Abstract
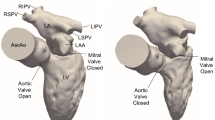
The immersed boundary (IB) method is a mathematical framework for fluid–structure interaction problems (FSI) that was originally developed to simulate flows around heart valves. Direct comparison of FSI simulations around heart valves against experimental data is challenging, however, due to the difficulty of performing robust and effective simulations, the complications of modeling a specific physical experiment, and the need to acquire experimental data that is directly comparable to simulation data. Such comparators are a necessary precursor for further formal validation studies of FSI simulations involving heart valves. In this work, we performed physical experiments of flow through a pulmonary valve in an in vitro pulse duplicator, and measured the corresponding velocity field using 4D flow MRI (4-dimensional flow magnetic resonance imaging). We constructed a computer model of this pulmonary artery setup, including modeling valve geometry and material properties via a technique called design-based elasticity, and simulated flow through it with the IB method. The simulated flow fields showed excellent qualitative agreement with experiments, excellent agreement on integral metrics, and reasonable relative error in the entire flow domain and on slices of interest. These results illustrate how to construct a computational model of a physical experiment for use as a comparator.









Similar content being viewed by others
References
Astorino, M., J. F. Gerbeau, O. Pantz, and K.-F. Traore. Fluid-structure interaction and multi-body contact: application to aortic valves. Comput. Methods Appl. Mech. Eng. 198(45–46):3603–3612, 2009.
Banko, A. J., F. Coletti, C. J. Elkins, and J. K. Eaton. Oscillatory flow in the human airways from the mouth through several bronchial generations. Int. J. Heat Fluid Flow. 61:45–57, 2016.
Banko, A. J., F. Coletti, D. Schiavazzi, C. J. Elkins, and J. K. Eaton. Three-dimensional inspiratory flow in the upper and central human airways. Exp. Fluids. 56(6):117, 2015.
Bao, Y., A. D. Kaiser, J. Kaye, and C. S. Peskin. Gaussian-like immersed boundary kernels with three continuous derivatives and improved translational invariance. http://arxiv.org/abs/1505.07529v3(2017).
Bertoglio, C., A. Caiazzo, Y. Bazilevs, M. Braack, M. Esmaily, V. Gravemeier, A. Marsden, O. Pironneau, I. E. Vignon-Clementel, and W. A. Wall. Benchmark problems for numerical treatment of backflow at open boundaries. Int. J. Numer. Methods Biomed. Eng. 34:e2918, 2017.
Billiar, K. L., and M. S. Sacks. Biaxial mechanical properties of the native and glutaraldehyde-treated aortic valve cusp: part II-a structural constitutive model. J. Biomech. Eng. 122(4):327–335, 2000.
Elkins, C. J., and M. T. Alley. Magnetic resonance velocimetry: applications of magnetic resonance imaging in the measurement of fluid motion. Exp. Fluids. 43(6):823–858, 2007.
Elkins, C. J., M. Markl, N. Pelc, and J. K. Eaton. 4D Magnetic resonance velocimetry for mean velocity measurements in complex turbulent flows. Exp. Fluids. 34(4):494–503, 2003.
Emendi, M., F. Sturla, R. P. Ghosh, M. Bianchi, F. Piatti, F. R. Pluchinotta, D. Giese, M. Lombardi, A. Redaelli, and D. Bluestein. Patient-specific bicuspid aortic valve biomechanics: a magnetic resonance imaging integrated fluid-structure interaction approach. Ann. Biomed. Eng. 49(2):627–641, 2021.
Gao, H., L. Feng, X. Luo, N. Qi, W. Sun, M. Vazquez, and B. E. Griffith. On the chordae structure and dynamic behaviour of the mitral valve. IMA J. Appl. Math. 83(6):1066–1091, 2018.
Griffith, B. E. Immersed boundary model of aortic heart valve dynamics with physiological driving and loading conditions. Int. J. Numer. Methods Biomed. Eng. 28(3):317–345, 2012.
