2D status in breast cancer survivors compared with their non-cancer counterparts. Furthermore, few studies reported data on the risk of T2D associated with specific breast cancer treatments, and no studies explicitly investigated the risk of T2D in premenopausal breast cancer patients. Still, the evidence points to increased risk of T2D in breast cancer survivors. Clinicians and those working in cancer survivorship care should consider the benefit of routine blood glucose testing in breast cancer survivors.
Data availability
Enquiries about data availability should be directed to the authors.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin 71(3):209–249
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Lipscombe LL, Chan WW, Yun L, Austin PC, Anderson GM, Rochon PA (2013) Incidence of diabetes among postmenopausal breast cancer survivors. Diabetologia 56(3):476–483
Hwangbo Y, Kang D, Kang M, Kim S, Lee EK, Kim YA, Chang YJ, Choi KS, Jung SY, Woo SM et al (2018) Incidence of diabetes after cancer development: a Korean national cohort study. JAMA Oncol 4(8):1099–1105
Wang CY, Shih SR, Huang KC (2020) Increasing risk of diabetes mellitus in postmenopausal women with newly diagnosed primary breast cancer. J Diabetes Investig 11(2):490–498
Lipscombe LL, Fischer HD, Yun L, Gruneir A, Austin P, Paszat L, Anderson GM, Rochon PA (2012) Association between tamoxifen treatment and diabetes: a population-based study. Cancer 118(10):2615–2622
Sun LM, Chen HJ, Liang JA, Li TC, Kao CH (2014) Association of tamoxifen use and increased diabetes among asian women diagnosed with breast cancer. Br J Cancer 111(9):1836–1842
Wolf I, Sadetzki S, Gluck I, Oberman B, Ben-David M, Papa MZ, Catane R, Kaufman B (2006) Association between diabetes mellitus and adverse characteristics of breast cancer at presentation. Eur J Cancer 42(8):1077–1082
Hamood R, Hamood H, Merhasin I, Keinan-Boker L (2018) Diabetes after hormone therapy in breast cancer survivors: a case-cohort study. J Clin Oncol 36(20):2061–2069
Bordeleau L, Lipscombe L, Lubinski J, Ghadirian P, Foulkes WD, Neuhausen S, Ainsworth P, Pollak M, Sun P, Narod SA (2011) Diabetes and breast cancer among women with BRCA1 and BRCA2 mutations. Cancer 117(9):1812–1818
Nadal A, Alonso-Magdalena P, Soriano S, Quesada I, Ropero AB (2009) The pancreatic β-cell as a target of estrogens and xenoestrogens: implications for blood glucose homeostasis and diabetes. Mol Cell Endocrinol 304(1):63–68
Yan H, Yang W, Zhou F, Li X, Pan Q, Shen Z, Han G, Newell-Fugate A, Tian Y, Majeti R et al (2019) Estrogen improves insulin sensitivity and suppresses gluconeogenesis via the transcription factor Foxo1. Diabetes 68(2):291
Miller WR (2003) Aromatase inhibitors: mechanism of action and role in the treatment of breast cancer. Semin Oncol 30:3–11
Le May C, Chu K, Hu M, Ortega CS, Simpson ER, Korach KS, Tsai M-J, Mauvais-Jarvis F (2006) Estrogens protect pancreatic beta-cells from apoptosis and prevent insulin-deficient diabetes mellitus in mice. Proc Natl Acad Sci USA 103(24):9232–9237
Johansson H, Gandini S, Guerrieri-Gonzaga A, Iodice S, Ruscica M, Bonanni B, Gulisano M, Magni P, Formelli F, Decensi A (2008) Effect of fenretinide and low-dose tamoxifen on insulin sensitivity in premenopausal women at high risk for breast cancer. Cancer Res 68(22):9512–9518
Ye F, Wen J, Yang A, Wang Y, Li N, Yu P, Wei W, Tang J (2021) The influence of hormone therapy on secondary diabetes mellitus in breast cancer: a meta-analysis. Clin Breast Cancer 22:e48–e58
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Dekkers OM, Vandenbroucke JP, Cevallos M, Renehan AG, Altman DG, Egger M (2019) COSMOS-E: guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. PLoS Med 16(2):e1002742
Green MS, Symons MJ (1983) A comparison of the logistic risk function and the proportional hazards model in prospective epidemiologic studies. J Chronic Dis 36(10):715–723
Accordino MK, Wright JD, Buono D, Lin A, Huang Y, Neugut AI, Hillyer GC, Hershman DL (2020) Incidence and predictors of diabetes mellitus after a diagnosis of early-stage breast cancer in the elderly using real-world data. Breast Cancer Res Treat 183(1):201–211
