Abstract
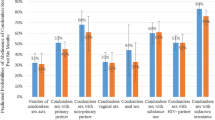
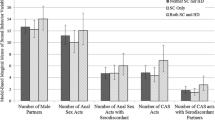
Heterosexual anal intercourse (HAI) is an understudied risk behavior among women and men in substance abuse treatment. Rates of HAI for women (n = 441) and men (n = 539) were identified for any, main and casual partners. More men (32.8 %) than women (27.1 %) reported engaging in HAI in the previous 90 days. These rates are higher than those reported for both men (6.0–15.9 %) and women (3.5–13.0 %) ages 25–59 in the National Survey of Sexual Health and Behavior. Men were significantly more likely to report HAI with their casual partners (34.1 %) than women (16.7 %). In a logistic regression model generated to identify associations between HAI and variables previously shown to be related to high risk sexual behavior, being younger, bisexual, and White were significantly associated with HAI. For men, having more sex partners was also a significant correlate. HAI is a logical target for increased focus in HIV prevention interventions.
Resumen
El sexo anal heterosexual (SAH) no se ha estudiado bastante como una conducta de riesgo en mujeres y hombres en tratamiento de abuso de sustancia. Las tasas de SAH para mujeres (n = 441) y hombres (n = 539) fueron identificadas para parejas principales, casuales o cualquier otra pareja. Más hombres (32.8 %) que mujeres (27.1 %) reportearon haberse involucrado en SAH durante los 90 días anteriores. Estas tasas son más altas que las reporteadas para hombres (6.0–15.9 %) y mujeres (3.5–13.0 %) de 25–29 años en la National Survey of Sexual Health and Behavior (Encuesta Nacional de Salud y Conducta Sexuales). Los hombres fueron significativamente más propensos a reportear SAH con sus parejas casuales (34.1 %) que las mujeres (16.7 %). En un modelo de regresión logística diseñado para identificar las asociaciones entre SAH y variables anteriormente mostradas a ser relacionadas con conductas sexuales de alto riesgo, ser más joven, bisexual, y caucásico se asoció significativamente con SAH. Para los hombres, tener más parejas sexuales fue también un correlato significativo. SAH es un objetivo lógico para mayor enfoque en las intervenciones de prevención de VIH.
Similar content being viewed by others
References
Center for Disease Control and Prevention: Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 2009. February 2011 http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Accessed 22 May 2012.
Calsyn DA, Hatch-Maillette M, Tross S, Doyle SR, Crits-Christoph P, Song YS. Motivational and skills training HIV/sexually transmitted infection sexual risk reduction groups for men. J Subst Abuse Treat. 2009;37(2):138–50.
Tross S, Campbell ANC, Cohen LR, Calsyn D, Pavlicova M, Miele GM, et al. Effectiveness of HIV/STD sexual risk reduction groups for women in substance abuse treatment programs: results of nida clinical trials network trial. J Acquir Immune Defic Syndr. 2008;48:581–9.
Kalichman SC, Cherry C, Browne-Sperling F. Effectiveness of a video-based motivational skills-building HIV risk-reduction intervention for inner-city African American men. J Consult Clin Psychol. 1999;67:959–66.
Pyeatt M, Tirado A. Nia facilitator’s Guide. Dallas: University of Texas Southwestern; 2008.
Villarruel AM, Jemmott JB, Jemmott LS. A randomized controlled trial testing an HIV prevention intervention for latino youth. Arch Pediatric Adolesc Med. 2006;160:1–6.
Boily MC, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta analysis of observational studies. Lancet Infect Dis. 2009;9:118–29.
Halperin D. Heterosexual anal intercourse: prevalence, cultural factors, and HIV infection and other health risks, part I. AIDS Patient Care and STDs. 1999;13:717–30.
Mastro TD, Kitayaporn D. HIV type 1 transmission probabilities: estimates from epidemiological studies. AIDS Res Hum Retroviruses. 1998;14:S223–7.
