Abstract
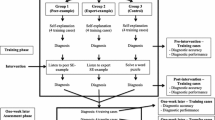
Self-explanation while diagnosing clinical cases fosters medical students’ diagnostic performance. In previous studies on self-explanation, students were free to self-explain any aspect of the case, and mostly clinical knowledge was used. Elaboration on knowledge of pathophysiological mechanisms of diseases has been largely unexplored in studies of strategies for teaching clinical reasoning. The purpose of this two-phase experiment was to investigate the effect of self-explanation of pathophysiology during practice with clinical cases on students’ diagnostic performance. In the training phase, 39 4th-year medical students were randomly assigned to solve 6 criterion cases (3 of jaundice; 3 of chest pain), either self-explaining the pathophysiological mechanisms of the findings (n = 20) or without self-explaining (n = 19). One-week later, in the assessment phase, all students solved 6 new cases of the same syndromes. A repeated-measures analysis of variance on the mean diagnostic accuracy scores showed no significant main effects of study phase (p = 0.34) and experimental condition (p = 0.10) and no interaction effect (p = 0.42). A post hoc analysis found a significant interaction (p = 0.022) between study phase and syndrome type. Despite equal familiarity with jaundice and chest pain, the performance of the self-explanation group (but not of the non-self-explanation group) on jaundice cases significantly improved between training and assessment phases (p = 0.035) whereas no differences between phases emerged on chest pain cases. Self-explanation of pathophysiology did not improve students’ diagnostic performance for all diseases. Apparently, the positive effect of this form of self-explanation on performance depends on the studied diseases sharing similar pathophysiological mechanisms, such as in the jaundice cases.


Similar content being viewed by others
Change history
21 February 2017
An erratum to this article has been published.
References
Boshuizen, H. P., & Schmidt, H. G. (1992). On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novice. Cognitive Science, 16, 153–184.
Bruin, A. B., Rikers, R. M., & Schmidt, H. G. (2007). The effect of self-explanation and prediction on the development of principled understanding of chess in novices. Contemporary Educational Psychology, 32(2), 188–205. doi:10.1016/j.cedpsych.2006.01.001.
Calin-Jageman, R. J., & Ratner, H. H. (2005). The role of encoding in the self-explanation effect. Cognition and Instruction, 23(4), 523–543.
Chamberland, M., Mamede, S., St-Onge, C., Rivard, M.-A., Setrakian, J., Lévesque, A., et al. (2013). Students’ self-explanations while solving unfamiliar cases: The role of biomedical knowledge. Medical Education, 47, 1109–1116. doi:10.1111/medu.12253.
Chamberland, M., Mamede, S., St-Onge, C., Setrakian, J., Bergeron, L., & Schmidt, H. (2015). Self-explanation in learning clinical reasoning: The added value of examples and prompts. Medical Education, 49, 193–202. doi:10.1111/medu.12623.
Chamberland, M., Mamede, S., St-Onge, C., Setrakian, J., & Schmidt, H. (2014). Does medical students’ diagnostic performance improve by observing examples of self-explanation provided by peers or experts? Advances in Health Sciences Education. doi:10.1007/s10459-014-9576-7. (Epub ahead of print).
Chamberland, M., St-Onge, C., Setrakian, J., Lanthier, L., Bergeron, L., Bourget, A., et al. (2011). The influence of medical students’ self-explanations on diagnostic performance. Medical Education, 45, 688–695. doi:10.1111/j.1365-2923.2011.03933.x.
Charlin, B., Boshuizen, H. P., Custers, E. J., & Feltovich, P. J. (2007). Scripts and clinical reasoning. Medical Education, 41, 1178–1184. doi:10.1111/j.1365-2923.2007.02924.x.
Chi, M. T., Bassok, M., Lewis, M. W., Reimann, P., & Glaser, R. (1989). Self-explanations: How students study and use examples in learning to solve problems. Cognitive Science, 13, 145–182.
Chi, M. T., Leeuw, N. D., Chiu, M.-H., & LaVancher, C. (1994). Eliciting self-explanations improves understanding. Cognitive Science, 18, 439–477.
Chi, M. T., & Slotta, J. D. (1993). The ontological coherence of intuitive physics. Cognition and Instruction, 10(2–3), 249–260. doi:10.1080/07370008.1985.9649011.
Chi, M. T., & VanLehn, K. A. (1991). The content of physics self-explanations. The Journal of the Learning Sciences, 1(1), 69–105.
Dunlosky, J., Rawson, K. A., Marsh, E. J., Nathan, M. J., & Willingham, D. T. (2013). Improving students’ learning with effective learning techniques: Promising directions from cognitive and educational psychology. Psychological Science in the Public Interest, 14(1), 4–58. doi:10.1177/1529100612453266.