Griffith, B. E. IBAMR: Immersed boundary adaptive mesh refinement, Accessed 2021. https://github.com/IBAMR/IBAMR.
Griffith, B. E., R. D. Hornung, D. M. McQueen, and C. S. Peskin. Parallel and Adaptive Simulation of Cardiac Fluid Dynamics. Advanced Computational Infrastructures for Parallel and Distributed Adaptive Applications. Hoboken: Wiley, p. 105, 2010.
Hsu, M. C., D. Kamensky, F. Xu, J. Kiendl, C. Wang, M. C. Wu, J. Mineroff, A. Reali, Y. Bazilevs, and M. S. Sacks. Dynamic and fluid-structure interaction simulations of bioprosthetic heart valves using parametric design with t-splines and fung-type material models. Comput. Mech. 55(6):1211–1225, 2015.
Kaiser, A. D. Modeling the mitral valve. Ph.D. thesis, Courant Institute of Mathematical Sciences, New York University (2017).
Kaiser, A. D., D. M. McQueen, and C. S. Peskin. Modeling the mitral valve. Int. J. Numer. Methods Biomed. Eng. 35(11):e3240, 2019.
Kaiser, A. D., R. Shad, W. Hiesinger, and A. L. Marsden. A design-based model of the aortic valve for fluid-structure interaction. Biomech. Model. Mechanobiol. 20(6):2413–2435, 2021.
Kaiser, A. D., R. Shad, N. Schiavone, W. Hiesinger, and A. L. Marsden. Controlled comparison of simulated hemodynamics across tricuspid and bicuspid aortic valves. Ann. Biomed. Eng. 50(9):1053–1072, 2022.
Kalejs, M., P. Stradins, R. Lacis, I. Ozolanta, J. Pavars, and V. Kasyanov. St Jude epic heart valve bioprostheses versus native human and porcine aortic valves-comparison of mechanical properties. Interact. Cardiovasc. Thorac. Surg. 8(5):553–556, 2009.
Kheradvar, A., E. M. Groves, A. Falahatpisheh, M. K. Mofrad, S. H. Alavi, R. Tranquillo, L. P. Dasi, C. A. Simmons, K. J. Grande-Allen, C. J. Goergen, et al. Emerging trends in heart valve engineering: Part IV. Computational modeling and experimental studies. Ann. Biomed. Eng. 43(10):2314–2333, 2015.
Kim, Y., and C. S. Peskin. Penalty immersed boundary method for an elastic boundary with mass. Phys. Fluids. 19(5):053103, 2007.
Lai, M. C., and C. S. Peskin. An immersed boundary method with formal second-order accuracy and reduced numerical viscosity. J. Comput. Phys. 160(2):705–719, 2000.
Lee, J. H., A. D. Rygg, E. M. Kolahdouz, S. Rossi, S. M. Retta, N. Duraiswamy, L. N. Scotten, B. A. Craven, and B. E. Griffith. Fluid-structure interaction models of bioprosthetic heart valve dynamics in an experimental pulse duplicator. Ann. Biomed. Eng. 48(5):1475–1490, 2020.
Lee, J. H., L. N. Scotten, R. Hunt, T. G. Caranasos, J. P. Vavalle, and B. E. Griffith. Bioprosthetic aortic valve diameter and thickness are directly related to leaflet fluttering: results from a combined experimental and computational modeling study. JTCVS Open. 6:60–81, 2021.
Lim, S., A. Ferent, X. Wang, and C. Peskin. Dynamics of a closed rod with twist and bend in fluid. SIAM J. Sci. Comput. 31(1):273–302, 2008.
Ma, X., H. Gao, B. E. Griffith, C. Berry, and X. Luo. Image-based fluid-structure interaction model of the human mitral valve. Comput. Fluids. 71:417–425, 2013.
Mao, W., A. Caballero, R. McKay, C. Primiano, and W. Sun. Fully-coupled fluid-structure interaction simulation of the aortic and mitral valves in a realistic 3d left ventricle model. PLoS ONE. 12:e0184729, 2017.
