Abstract
Slow paced breathing has been demonstrated to provide significant health benefits for a person’s health, and, during breathing sessions, it is desirable to monitor that a person is actually compliant with the breath pacer. We explore the potential use of pulse rate variability to monitor compliance with a breath pacer during meditation sessions. The study involved 6 human subjects each participating in 2–3 trials, where they are asked to follow or not to follow the breath pacer, where we collected data on how the magnitude of pulse rate variability changed. Two methods, logistic regression and a running standard deviation technique, were developed to detect non-compliance with the breath pacer based on pulse rate variability metrics. Results indicate that using pulse rate variability alone may not reliably detect non-compliance with the breath pacer. Both models exhibited limitations in terms of false positives and false negatives, with accuracy ranging from 67 to 65%. Existing methods involving visual, audio, and motion signals currently perform better for monitoring compliance with the breath pacer.
Similar content being viewed by others
Introduction
Slow paced-breathing has recently gained increasing recognition for its potential to improve an individual’s health and overall well being. Specifically, it has been shown that such breathing can significantly lower the blood pressure (Schein et al., 2001; Grossman et al., 2001; Rosenthal et al., 2001; van Hateren et al., 2014; Elliot et al., 2004; Meles et al., 2004; Landman et al., 2014; Schein et al., 2009; Altena et al., 2009), lower neural sympathetic activity (Oneda el at., 2010; Harada et al., 2014; Barros et al., 2014), decrease peripheral resistance (Gavish et al., 2011; Ovadia-Blechman et al., 2017; Faconti et al., 2019; Bachler et al., 2020) and arterial stiffness (Parati et al., 2008; Ekman et al., 2011; Bilo et al., 2012; Debicka-Dabrowska et al., 2015) as well as reduce anxiety and stress (Morarend et al., 2011; Ouseph et al., 2014; Gabriely et al., 2020). Slow paced breathing has also been utilized for Heart Rate Variability Biofeedback (HRVB) which involves training individuals to control their heart rate using slow breathing patterns (Lehrer et al., 2014). There has been innovative work done that shows benefits and positive effects of HRVB for one’s health and overall well being (Aschbacher et al., 2023; Lehrer et al., 2020; Goessl et al., 2017). There are many devices that can guide slow breathing (Miri et al., 2020; Martin et al., 2014; Kirby et al., 2009). However, it is important to monitor that the user is actually following the guided breathing pattern (Benetazzo et al., 2014), as it is common for people to get distracted and deviate from the breathing rate of the breath pacer.
In this light, several existing techniques, that used image (Nam et al., 2016a), sound (Nam et al., 2016b; Avalur, 2013) or motion recognition (Hernandez et al., 2015; Shen et al., 2017; Prigent et al., 2021), have been used in order to determine the breathing rate of the person. Specifically, such techniques as extracting breathing rate from image recognition (Benetazzo et al., 2014, Nam et al., 2016a) have demonstrated outstanding performance. For example, there exists an FDA-approved device, RESPeRATE that can detect a person’s breathing rate using a chest strap (Anderson et al., 2009). Such data then can be used to judge if the person’s breathing is compliant with the breath pacer during a meditation session (Zhang et al., 2013).
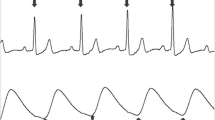
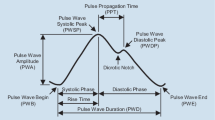
In this paper we explored the possibility of using pulse rate variability to determine compliance with a breath pacer. Recently, a novel technique to calculate the magnitude of pulse rate variability has been developed known as Dynamic Phase Extraction (DPE) (Li et al., 2022). DPE calculates how much the pulse rate of a person varies during a single breath due to respiratory sinus arrhythmia as well as its phase shift relative to breath (Fig. 1). The magnitude drops significantly (Fig. 3a) as a person stops following the breath pacer and starts breathing at their own rate. Therefore, in this study we explored the possibility of using Dynamic Phase Extraction and change in magnitude of the pulse rate variability in order to determine the compliance with the breath pacer.