Eva, K. W. (2004). What every teacher needs to know about clinical reasoning. Medical Education, 39, 98–106. doi:10.1111/j.1365-2929.2004.01972.x.
Heitzmann, N., Fischer, F., Kuhne-Eversmann, L., & Fischer, M. R. (2015). Enhancing diagnostic competence with self-explanation prompts and adaptable feedback. Medical Education, 49, 993–1003. doi:10.1111/medu.12778.
Ibiapina, C., Mamed, S., Moura, A., Elói-Santos, S., & Gog, T. V. (2014). Effects of free, cued and modelled reflection on medical students’ diagnostic competence. Medical Education, 48, 796–805. doi:10.1111/medu.12435.
Kassirer, J. P. (2010). Teaching clinical reasoning: Case-based and coached. Academic Medicine, 85(7), 1118–1124.
Larsen, D. P., Butler, A. C., & Roediger, H. L., III. (2013). Comparative effects of test-enhanced learning and self-explanation on long-term retention. Medical Education, 47, 674–682. doi:10.1111/medu.12141.
Lee, A., Joynt, G. M., Lee, A. K., Ho, A. M., Groves, M., Vlantis, A. C., et al. (2010). Using illness scripts to teach clinical reasoning skills to medical students. Family Medicine, 42(4), 255–261.
Leppink, J., Broers, N., Imbos, T., Vleuten, C. V., & Berger, M. P. (2012). Self-explanation in the domain of statistics: An expertise reversal effect. Higher Education, 63, 771–785. doi:10.1007/s10734-011-9476-1.
Mamede, S., van Gog, T., Moura, A. S., Faria, R. M., Peixoto, J. M., Rikers, R. M., et al. (2012). Reflection as a strategy to foster medical students’ acquisition of diagnostic competence. Medical Education, 46, 464–472. doi:10.1111/j.1365-2923.2012.04217.x.
Mamede, S., van Gog, T., Moura, A. S., Faria, R. M., Peixoto, J. M., & Schmidt, H. G. (2014). How can students’ diagnostic competence benefit most from practice with clinical cases? The effects of structured reflection on future diagnosis of the same and novel diseases. Academic Medicine, 89(1), 121–127. doi:10.1097/ACM.0000000000000076.
Norman, G. (2005). Research in clinical reasoning: Past history and current trends. Medical Education, 39, 418–427. doi:10.1111/j.1365-2929.2005.02127.x.
Norman, G., Young, M., & Brooks, L. (2007). Non-analytical models of clinical reasoning: The role of experience. Medical Education, 41(12), 1140–1145. doi:10.1111/j.1365-2923.2007.02914.x.
Papa, F. J., Shores, J. H., & Meyer, S. (1990). Effects of pattern matching, patter discrimination, and experience in the development of diagnostic expertise. Academic Medicine, 65(9), S21–S22.
Patel, V. L., Yoskowitz, N. A., Arocha, J. F., & Shortliffe, E. H. (2009). Cognitive and learning sciences in biomedical and health instructional design: A review with lessons for biomedical informatics education. Journal of Biomedical Informatics, 42, 176–197. doi:10.1016/j.jbi.2008.12.002.
Roy, M., & Chi, M. (2005). The self-explanation principle in multimedia learning. In R. E. Mayer (Ed.), The Cambridge handbook of multimedia learning (pp. 271–286). New York: Cambridge University Press.
Schmidt, H. G., & Boshuizen, H. P. (1993). On acquiring expertise in medicine. Educational Psychology Review, 5(3), 205–221. doi:10.1007/BF01323044.
Schmidt, H. G., Norman, G. R., & Boshuizen, H. A. (1990). A cognitive perspective on medical expertise: Theory and implications. Academic Medicine, 65(10), 611–621.
Schmidt, H. G., & Rikers, R. J. (2007). How expertise develops in medicine: Knowledge encapsulation and illness sripts formation. Medical Education, 41, 1133–1139. doi:10.1111/j.1365-2923.2007.02915x.
VanLehn, K. & Jones, R. M. (1993). What mediates the self-explanation effect? Knowledge gaps, schemas or analogies? In M. Polson (Ed.), Proceedings of the Fifteenth Annual Conference of the Cognitive Science Society (pp. 1034–1039). Hillsdale: Lawrence Erlbaum Associates.
Verkoeijen, P. P. J. L., Rikers, R. M .J .P., Schmidt, H. G., van de Wiel, M. W. J., & Kooman, J. P. (2004). Case representation by medical experts, intermediates and novices for laboratory data presented with or without a clinical context. Medical Education, 38, 617–627. doi:10.1046/j.1365-2923.2004.01797.x.
