Abstract
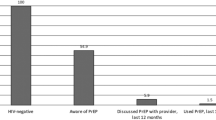
We examined PrEP awareness and use among people who inject drugs (PWID) in San Francisco in 2018. Of 397 respondents not known to be HIV positive, 56.7% had heard of PrEP, 38.9% knew that PrEP can prevent HIV transmission from sharing injection equipment, 13.6% had discussed PrEP with a health care provider, and 3.0% had used PrEP in the last 12 months. All seven male PWID who had used PrEP were also men who had sex with men. There is urgent need to improve messaging on PrEP’s effectiveness for PWID and to tailor ways of engaging PWID in PrEP programs.

Similar content being viewed by others
References
Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019. https://doi.org/10.1001/jama.2019.1343.
Raymond HF, Snowden JM, Guigayoma J, McFarland W, Chen YH. Community levels of PrEP use among men who have sex with men by race/ethnicity, San Francisco, 2017. AIDS Behav. 2019. https://doi.org/10.1007/s10461-019-02428-5.
San Francisco Department of Public Health. HIV Epidemiology Annual Report 2017. https://www.sfdph.org/dph/files/reports/RptsHIVAIDS/AnnualReport2017-Green-20180904-Web.pdf. Accessed on 13 Sept 2018.
Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90. https://doi.org/10.1016/S0140-6736(13)61127-7.
Centers for Disease Control and Prevention. HIV infection, risk, prevention, and testing behaviors among persons who inject drugs—National HIV Behavioral Surveillance: Injection Drug Use, 20 U.S. Cities, 2015. HIV Surveillance Special Report 18. Revised edition. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2018. Accessed 21 Aug 2019.
Roth A, Tran N, Piecara B, Welles S, Shinefeld J, Brady K. Factors associated with awareness of pre-exposure prophylaxis for HIV among persons who inject drugs in Philadelphia: National HIV Behavioral Surveillance, 2015. AIDS Behav. 2019;23(7):1833–40.
Sherman SG, Schneider KE, Park JN, et al. PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug Alcohol Depend. 2019;195:148–55.
Bazzi AR, Biancarelli DL, Childs E, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDS. 2018;32(12):529–37.
Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025–33.
US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed 30 May 2019.
Strathdee SA, Shoptaw S, Dyer TP, Quan VM, Aramrattana A. Substance use scientific committee of the HIV prevention trials network. Towards combination HIV prevention for injection drug users: addressing addictophobia, apathy and inattention. Curr Opin HIV AIDS. 2012;7(4):320–5.
Li J, Valente TW, Shin HS, et al. Overlooked threats to respondent driven sampling estimators: peer recruitment reality, degree measures, and random selection assumption. AIDS Behav. 2018;22(7):2340–59. https://doi.org/10.1007/s10461-017-1827-1.
Acknowledgements
This research was supported by the US Centers for Disease Control and Prevention (CDC) (6NU62PS005077).
Funding
This research was supported by the US Centers for Disease Control and Prevention (1U1BPS003247, 5U1BPS003247, and 6NU62PS005077).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical Approval
The study was reviewed and approved by the Institutional Review Board of the University of California San Francisco. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McFarland, W., Lin, J., Santos, GM. et al. Low PrEP Awareness and Use Among People Who Inject Drugs, San Francisco, 2018. AIDS Behav 24, 1290–1293 (2020). https://doi.org/10.1007/s10461-019-02682-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02682-7