Powis B, Griffiths P, Gossop M, Strang J. Heterosexual anal intercourse, health risks and drug use: a review with special attention to drug users. Drug Alcohol Rev. 1995;14:223–9.
Voellner B. AIDS and heterosexual anal intercourse. Arch Sex Behav. 1991;20:233–76.
Padian N, Shiboski S, Jewell N. The effect of number of exposures on the risk of heterosexual HIV transmission. J Infect Dis. 1990;161(5):883–7.
Risser JMH, Padgett P, Wolverton M, Risser WL. Relationship between heterosexual anal sex, injection drug use and HIV infection among black men and women. Int J STD AIDS. 2009;20:310–4.
Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, et al. Efficacy of an HIV/STI prevention intervention for black men who have sex with men: findings from the many men, many voices (3MV) project. AIDS Behav. 2009;13:532–44.
Jones KT, Gray P, Whiteside YO, Wang T, Bost D, Dunbar E, et al. Evaluation of an HIV preventinon intervention adapted for black men who have sex with men. Am J Public Health. 2008;98:1043–60.
Erickson P, Bastani R, Maxwell AE, Marcus AC, Capell FJ, Yan KX. Prevalence of anal sex among heterosexuals in California and its relationship to other AIDS risk behaviors. AIDS Educ Prev. 1995;7(6):477–93.
Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behaviors, relationships, and perceived health status among adult women in the United States: Results from a national probability sample. J Sexual Med. 2010;7(Suppl 5):277–90.
Reece M, Herbenick D, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behaviors, relationships, and perceived health among adult men in the United States: results from a national probability sample. J Sexual Med. 2010;7(Suppl 5):291–304.
Tian LH, Peterman TA, Tao G, Brooks LC, Metcalf C, Malotte CK, et al. Heterosexual anal sex activity in the year after an STD clinic visit. Sex Transm Dis. 2008;35(11):905–9.
Reynolds GL, Fisher DG, Napper LE, Fremming BW, Jansen MA. Heterosexual anal sex reported by women receiving HIV prevention services in Los Angeles county. Women’s Health Issues. 2010;20(6):414–9.
Zule WE, Costenbader EC, Meyer WJ Jr, Wechsberg WM. Methamphetamine use and risky sexual behaviors during heterosexual encounters. Sex Transm Dis. 2007;34(9):689–94.
Center for Disease Control and Prevention. Methamphetamine use and HIV risk behaviors among heterosexual men-preliminary results from five northern California counties, december 2001–november 2003. MMWR. 2006;55(10):273–7.
Bogart LM, Kral AH, Scott A, Anderson R, Flynn N, Gilbert ML, et al. Sexual risk among injection drug users recruited from syringe exchange programs in California. Sex Transm Dis. 2005;32(1):27–34.
Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. The Western J Med. 1998;168:93–7.
Baldwin J, Baldwin J. Heterosexual anal intercourse: an understudied, high-risk sexual behavior. Arch Sex Behav. 2000;29:357–73.
Seidlin M, Vogler M, Lee E, Lee YS, Dubin N. Heterosexual transmission of HIV in a cohort of couples in New York City. AIDS. 1993;7:1247–54.
Leichliter JS. Heterosexual anal sex: part of an expanding sexual repertoire. Sex Transm Dis. 2008;35(11):910–1.
Padian N, Shiboski S, Glass S, Vittinghoff E. Heterosexual transmission of human immunodeficiency virus (HIV) in northern California: results from a ten-year study. Am J Epidemiol. 1997;168(4):350–7.
Pendergrast ML, Urada D, Podus D. Meta-analysis of HIV risk-reduction interventions within drug abuse treatment programs. J Consult Clin Psychol. 2001;69(3):389–405.
Davis W, Johnson B, Randolph D, Liberty H. Risks for HIV infection among users and sellers of crack, powder cocaine and heroin in central Harlem: implications for interventions. AIDS Care. 2006;18(2):158–65.
Strathdee S, Sherman S. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(4 (suppl 3)):iii7–14.