Experimental Methods
The device (control unit) (Fig. 2) that was used in the study consisted of a WEMOS LOLIN 32 board, Seeed Studio earclip pulse sensor, and a WCMCU-2812-7 board with 6 LED lights mounted on it. The WEMOS LOLIN 32 board was put in a metal case. Three wires were coming out of the case: one to power and read the signal from the pulse sensor, one to power and control breath pacer, and a micro USB cable that was connected to the desktop computer to power the device and collect the data from it.
Experimental setup including device (control unit) with breath pacer and ear clip pulse sensor, and computer for data collection. Participant is seated in front of the computer in a padded chair and is wearing an ear clip pulse sensor. Participant is following a visual breath pacer and is guided to breathe according to the instructions on the computer screen with a timer
The LED board was put in a white 3D printed oval shell, and attached to its inner surface such that the brightness of the light would be distinguishable through the shell. The breath pace was set using the brightness of the LEDs: increasing brightness meant inhale, and decreasing brightness meant exhale. The breath length was set to 10 s during all trials in the study.
Using collected pulse data and Dynamic Phase Extraction (DPE) Algorithm, the device computed the magnitude and phase of the pulse rate variability (PRV). Computed magnitude and phase along with timestamps of the breath were sent to the desktop computer with a serial communication. It received data using a Python Program, and saved it. This program also provided a graphical user interface that displayed directions on whether the subject had to or did not have to follow the breath pacer.
The study procedure was approved for use by the Human Subjects Committee through the University of California, Santa Barbara. The study was conducted throughout a one week period of 3 sessions on 3 different days of the week. Six participants (3 male and 3 female) of ages 18–24 were chosen for the study among current University of California, Santa Barbara students via major department mailing lists. Participants were contacted regarding the procedure of the study and asked to complete a consent form before receiving any other information. All subjects were also asked to complete an assessment form prior to enrollment in the study to verify any chronic medical conditions. None of the participants had listed any chronic medical conditions. Before the start of data collection, participants were briefed on the purpose and process to completing the study. Participants were seated in front of the computer in a padded chair and connected to the ear clip pulse sensor. The pulse sensor was attached to either the right or left earlobe. Participants were given a visual breath pacer described above and guided to breathe according to the instructions on the computer screen with a timer. For the first 2 min of the session, instructions asked the participants to follow the breath pacer. For the next 1 min, instructions asked the participants to breathe at their own pace. Such a pattern repeated for the whole duration of a 12 min session. Timer on the screen showed how much time was left for each part of the session as well as for the whole session. Change of the instructions on the screen was accompanied by a sound notification to make sure that the participants change their breathing pace at the correct times. Once the session was over, participants were given $5 in cash for compensation.
The data that were collected in the study consisted of data points that included magnitude and phase of pulse rate variability, pulse rate values, digital pulse signal, and corresponding times relative to the start of the session (trial). Data points were collected at a rate of 1 data point per 15 milliseconds. The magnitude and phase, however, were only computed once per breath cycle (10 s). We also collected binary data that told in which region of the session the subject was or was not following the breath pacer.
Once the data were collected for every session, it was rescaled such that a single data point corresponded to a single breath. The primary metric was the magnitude of the pulse rate variability. For each data point (breath) we computed the average and the standard deviation of the magnitude over the previous 4 breaths. We then introduced 3 metrics (each for a given breath): change of magnitude with respect to average over previous 4 breaths excluding current; ratio of change of magnitude with respect to average over previous 4 breaths excluding current to the standard deviation computed over the same interval; ratio of change of magnitude with respect to average over previous 4 breaths including current to the standard deviation computed over the same interval.
Using these metrics, we explored two possible models to detect non-compliance with the breath pacer. In the first technique, we trained a linear regression model with Python scikit-learn library, where the output was trained based on collected binary data of subjects either being compliant with the breath pacer or not.