Markl, M., F. P. Chan, M. T. Alley, K. L. Wedding, M. T. Draney, C. J. Elkins, D. W. Parker, R. Wicker, C. A. Taylor, R. J. Herfkens, and N. J. Pelc. Time-resolved three-dimensional phase-contrast MRI. J. Magn. Reson. Imaging. 17(4):499–506, 2003.
May-Newman, K., C. Lam, and F. C. Yin. A hyperelastic constitutive law for aortic valve tissue. J. Biomech. Eng. 131:8, 2009.
McQueen, D., T. O’Donnell, B. Griffith, and C. Peskin. Constructing a Patient-Specific Model Heart from CT Data. Handbook of Biomedical Imaging. New York: Springer, pp. 183–197, 2015.
McQueen, D. M., and C. S. Peskin. Heart Simulation by an Immersed Boundary Method with Formal Second-Order Accuracy and Reduced Numerical Viscosity. Mechanics for a New Mellennium. New York: Springer, pp. 429–444, 2001.
Pelc, N. J., R. J. Herfkens, A. Shimakawa, and D. R. Enzmann. Phase contrast cine magnetic resonance imaging. Magn. Reson. Q. 7(4):229–254, 1991.
Pelc, N. J., F. G. Sommer, K. C. Li, T. J. Brosnan, R. J. Herfkens, and D. R. Enzmann. Quantitative magnetic resonance flow imaging. Magn. Reson. Q. 10(3):125–147, 1994.
Peskin, C. S. Flow patterns around heart valves: a numerical method. J. Comput. Phys. 10(2):252–271, 1972.
Peskin, C. S. The immersed boundary method. Acta Numer. 11:479–517, 2002.
Rousseau, E., A. Sauren, M. Van Hout, and A. Van Steenhoven. Elastic and viscoelastic material behaviour of fresh and glutaraldehyde-treated porcine aortic valve tissue. J. Biomech. 16(5):339–348, 1983.
Sahasakul, Y., W. D. Edwards, J. M. Naessens, and A. J. Tajik. Age-related changes in aortic and mitral valve thickness: implications for two-dimensional echocardiography based on an autopsy study of 200 normal human hearts. Am. J. Cardiol. 62(7):424–430, 1988.
Sauren, A., W. Kuijpers, A. van Steenhoven, and F. Veldpaus. Aortic valve histology and its relation with mechanics: preliminary report. J. Biomech. 13(2):97–104, 1980.
Schiavone, N. K., C. J. Elkins, D. B. McElhinney, J. K. Eaton, and A. L. Marsden. In vitro assessment of right ventricular outflow tract anatomy and valve orientation effects on bioprosthetic pulmonary valve hemodynamics. Cardiovasc. Eng. Technol. 2021:1–17, 2021.
Shadden, S. C., M. Astorino, and J. F. Gerbeau. Computational analysis of an aortic valve jet with Lagrangian coherent structures. Chaos. 20(1):017512, 2010.
Sigüenza, J., D. Pott, S. Mendez, S. J. Sonntag, T. A. Kaufmann, U. Steinseifer, and F. Nicoud. Fluid-structure interaction of a pulsatile flow with an aortic valve model: a combined experimental and numerical study. Int. J. Numer. Methods Biomed. Eng. 34(4):e2945, 2018.
Sullivan, C. B., and A. Kaszynski. PyVista: 3D plotting and mesh analysis through a streamlined interface for the Visualization Toolkit (VTK). J. Open Source Softw. 4(37):1450, 2019.
Sung, H. W., Y. Chang, C. T. Chiu, C. N. Chen, and H. C. Liang. Mechanical properties of a porcine aortic valve fixed with a naturally occurring crosslinking agent. Biomaterials. 20(19):1759–1772, 1999.
Toma, M., M. Ø. Jensen, D. R. Einstein, A. P. Yoganathan, R. P. Cochran, and K. S. Kunzelman. Fluid-structure interaction analysis of papillary muscle forces using a comprehensive mitral valve model with 3d chordal structure. Ann. Biomed. Eng. 44(4):942–953, 2016.
