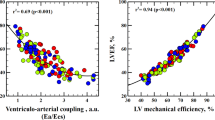
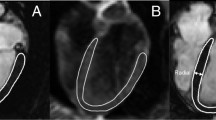
The cardiohemodynamics was studied 2 and 4 weeks after myocardial infarction modeling in Wistar rats. We compared the data obtained by echocardiography (echoCG) and catheterization of the left ventricle. The myocardial infarction was modeled by ligation of the left anterior descending coronary artery. EchoCG and the left ventricle catheterization were performed before and after myocardial infarction modeling. Similar results were obtained by both methods, namely the left ventricle dilatation, bradycardia, a reduced ejection fraction and delayed relaxation. According to echoCG, the end-diastolic left ventricle volume increased by 2 times, and initial diastolic left ventricle volume — by more than 5 times. The left ventricle catheterization showed lower rise, by 32 and 69%, respectively. The overestimated volume of the left ventricle in myocardial infarction according to echoCG data in comparison with catheterization can be explained by changes in the geometry of the ventricle (bulging of a part of the ventricular wall).
Similar content being viewed by others
References
Onai Y, Suzuki J, Maejima Y, Haraguchi G, Muto S, Itai A, Isobe M. Inhibition of NF-{kappa}B improves left ventricular remodeling and cardiac dysfunction after myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2007;292(1):H530-H538. https://doi.org/10.1152/ajpheart.00549.2006
Kanashiro RM, Nozawa E, Murad N, Gerola LR, Moisés VA, Tucci PJ. Myocardial infarction scar plication in the rat: cardiac mechanics in an animal model for surgical procedures. Ann. Thorac. Surg. 2002;73(5):1507-1513. https://doi.org/10.1016/s0003-4975(01)03416-6
Solomon SD, Glynn RJ, Greaves S, Ajani U, Rouleau JL, Menapace F,Arnold JM, Hennekens C, Pfeffer MA. Recovery of ventricular function after myocardial infarction in the reperfusion era: the healing and early afterload reducing therapy study. Ann. Intern. Med. 2001;134(6):451-458. https://doi.org/10.7326/0003-4819-134-6-200103200-00009
Sjöblom J, Muhrbeck J, Witt N, Alam M, Frykman-Kull V. Evolution of left ventricular ejection fraction after acute myocardial infarction: implications for implantable cardioverter-defibrillator eligibility. Circulation. 2014;130(9):743-748. https://doi.org/10.1161/CIRCULATIONAHA.114.009924
Marwick TH. Ejection fraction pros and cons: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2018;72(19):2360-2379. https://doi.org/10.1016/j.jacc.2018.08.2162.
Gerber Y, Weston SA, Berardi C, McNallan SM, Jiang R, Redfield MM, Roger VL. Contemporary trends in heart failure with reduced and preserved ejection fraction after myocardial infarction: a community study. Am. J. Epidemiol. 2013;178(8):1272-1280. https://doi.org/10.1093/aje/kwt109
Eskander M, Kern MJ. Invasive hemodynamics of myocardial disease: systolic and diastolic dysfunction (and hypertrophic obstructive cardiomyopathy). Interv. Cardiol. Clin. 2017;6(3):297-307. https://doi.org/10.1016/j.iccl.2017.03.001
Sanderson JE. Heart failure with a normal ejection fraction. Heart. 2007;93(2):155-158. https://doi.org/10.1136/hrt.2005.074187
Gonçalves AF, Congio LH, dos Santos PP, Rafacho BP, Pereira BL, Claro RF, Costa NA, Chiuso-Minicucci F, Azevedo PS, Polegato BF, Okoshi K, Pereira EJ, Okoshi MP, Paiva SA, Zornoff LA, Minicucci MF. Pamidronate attenuates diastolic dysfunction induced by myocardial infarction associated with changes in geometric patterning. Cell Physiol. Biochem. 2015;35(1):259-269. https://doi.org/10.1159/000369693
Røe ÅT, Ruud M, Espe EK, Manfra O, Longobardi S, Aronsen JM, Nordén ES, Husebye T, Kolstad TRS, Cataliotti A, Christensen G, Sejersted OM, Niederer SA, Andersen GØ, Sjaastad I, Louch WE. Regional diastolic dysfunction in post-infarction heart failure: role of local mechanical load and SERCA expression. Cardiovasc. Res. 2019;115(4):752-764. https://doi.org/10.1093/cvr/cvy257
Tomoaia R, Beyer RS, Simu G, Serban AM, Pop D. Understanding the role of echocardiography in remodeling after acute myocardial infarction and development of heart failure with preserved ejection fraction. Med. Ultrason. 2019;21(1):69-76. https://doi.org/10.11152/mu-1768
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Byulleten’ Eksperimental’noi Biologii i Meditsiny, Vol. 176, No. 9, pp. 299-302, September, 2023
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abramov, A.A., Prosvirnin, A.V., Lakomkin, V.L. et al. Noninvasive and Invasive Study of the Pumping Function of Rat Heart in Myocardial Infarction. Bull Exp Biol Med 176, 321–323 (2024). https://doi.org/10.1007/s10517-024-06016-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10517-024-06016-z