In the second technique (later referred as running standard deviation technique), we computed the ratio of change of magnitude with respect to average over previous 4 breaths excluding current to the standard deviation computed over the same interval; ratio of change of magnitude with respect to average over previous 4 breaths including current to the standard deviation computed over the same interval. If the former exceeded 1.8 and the latter exceeded 3, we assumed that the subject’s breath was not compliant with the breath pacer. These thresholds were determined experimentally to yield the best accuracy of the algorithm.
Results
We tested how well the models performed on the collected data. The key assumption was that the in-phase with breathing component of pulse rate variability was dropping significantly as the person stopped following the breath pacer and started breathing at his or her own rate (Fig. 3a). However, as was revealed during the study, this approach does not work for all people. For example, if a person has low pulse rate variability (Fig. 3b), then such a method cannot be used to reliably detect compliance with the breath pacer.
The magnitude of the pulse rate variability (PRV) that is in-phase with the breath pacer, also known as the magnitude of the Respiratory Sinus Arrhythmia (RSA). Subject with large PRV (3a): when the person stops following the breath pacer, the magnitude drops significantly which can be used to identify non-compliance with the breath pacer. Subject with low PRV (3b): magnitude does not correlate well with following or not following the breath pacer, which makes it hard to make a detection
We present the performance of both logistic regression and running standard deviation (Fig. 4a and b correspondingly). Here the red bars denote the points in the session where an algorithm detects non-compliance with the breath pacer. The logistic regression model tended to have a lot of false positive detections, while running standard deviation tended to have more false negative detections. Quantitatively, we can describe each model with a confusion matrix (Fig. 5.) Here true positive is defined as correct detection of non-compliance, false positive is defined as incorrect detection of non-compliance, true negative is defined as correct detection compliance, and false negative is incorrect detection of compliance. From the confusion matrices we can compute an accuracy, defined as (True Positive + True Negative)/(True Positive + True Negative + False Positive + False Negative) (Fig. 5), for each model. The values are 67% for logistic regression technique, and 65% for running standard deviation technique.
Detection of non-compliance with the breath pacer for different trials from the model based on logistic regression technique (4a) and running standard deviation technique (4b). Thicker detection bars indicate that the model detects non-compliance for several breaths in a row. Logistic regression model tended to have more false positive detections, while running standard deviation tended to have more false negative detections
Confusion matrix for logistic regression technique (5a) and running standard deviation technique (5b). True positive is defined as correct detection of non-compliance, false positive is defined as incorrect detection of non-compliance, true negative is defined as correct detection of compliance, and false negative is incorrect detection of compliance
Here we also present the cumulative distribution of the device detections over the whole session for all subjects. Overall, we can see that both logistic regression (Fig. 6a) and running standard deviation (Fig. 6b) exhibit a trend and cluster around regions of non-compliance with the breath pacer. However, quantitatively, it is difficult to use such data for detection of non-compliance with the breath pacer.
Discussion
In this study we have collected and analyzed that data from 6 subjects, where each subject participated in 2–3 trials (sessions). Overall, we were able to identify that our assumption that pulse rate variability can be used in order to detect non-compliance with the breath pacer was not valid for the majority of subjects. Although the models performed relatively well for some (for example, trial #1 on Fig. 4a or trial #3 on Fig. 4b), both models failed for most of the subjects. Based on these results, we can confirm that existing methods can demonstrate much better results for the purpose of breath pacer compliance and breathing rate detection (Benetazzo et al., 2014; Nam et al., 2016a, b; Avalur, 2013; Hernandez et al., 2015; Shen et al., 2017; Prigent et al., 2021).
Our study contained several limitations that could potentially be eliminated in further research. One issue is that we were not controlling the true (e.g. actual) breathing rate of people. Here, we implicitly assumed that people were indeed following the breath pacer and were breathing at a specific frequency, although we have no real data to confirm it. In the future studies, we would like to use some independent metric such as a chest strap sensor to measure the true breathing rate of the subject.