Buchacz K, van der Straten A, Shiboski S, Gomez C, Padian N. Sociodeographic, behavioral, and clinical correlates of inconsistent condom use in HIV-serodiscordant heterosexual couples. J Acquir Immune Defic Syndr. 2001;28(3):289–97.
Raj A, Saitz R, Cheng D, Winter M, Samet J. Associations between alcohol, heroin, and cocaine use and high risk sexual behaviors among detoxification patients. Am J Drug Alcohol Abuse. 2007;33:169–78.
Meade CS, Sikkema KJ. HIV risk behavior among adults with severe mental illness: a systematic review. Clin Psychol Rev. 2005;25:433–57.
Meade C. Sexual risk behavior among persons dually diagnosed with severe mental illness and substance use disorder. J Subst Abuse Treat. 2006;30:147–57.
Meade CS, Sikkema KJ. Psychiatric and psychosocial correlates of sexual risk behavior among adults with severe mental illness. Community Ment Health J. 2007;43(2):153–69.
Cockrell JR, Folstein MF. Mini-mental state examination (mmse). Psychopharmacol Bull. 1988;24(4):689–92.
Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:196–8.
Calsyn DA, Wells EA, Saxon AJ, Jackson R, Heiman JR. Sexual activity under the influence of drugs is common among methadone clients. Rockville : National Institute on Drug Abuse, 2000 Contract No.: 00-4773.
Meyer-Bahlburg H, Ehrhardt A, Exner TM, Gruen RS. Sexual risk behavior assessment schedule-adult-armory interview. New York: New York State Psychiatric Institute and Columbia University; 1991.
Sohler N, Colson PW, Meyer-Bahlburg HFL, Susser E. Reliability of self reports about sexual risk behaviors for HIV among homeless men with severe mental illness. Psychiatric Services. 2000;51:814–6.
Gross M, Holte SE, Marmor M, Mwatha A, Koblin BA, Mayer KM. Anal sex among HIV-seronegative women at high risk of HIV exposure. J Acquir Immune Defic Syndr. 2000;24:393–8.
Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET vaccine preparedness study protocol team. Am J Epidemiol. 2000;152(2):99–106.
Bruning J, Kintz B. Computational Handbook of Statistics. 3rd ed. Glenview: Scott Foresman; 1987.
Howard D, Latkin C. A bridge over troubled waters: factors associated with non-injection drug users having injection drug using sex partners. J Acquir Immune Defic Syndr. 2006;43:325–30.
PASW Statistics. Release 18. ed. Chicago, IL: IBM Corporation. 2009.
Cheng WS, Garfein RS, Semple SJ, Strathdee SA, Zians JK, Patterson TL. Methamphetamine users binge use and sex and drug use behaviors among HIV(−), heterosexual methamphetamine users in San Diego. Subst Use Misuse. 2010;45:116–33.
Calsyn D, Berns S, Hatch-Maillette MA, Tross S. Real Men Are Safe (REMAS): A Gender-Focused HIV and Sexual Risk Reduction Intervention for Men in Substance Abuse Treatment. Seattle, WA: CTN Dissemination Library; 2009. Available from: http://ctndisseminationlibrary.org/display/397.htm.
Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994;62:385–97.
Acknowledgments
The study was supported by National Institute on Drug Abuse (NIDA) Clinical Trials Network (CTN). Grants:U10 DA13714 (D. Donovan, PI), U10 DA 13035 (Edward Nunes and John Rotrosen, Co-PIs), U10 DA 013727 (Kathleen Brady, PI), and K23 DA028660 (Christina Meade, PI). The authors wish to thank Paul Crits-Christoph, Ph.D., University of Pennsylvania and Robert Gallop, Ph.D., West Chester University, for their assistance in combining the datasets from CTN protocol 0018 and CTN protocol 0019.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calsyn, D.A., Hatch-Maillette, M.A., Meade, C.S. et al. Gender Differences in Heterosexual Anal Sex Practices Among Women and Men in Substance Abuse Treatment. AIDS Behav 17, 2450–2458 (2013). https://doi.org/10.1007/s10461-012-0387-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0387-7