Abstract
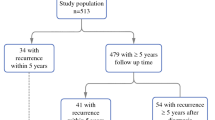
Evaluation of prognostic factors in lymph node negative (LNneg) invasive lobular cancers (ILCs). Prospective analysis of proliferation and other prognosticators in 121 LNneg ILCs (119 months median follow-up, range 19–181), without adjuvant chemotherapy. ILC subtype was assessed in accordance with WHO-2003 criteria. Immunohistochemical E-cadherin and estrogen receptor were used. With a median follow up time of 83 months (range 19–181), 30 of the 121 (25%) ILC patients developed distant metastases and 27 (22%) died. None of the cases classified as solid/pleomorphic lobular were E-cadherin or estrogen receptor positive, contrasting the other ILCs. The solid/alveolar ILCs (n = 17) had a worse survival (50%) than the other ILCs (n = 104; 83%, P < 0.0001). Mitotic activity index (MAI) (but not nuclear grade or tubule formation) was prognostic with a threshold 0–5 versus >5 (=MAI-5) (contrasting MAI < 10 vs. ≥10 in breast cancers in general; 85 and 54% survival, P < 0.0001). In multivariate analysis only subtype and MAI but none of the other characteristics had independent prognostic value. Histologic subtype and MAI have independent prognostic value in node negative invasive lobular cancers.



Similar content being viewed by others
References
Ellis IO, Schnitt SJ, Sastre-Garau X (2003) Invasive breast carcinoma. In: Tavassoli FA, Devilee P et al (eds) Pathology and genetics of tumours of the breast and female genital organs: WHO classification of tumours series. IARC press, Lyon, pp 13–48
Mathieu MC, Rouzier R, Llombart-Cussac A et al (2004) The poor responsiveness of infiltrating lobular breast carcinomas to neoadjuvant chemotherapy can be explained by their biological profile. Eur J Cancer 40:342–351. doi:10.1016/j.ejca.2003.08.015
Cocquyt V, Van Belle S (2005) Lobular carcinoma in situ and invasive lobular cancer of the breast. Curr Opin Obstet Gynecol 17:55–60. doi:10.1097/00001703-200502000-00010
Dixon JM, Anderson TJ, Page DL et al (1982) Infiltrating lobular carcinoma of the breast. Histopathology 6:149–161. doi:10.1111/j.1365-2559.1982.tb02712.x
Arpino G, Bardou VJ, Clark GM, Elledge RM (2004) Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res 6:R149–R156. doi:10.1186/bcr767
Reis-Filho JS, Simpson PT, Jones C, Steele D, Mackay A, Iravani M et al (2005) Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol 207:1–13. doi:10.1002/path.1806
Baak JP, van Diest PJ, Voorhorst FJ, van der Wall E, Beex LV, Vermorken JB et al (2005) Prospective multicenter validation of the independent prognostic value of the mitotic activity index in lymph node-negative breast cancer patients younger than 55 years. J Clin Oncol 23(25):5993–6001. doi:10.1200/JCO.2005.05.511
Baak JP, van Diest PJ, Janssen EA et al (2008) Proliferation accurately identifies the high-risk patients among small, low-grade, lymph node-negative invasive breast cancers. Ann Oncol 19(4):649–654. doi:10.1093/annonc/mdm535
McShane LM, Altman DG, Sauerbrei W et al (2005) Reporting recommendations for tumor marker studies. J Clin Oncol 23(36):9067–9072
Baak JPA, Snijders W, van Diermen B et al (2003) Prospective multicenter validation confirms the prognostic superiority of the ECPI in FIGO-1 endometrial carcinoma. J Clin Oncol 23:4214–4221. doi:10.1200/JCO.2003.02.087
Jannink I, Bennen JN, Blaauw J et al (1995) At convenience and systematic random sampling: effects on the prognostic value of nuclear area assessments in breast cancer patients. Breast Cancer Res Treat 36:55–60. doi:10.1007/BF00690185
Fleege JC, van Diest PJ, Baak JPA (1993) Systematic random sampling for selective interactive nuclear morphometry in breast cancer sections. Refinement and multiobserver evaluation. Anal Quant Cytol Histol 15:281–289
Skaland I, van Diest PJ, Janssen EAM et al (2008) Prognostic differences of WHO-assessed mitotic activity index (MAI) and mitotic impression by quick scanning in invasive ductal breast cancer patients under 55 years of age. Hum Pathol 39(4):584–590. doi:10.1016/j.humpath.2007.08.016
Rakha EA, El-Sayed ME, Menon S et al (2008) Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 111(1):121–127 (Epub 2007 Oct 11)
Acknowledgments
The MMMCP study is supported by grant #28-1398 of the Zorg Onderzoek Nederland (ZON) and grants #06-212 and 07-218 of the SBDM. Besides the authors, the project has been made possible by the continuing collaboration of all the specialists, bioengineers and administrative collaborators of the MMMCP project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gudlaugsson, E., Skaland, I., Janssen, E.A.M. et al. Prospective multicenter comparison of proliferation and other prognostic factors in lymph node negative lobular invasive breast cancer. Breast Cancer Res Treat 121, 35–40 (2010). https://doi.org/10.1007/s10549-009-0442-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0442-x