Conclusion
In conclusion, in this paper we presented the description of the study on exploring the possibility of using the pulse rate variability in order to monitor the compliance with the breath pacer for people during meditation sessions. The device that was used in the study collected data concerning the pulse rate and magnitude of pulse rate variability of subjects, and actual compliance of the participants with the breath pacer. Specific metrics were derived from these data in order to create an algorithm to detect compliance with a breath pacer using just pulse rate and pulse rate variability data. We constructed two techniques, one based on logistic regression, and the other based on running standard deviation. The accuracy of both models was around 67% and 65% respectively, suggesting that pulse rate variability might be not the best metric in order to monitor compliance with the breath pacer, and that existing methods involving visual, audio, and motion signals perform better (Benetazzo et al., 2014; Nam et al., 2016a, b; Avalur, 2013; Hernandez et al., 2015; Shen et al., 2017; Prigent et al., 2021). We have also highlighted the limitations of the study, particularly the assumption that subjects followed breath pacer accurately, which may not always hold true. In summary, this study provided valuable insights into the challenges and complexities of using pulse rate variability in order to detect compliance with the breath pacer, and suggested that existing methods perform significantly better for this purpose.
References
Altena, M., Kleefstra, N., Logtenberg, S., Groenier, K., Houweling, S., & Bilo, H. (2009). Effect of device-guided breathing exercises on blood pressure in patients with Hypertension: A randomized controlled trial. Blood Pressure, 18(5), 273–279. https://doi.org/10.1080/08037050903272925
Anderson, D. E., McNeely, J. D., & Windham, B. G. (2009). Device-guided slow-breathing effects on end-tidal CO2 and heart-rate variability. Psychology Health & Medicine, 14(6), 667–679. https://doi.org/10.1080/13548500903322791
Aschbacher, K., Mather, M., Lehrer, P., Gevirtz, R., Epel, E., & Peiper, N. C. (2023, March 18). Toward Digital Precision Care: Large-scale Age and Gender Norms for Heart Rate Variability Biofeedback Metrics from a Real-World Digital Mental Health Intervention. https://doi.org/10.31234/osf.io/47up5
Avalur, D. S. (2013). Human breath detection using a microphone (Doctoral dissertation, Faculty of Science and Engineering).
Bachler, M., Sehnert, W., Mikisek, I., Wassertheurer, S., & Mengden, T. (2020). Non-invasive quantification of the effect of device-guided slow breathing with direct feedback to the patient to reduce blood pressure. Physiological Measurement, 41(10), 104002–104002. https://doi.org/10.1088/1361-6579/abb320
Barros, S., Silva, G. V., Gusmão, J. L., Araujo, T. G., & Mion, D. (2014). Reduction of sympathetic nervous activity with device-guided breathing. The Journal of Clinical Hypertension (Greenwich Conn), 16(8), 614–615. https://doi.org/10.1111/jch.12360
Benetazzo, F., Freddi, A., Monteriù, A., & Longhi, S. (2014). Respiratory rate detection algorithm based on RGB-D camera: Theoretical background and experimental results. Healthcare Technology Letters, 1(3), 81–86. https://doi.org/10.1049/htl.2014.0063