Woods, N. (2007). Science is fundamental: The role of biomedical knowledge in clinical reasoning. Medical Education, 41(12), 1173–1177. doi:10.1111/j.1365-2923.2007.02911.x.
Woods, N. N., Brooks, L. R., & Norman, G. R. (2005). The value of basic science in clinical diagnosis: Creating coherence among signs and symptoms. Medical Education, 39, 107–112. doi:10.1111/j.1365-2929.2004.02036.x.
Acknowledgements
The authors are grateful to the students who dedicated their time to participate in the study. The authors would like to thank Albert Nilo, Bruna Costa Carvalho França, Eliane Perlatto de Moura, Fabiano Gonçalves Guimarães, Flávio Chaimowicz, Josemar de Almeida Moura, Lígia Maria Cayres Ribeiro, Paulo Henrique Boy Torres for their assistance with data collection.
Funding
During the realisation of the study, José Maria Peixoto was supported by a scholarship provided by the CAPES Foundation, Ministry of Education of Brazil, Brasilia/DF (Process No. 9460/14-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
The original version of this article was revised: The name of author Alexandre Sampaio Moura was incorrectly captured as Alexandre Sampaio de Moura. It has been corrected here.
An erratum to this article is available at https://doi.org/10.1007/s10459-017-9764-3.
Appendices
Appendix 1: Case diagnoses used in different phase of the study
Training phase | Assessment phase |
|---|---|
Jaundice | |
Acute vital hepatitis | Acute vital hepatitis |
Haemolysis | Haemolysis |
Colelithiasis | Colelithiasis |
Pancreas tumor | |
Chest pain | |
Myocardial infarction | Myocardial infarction |
Aortic dissection | Aortic dissection |
Gastroesophageal reflux | Gastroesophageal reflux |
Pericarditis | |
Fillers | |
Pyelonephritis | Infectious mononucleosis |
Pneumonia | Meningitis |
Appendix 2: Example of a case used in the study
The patient was a 50-year-old female, married, lawyer, borned in São José de Almeida-MG and living in Belo Horizonte. She had one birth, one child and no abortion. She complains a severe abdominal colic pain located in the right upper quadrant and radiating to back. The pain started two weeks ago. She has made use of antispasmodic medication with partial improvement. Ten days ago she begans jaundice, dark urine, fecal hipocolia and itching. She denies nausea or vomiting. Reports loss weight (3 kg) in the last 3 months. She is social drinker: 2 cans of beer per week for 10 years. She denies smoking and previous surgeries. On physical examination the patient presented jaundice (3+/4), in a good general condition, mucous stained and hydrated, without edema. Her BMI was 28, temperature 37.3 °C, blood pressure 110/80 mmHg; pulse 78 bpm and respiratory rate 18/min. Cardiovascular system: good peripheral perfusion with large and full arterial pulses, regular heart rhythm times, without murmurs. Respiratory system: Normal expandability, physiological vesicular murmur, with no signs of breathing. Abdomen: peristaltic, flaccid, positive Murphy sign without pasta or visceromegaly.
Lab tests results | Reference values | Lab tests results | Reference values |
|---|---|---|---|
Hemoglobin: 14.8 g/dl | 12.0–16.0 g/dL | AST: 90 U/L | 15–40 U/L |
MCV: 88 Fl | 80–100 Fl | ALT: 70 U/L | 5–35 U/L |
MCH: 28 pg | 26–34 pg | Alkaline phosphatase: 740 U/L | 40–130 U/L |
Leukocytes: 8800/µL | 4000–11,000/µL | Gamma GT: 277 U/L | 10–49 U/L |
Neutrophilis: 77% | 45–75% | Total bilirubin: 18.2 mg/dL | 0.20–1.00 mg/dL |
Lymphocytes: 23% | 22–40% | Direct bilirubin: 13.4 mg/dL | 0.00–0.20 mg/dL |
Platelets: 344.000/µL | 150.000–450.000/µL | Indirect bilirubin: 4.8 mg/dL | 0.20–0.80 mg/dL |
Reticulocytes: 1% | 0.5–1.5% |
Rights and permissions
About this article
Cite this article
Peixoto, J.M., Mamede, S., de Faria, R.M.D. et al. The effect of self-explanation of pathophysiological mechanisms of diseases on medical students’ diagnostic performance. Adv in Health Sci Educ 22, 1183–1197 (2017). https://doi.org/10.1007/s10459-017-9757-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-017-9757-2