Watton, P., X. Luo, X. Wang, G. Bernacca, P. Molloy, and D. Wheatley. Dynamic modelling of prosthetic chorded mitral valves using the immersed boundary method. J. Biomech. 40(3):613–626, 2007.
Yap, C. H., H.-S. Kim, K. Balachandran, M. Weiler, R. Haj-Ali, and A. P. Yoganathan. Dynamic deformation characteristics of porcine aortic valve leaflet under normal and hypertensive conditions. Am. J. Physiol. Heart Circul. Physiol. 298(2):H395–H405, 2009.
Yun, B. M., L. Dasi, C. Aidun, and A. Yoganathan. Highly resolved pulsatile flows through prosthetic heart valves using the entropic lattice-Boltzmann method. J. Fluid Mech. 754:122–160, 2014.
Acknowledgements
ADK was supported in part by a grant from the National Heart, Lung and Blood Institute (1T32HL098049), Training Program in Mechanisms and Innovation in Vascular Disease. ADK and ALM were supported in part by the National Science Foundation SSI (Grant #1663671). ADK and NS were supported in part by American Heart Association Transformational Project Award (Grant # 19TPA34910000). NS was supported in part by the Stanford Bio-X Bowes Fellowship. Computing for this project was performed on the Stanford University’s Sherlock cluster with assistance from the Stanford Research Computing Center. Simulations were performed using the open-source solver package IBAMR, https://ibamr.github.io.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Stefan M. Duma oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
We performed a convergence study to evaluate the sensitivity of the phase-averaged velocity fields and flow rates to changes in simulation resolution. The fluid resolutions were set to \(\Delta x =\) 0.9, 0.68, 0.45, 0.34 and 0.28 mm. We ran each simulation ran for two cardiac cycles, then performed phase averaging on the second cycle and sampled onto the MRI mesh for comparisons, as described in “Post Processing” section. For \(\Delta x =\) 0.9 and 0.68 mm, we used a coarsened structure mesh with a target edge length of \(\Delta s = 0.45\) mm, for \(\Delta x =\) 0.45 and 0.34 mm we used the target edge length of \(\Delta s = 0.225\) mm, as used in the remainder of this work, and for \(\Delta x =\) 0.28 mm we use the leaflet mesh targeted to \(\Delta s = 0.225\) mm, and a slightly finer mesh for the vessel targeted to \(\Delta s = 0.2\) mm.
Exact convergence in IB method simulations is challenging to achieve due to diffuse coupling of the fluid–structure interface and the physical instability of the flow. The radius of the support of the discrete \(\delta\)-function is \(2.5\Delta x\), which depends on the fluid mesh width, meaning that the effective thickness of all objects in the structure depends on the fluid resolution. Thus, IB method coupling reduces the effective radius of the valve and vasculature proportional to \(\Delta x\), meaning that the effective radius converges to the true radius in a first order manner as \(\Delta x \rightarrow 0\). Resistance to forward flow depends more than linearly on radius (to the fourth power in the case of Poiseuille flow), and thus slow convergence of the flow rate under a specified pressure difference is expected. Alternative schemes could include compensatory measures to adjust the boundary conditions to achieve a more constant flow rate, but this would not reduce numerical error at the fluid–structure interfaces. Additionally, the Reynolds number of the flow is much greater than one, the flow is inertially dominated and flow structures are unstable in time. This effect is partially mitigated by phase averaging the flow.