Bilo, G., Revera, M., Bussotti, M., Bonacina, D., Styczkiewicz, K., Caldara, G., Giglio, A., Faini, A., Giuliano, A., Lombardi, C., Kawecka-Jaszcz, K., Mancia, G., Agostoni, P., & Parati, G. (2012). Effects of slow deep breathing at high altitude on oxygen saturation, pulmonary and systemic hemodynamics. PloS One, 7(11), e49074–e49074. https://doi.org/10.1371/journal.pone.0049074
Debicka-Dabrowska, D., Lisi, E., Drozdz, T., Styczkiewicz, K., Malfatto, G., Salerno, S., Bednarek, A., Olszanecka, A., Kielbasa, G., Bilo, G., Czarnecka, D., Kawecka-Jaszcz, K., & Parati, G. (2015). PP.36.04: Usefulness of slow breathing training in chronic heart failure. Study design and intermediate results. Journal of Hypertension, 33(Supplement 1), e462. https://doi.org/10.1097/01.hjh.0000468837.88331.16
Ekman, I., Kjellström, B., Falk, K., Norman, J., & Swedberg, K. (2011). Impact of device-guided slow breathing on symptoms of chronic Heart Failure: A randomized, controlled feasibility study. European Journal of Heart Failure, 13(9), 1000–1005. https://doi.org/10.1093/eurjhf/hfr090
Elliott, W. J., Izzo, J. L., White, W. B., Rosing, D. R., Snyder, C. S., Alter, A., Gavish, B., & Black, H. R. (2004). Graded blood pressure reduction in Hypertensive outpatients Associated with Use of a device to assist with slow breathing. The Journal of Clinical Hypertension (Greenwich Conn), 6(10), 553–559. https://doi.org/10.1111/j.1524-6175.2004.03553.x
Faconti, L., Farukh, B., McNally, R., Webb, A., & Chowienczyk, P. (2019). Arterial stiffness can be modulated by pressure-independent mechanisms in Hypertension. Journal of the American Heart Association, 8(15), e012601–e012601. https://doi.org/10.1161/JAHA.119.012601
Gabriely, R., Tarrasch, R., Velicki, M., & Ovadia-Blechman, Z. (2020). The influence of mindfulness meditation on inattention and physiological markers of stress on students with learning disabilities and/or attention deficit hyperactivity disorder. Research in Developmental Disabilities, 100, 103630–103630. https://doi.org/10.1016/j.ridd.2020.103630
Gavish, B., Alter, A., Barkai, Y., et al. (2011). Effect of non-drug interventions on arterial properties determined from 24-h ambulatory blood pressure measurements. Hypertension Research, 34, 1233–1238. https://doi.org/10.1038/hr.2011.125
Goessl, V. C., Curtiss, J. E., & Hofmann, S. G. (2017). The effect of heart rate variability biofeedback training on stress and anxiety: A meta-analysis. Psychological Medicine, 47(15), 2578–2586. https://doi.org/10.1017/S0033291717001003
Grossman, E., Grossman, A., Schein, M. H., Zimlichman, R., & Gavish, B. (2001). Breathing-control lowers blood pressure. Journal of Human Hypertension, 15(4), 263–269. https://doi.org/10.1038/sj.jhh.1001147
Harada, D., Asanoi, H., Takagawa, J., Ishise, H., Ueno, H., Oda, Y., Goso, Y., Joho, S., & Inoue, H. (2014). Slow and deep respiration suppresses steady-state sympathetic nerve activity in patients with chronic Heart Failure: From modeling to clinical application. American Journal of Physiology Heart and Circulatory Physiology, 307(8), H1159–H1168. https://doi.org/10.1152/ajpheart.00109.2014
Hernandez, J., McDuff, D., & Picard, R. W. (2015). Biowatch: Estimation of heart and breathing rates from wrist motions. 2015 9th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth), 1(3), 169–176. https://doi.org/10.4108/icst.pervasivehealth.2015.259064
Kirby, T., Baloa, L. A., & Witt, E. K. (2009). U.S. Patent No. 7,556,038. Washington, DC: U.S. Patent and Trademark Office.