Choi Y-J, Bak K, Yeo Y, Choi Y, Shin S (2021) Incident type 2 diabetes risk of selective estrogen receptor modulators in female patients with breast cancer. Pharmaceuticals 14(9):925
Ji GY, Jin LB, Wang RJ, Bai Y, Yao ZX, Lu LJ, Huang JB, Liu SC, Li HY, Wang ZW et al (2013) Incidences of diabetes and prediabetes among female adult breast cancer patients after systemic treatment. Med Oncol 30(3):687
Juanjuan L, Wen W, Zhongfen L, Chuang C, Jing C, Yiping G, Changhua W, Dehua Y, Shengrong S (2015) Clinical pathological characteristics of breast cancer patients with secondary diabetes after systemic therapy: a retrospective multicenter study. Tumour Biol 36(9):6939–6947
Kwan ML, Cheng RK, Iribarren C, Neugebauer R, Rana JS, Nguyen-Huynh M, Shi Z, Laurent CA, Lee VS, Roh JM et al (2022) Risk of cardiometabolic risk factors in women with and without a history of breast cancer: the pathways heart study. J Clin Oncol 0(0):JCO2101738
Ng HS, Koczwara B, Roder D, Niyonsenga T, Vitry A (2018) Incidence of comorbidities in women with breast cancer treated with tamoxifen or an aromatase inhibitor: an australian population-based cohort study. J Comorb 8(1):16–24
Ng HS, Koczwara B, Roder DM, Niyonsenga T, Vitry AI (2018) Comorbidities in australian women with hormone-dependent breast cancer: a population-based analysis. Med J Aust 208(1):24–28
Rao S, Prasad K, Abraham S, George T, Chandran SK, Baliga MS (2020) Incidence of hyperglycemia/secondary diabetes in women who have undergone curative chemotherapy for breast cancer: first study from India. South Asian J Cancer 9(3):130–135
Santorelli ML, Hirshfield KM, Steinberg MB, Rhoads GG, Lin Y, Demissie K (2016) Hormonal therapy for breast cancer and diabetes incidence among postmenopausal women. Ann Epidemiol 26(6):436–440
Tamez-Pérez HE, Quintanilla-Flores DL, Rodríguez-Gutiérrez R, González-González JG, Tamez-Peña AL (2015) Steroid hyperglycemia: prevalence, early detection and therapeutic recommendations: a narrative review. World J Diabetes 6(8):1073–1081
Hwang JL, Weiss RE (2014) Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment. Diabetes Metab Res Rev 30(2):96–102
Vance V, Mourtzakis M, McCargar L, Hanning R (2011) Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev 12(4):282–294
Winer EP, Hudis C, Burstein HJ, Wolff AC, Pritchard KI, Ingle JN, Chlebowski RT, Gelber R, Edge SB, Gralow J et al (2005) American society of clinical oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor–positive breast cancer: status report 2004. J Clin Oncol 23(3):619–629
Nyrop KA, Williams GR, Muss HB, Shachar SS (2016) Weight gain during adjuvant endocrine treatment for early-stage breast cancer: what is the evidence? Breast Cancer Res Treat 158(2):203–217
Dang C, Guo H, Najita J, Yardley D, Marcom K, Albain K, Rugo H, Miller K, Ellis M, Shapira I et al (2016) Cardiac outcomes of patients receiving adjuvant weekly paclitaxel and trastuzumab for node-negative, ERBB2-positive breast cancer. JAMA Oncol 2(1):29–36
Funding
This work was funded by the Novo Nordisk Foundation STENO Collaborative Grant (grant number NNF20OC0065928), the Danish Cancer Society (grant number R328-A19070), and the Elvira and Rasmus Riisforts Foundation.
Author information
Authors and Affiliations
Contributions
Deirdre Cronin-Fenton conceived the study idea. The study protocol was written by Nanna Jordt. Literature search was performed by Nanna Jordt and Kasper Kjærgaard. Data analysis was performed by Nanna Jordt. The manuscript was mainly drafted by Nanna Jordt and critically revised by all authors (Kasper Kjærgaard, Reimar W. Thomsen, Signe Borgquist and Deirdre Cronin-Fenton).
Corresponding author
Ethics declarations
Competing interests
The authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jordt, N., Kjærgaard, K.A., Thomsen, R.W. et al. Breast cancer and incidence of type 2 diabetes mellitus: a systematic review and meta-analysis. Breast Cancer Res Treat 202, 11–22 (2023). https://doi.org/10.1007/s10549-023-07043-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07043-6