The phase-averaged, resampled velocity fields during peak systole and flow rates at each resolution are shown in Fig. 10. Despite the limitations discussed above, we observe similar qualitative trends in the flow field at all resolutions. At all resolutions, a jet formed and angled up downstream of the valve orifice, as shown in the sagittal view. The jets showed a triangle-like cross section at \(x = 0\) with points aligned with the commissures. At \(x = 0.625\) cm, the jet appears like a rounded triangle in the opposing orientation, with its points aligned with the center of the leaflets. At \(x = 1.25\) cm, the jet is narrower downstream of the commissures, and wider downstream of the leaflets, again with a triangle-like cross section. The area of the jet increased with resolution, as expected given the IB method thickening of the valve structure. The narrowed jets at the two more coarse resolutions show locally elevated velocities relative to the two more fine resolutions. Figure 11 shows the instantaneous velocity fields at each resolution in the same axial and sagittal views. At \(\Delta x =\) 0.9 mm, the sagittal view shows a qualitatively different jet than at finer resolutions, with regions of lower velocity farther from the vessel wall, indicating insufficient resolution. At \(\Delta x =\) 0.9 and 0.68 mm, the jet is visibly narrowed compared to higher resolutions. While some features are similar at these two coarse resolutions, we conclude that the narrower jets indicate these simulations are under-resolved. Flows in the three finest resolutions, \(\Delta x =\) 0.45, 0.34 and 0.28 mm. appeared qualitatively similar, with slightly more fine structure detail in both the axial and sagittal views present at the edges of the jet. The jets in the axial views all showed a similar triangle-like cross section, slightly narrower downstream of the commissures, as in the phase-averaged fields. In both the phase-averaged and instantaneous fields, the three finest resolutions appear sufficiently similar that the conclusions of this study would be identical with any of these resolutions.
The flow rates, depicted in Fig. 12, increase with increasing resolution, also as expected given the increase in effective valve orifice area and radius. The maximum flow rates at \(\Delta x =\) 0.45 and 0.34 mm were 248.6 and 281.4 ml/s, respectively, a relative difference of 11.7%. The mean flow rates at \(\Delta x =\) 0.45 and 0.34 were 55.5 and 63.2 ml/s, respectively, a relative difference of 12.4%. The maximum flow rates at \(\Delta x =\) 0.34 and 0.28 mm were 281.3 and 299.8 ml/s, respectively, a relative difference of 6.1%. The mean flow rates at \(\Delta x =\) 0.34 and 0.28 mm were 63.2 and 67.4 ml/s, respectively, a relative difference of 6.2%. Thus the flow rates show signs of converging with increasing resolution, though some minor differences remain.
Figure 13 shows the integral metric \(I_{1}\) evaluated at \(x = 0\) cm with various resolutions, where each resolution uses its own velocity scale (see Eq. (18)). Values at \(\Delta x =\) 0.9, 0.68 were elevated relative to finer resolutions, indicating under resolution. Values of \(I_{1}\) at \(\Delta x =\) 0.45, 0.34 and 0.28 mm are extremely similar, with slight decrease as resolution increases. Values of \(I_{1}\) at \(x =\) 0.625 and 1.25 cm showed similar trends and are not shown.
Given the overall qualitative similarity and relative changes in flow rates, we believed all conclusions in this work would be similar with \(\Delta x =\) 0.45, 0.34 or 0.28 mm. We therefore selected \(\Delta x =\) 0.45 mm, twice the MRI resolution, for the main portion of this study.
Additionally, we compared averaging the second cycle with phase averaging the second, third and fourth cycles with a resolution of \(\Delta x = 0.45\) mm. We found the fields appeared qualitatively similar in both cases. Averaging the second, third and fourth cycles resulted in slightly worse relative error compared to experiment than the second alone. Comparing the two averaging methods at peak systole, relative error on velocity magnitude, the x-component of velocity was 0.07, and 0.09, respectively in \(L^{1}\), and 0.10 and 0.11 in \(L^{2}\). As these differences were substantially lower than relative differences between the simulation results and experiments, we ended all further simulations after the second cycle and use only the second cycle for phase averaging.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaiser, A.D., Schiavone, N.K., Elkins, C.J. et al. Comparison of Immersed Boundary Simulations of Heart Valve Hemodynamics Against In Vitro 4D Flow MRI Data. Ann Biomed Eng 51, 2267–2288 (2023). https://doi.org/10.1007/s10439-023-03266-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-023-03266-2