Landman, G. W., van Hateren, K. J., van Dijk, P. R., Logtenberg, S. J., Houweling, S. T., Groenier, K. H., … Kleefstra, N. (2014). Efficacy of device-guided breathing for hypertension in blinded, randomized, active-controlled trials: a meta-analysis of individual patient data. JAMA internal medicine, 174(11), 1815–1821. https://doi.org/10.1001/jamainternmed.2014.4336
Lehrer, P. M., & Gevirtz, R. (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5, 756–756. https://doi.org/10.3389/fpsyg.2014.00756
Lehrer, P., Kaur, K., Sharma, A., Shah, K., Huseby, R., Bhavsar, J., Sgobba, P., & Zhang, Y. (2020). Heart Rate Variability Biofeedback improves emotional and physical health and performance: A systematic review and Meta Analysis. Applied Psychophysiology and Biofeedback, 45(3), 109–129. https://doi.org/10.1007/s10484-020-09466-z
Li, C. H., Ly, F. S., Woodhouse, K., Chen, J., Cheng, Z., Santander, T., Ashar, N., Turki, E., Yang, H. T., Miller, M., Petzold, L., & Hansma, P. K. (2022). Dynamic phase extraction: Applications in pulse rate variability. Applied Psychophysiology and Biofeedback, 47(3), 213–222. https://doi.org/10.1007/s10484-022-09549-z
Martin, D. C. C., & Bassin, D. J. (2014). U.S. Patent No. 8,844,527. Washington, DC: U.S. Patent and Trademark Office.
Meles, E., Giannattasio, C., Failla, M., Gentile, G., Capra, A., & Mancia, G. (2004). Nonpharmacologic treatment of Hypertension by respiratory exercise in the home setting. American Journal of Hypertension, 17(4), 370–374. https://doi.org/10.1016/j.amjhyper.2003.12.009
Miri, P., Flory, R., Uusberg, A., Culbertson, H., Harvey, R. H., Kelman, A., Peper, D., Gross, J., Isbister, K., & Marzullo, K. (2020). PIV: Placement, Pattern, and personalization of an inconspicuous Vibrotactile Breathing Pacer. ACM Transactions on Computer-Human Interaction, 27(1), 1–44. https://doi.org/10.1145/3365107
Morarend, Q. A., Spector, M. L., Dawson, D. V., Clark, S. H., & Holmes, D. C. (2011). The Use of a respiratory rate Biofeedback device to Reduce Dental anxiety: An exploratory investigation. Applied Psychophysiology and Biofeedback, 36(2), 63–70. https://doi.org/10.1007/s10484-011-9148-z
Nam, Y., Kong, Y., Reyes, B., Reljin, N., & Chon, K. H. (2016a). Monitoring of Heart and Breathing Rates using dual cameras on a smartphone. PloS One, 11(3), e0151013–e0151013. https://doi.org/10.1371/journal.pone.0151013
Nam, Reyes, B. A., & Chon, K. H. (2016b). Estimation of respiratory rates using the built-in microphone of a smartphone or headset. IEEE Journal of Biomedical and Health Informatics, 20(6), 1493–1501. https://doi.org/10.1109/JBHI.2015.2480838
Oneda, B., Ortega, K. C., Gusmao, J. L., Araujo, T. G., & Mion, D. (2010). Sympathetic nerve activity is decreased during device-guided slow breathing. Hypertension Research, 33(7), 708–712. https://doi.org/10.1038/hr.2010.74
Ouseph, R., Croy, C., Natvig, C., Simoneau, T., & Laudenslager, M. L. (2014). Decreased mental health care utilization following a psychosocial intervention in caregivers of hematopoietic stem cell transplant patients. Mental Illness, 6(1). https://doi.org/10.4081/mi.2014.5120
Ovadia-Blechman, Z., Gavish, B., Levy-Aharoni, D., Shashar, D., & Aharonson, V. (2017). The coupling between peripheral microcirculation and slow breathing. Medical Engineering & Physics, 39, 49–56. https://doi.org/10.1016/j.medengphy.2016.10.009
Parati, G., Malfatto, G., Boarin, S., Branzi, G., Caldara, G., Giglio, A., … Mancia, G. (2008). Device-guided paced breathing in the home setting: effects on exercise capacity, pulmonary and ventricular function in patients with chronic heart failure:a pilot study. Circulation: Heart Failure, 1(3), 178–183. https://doi.org/10.1161/CIRCHEARTFAILURE.108.772640
Prigent, G., Aminian, K., Rodrigues, T., Vesin, J. M., Millet, G. P., Falbriard, M., Meyer, F., & Paraschiv-Ionescu, A. (2021). Indirect estimation of Breathing Rate from Heart Rate Monitoring System during running. Sensors (Basel Switzerland), 21(16), 5651. https://doi.org/10.3390/s21165651
Rosenthal, T., Alter, A., Peleg, E., & Gavish, B. (2001). Device-guided breathing exercises reduce blood pressure: Ambulatory and home measurements. American Journal of Hypertension, 14(1), 74–76. https://doi.org/10.1016/S0895-7061(00)01235-8
Schein, M. H., Gavish, B., Herz, M., Rosner-Kahana, D., Naveh, P., Knishkowy, B.,… Melmed, R. N. (2001). Treating hypertension with a device that slows and regularizes breathing: a randomized, double-blind controlled study. Journal of human hypertension, 15(4), 271–278. https://doi.org/10.1038/sj.jhh.1001148
Schein, M. H., Gavish, B., Baevsky, T., Kaufman, M., Levine, S., Nessing, A., & Alter, A. (2009). Treating Hypertension in type II diabetic patients with device-guided breathing: A randomized controlled trial. Journal of Human Hypertension, 23(5), 325–331. https://doi.org/10.1038/jhh.2008.135
Shen, C. L., Huang, T. H., Hsu, P. C., Ko, Y. C., Chen, F. L., Wang, W. C., Kao, T., & Chan, C. T. (2017). Respiratory rate estimation by using ECG, Impedance, and Motion sensing in Smart Clothing. Journal of Medical and Biological Engineering, 37(6), 826–842. https://doi.org/10.1007/s40846-017-0247-z
van Hateren, K. J., Landman, G. W., Logtenberg, S. J., Bilo, H. J., & Kleefstra, N. (2014). Device-guided breathing exercises for the treatment of Hypertension: An overview. World Journal of Cardiology, 6(5), 277–282. https://doi.org/10.4330/wjc.v6.i5.277
Zhang, Z. B., Wu, H., Zheng, J. W., Wang, W. D., Wang, B. Q., Liu, H. Y., & Wang, G. J. (2013). A wearable biofeedback system supporting real-time paced breathing training and physiological monitoring. Biomedical Engineering: Applications Basis and Communications, 25(02), 1350018. https://doi.org/10.1089/tmj.2010.0182
Acknowledgements
We thank Chris Li and his collaborators for developing Dynamic Phase Extraction (DPE). We thank Franklin Ly for technical assistance. We thank Zongren Zhang for help in prototyping and development of the device. We thank Professor Deborah Fygenson for establishing the Physics department’s 3D printing facility that was used to produce prototypes of the device used in the study. We thank the subjects for participating in the study and the UCSB Human Subjects Committee for approving the study. Finally, we thank the UCSB Physics Department for providing infrastructure for conducting the study.
Author information
Authors and Affiliations
Contributions
S.S. wrote the manuscript, contributed to developing the study protocol and writing human subject committee proposal, built the device used in the study, conducted data analysis and produced the figures; D.A. contributed to developing the study protocol and writing human subject committee proposal, and worked on subject recruitment; P.H. was a faculty advisor who contributed to device design, experimental procedure, data analysis and helped editing manuscript and figures.
Corresponding author
Ethics declarations
Conflict of Interest
The authors of this paper report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sokolovskiy, S., Arroyo, D. & Hansma, P. Can Pulse Rate Variability be Used to Monitor Compliance with a Breath Pacer?. Appl Psychophysiol Biofeedback (2024). https://doi.org/10.1007/s10484-023-09617-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s10484-023-09617-y