Abstract
Ten years have passed since the first commercial equipment for elastography was released; since then clinical utility has been demonstrated. Nowadays, most manufacturers offer an elastography option. The most widely available commercial elastography methods are based on strain imaging, which uses external tissue compression and generates images of the resulting tissue strain. However, imaging methods differ slightly among manufacturers, which results in different image characteristics, for example, spatial and temporal resolution, and different recommended measurement conditions. In addition, many manufacturers have recently provided a shear wave-based method, providing stiffness images based on shear wave propagation speed. Each method of elastography is designed on the basis of assumptions of measurement conditions and tissue properties. Thus, we need to know the basic principles of elastography methods and the physics of tissue elastic properties to enable appropriate use of each piece of equipment and to obtain more precise diagnostic information from elastography. From this perspective, the basic section of this guideline aims to support practice of ultrasound elastography.















Similar content being viewed by others
References
Samani A, Zubovits J, Plewes D. Elastic moduli of normal and pathological human breast tissues: an inversion-technique-based investigation of 169 samples. Phys Med Biol. 2007;52(6):1565–76.
Krouskop TA, Wheeler TM, Kallel F, et al. The elastic moduli of breast and prostate tissues under compression. Ultrason Imaging. 1998;20(4):260–74.
Wellman PS, Howe RD, Dalton E, et al. Breast tissue stiffness in compression is correlated to histological diagnosis. Harvard BioRobotics Laboratory, Technical Report, 1999.
Duck FA. Physical properties of tissues. New York: Academic; 1990.
Sarvazyan A, Hill CR. Physical chemistry of the ultrasound-tissue interaction. In: Hill CR, Bamber JC, Terhaar GR, editors. Physical principles of medical ultrasonics. 2nd ed. Chichester: Wiley; 2004. p. 223–35.
Parker KJ, Taylor LS, Gracewski S, et al. A unified view of imaging the elastic properties of tissue. J Acoust Soc Am. 2005;117(5):2705–12.
Greenleaf JF, Fatemi M, Insana M. Selected methods for imaging elastic properties of biological tissues. Annu Rev Biomed Eng. 2003;5:57–78.
Deffieux T, Montaldo G, Tanter M, et al. Shear wave spectroscopy for in vivo quantification of human soft tissues visco-elasticity. IEEE Trans Med Imaging. 2009;28(3):313–22.
Ophir J, Cespedes I, Ponnekanti H, et al. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991;13:111–34.
Parker KJ, Doyley MM, Rubens DJ. Imaging the elastic properties of tissue: the 20 year perspective. Phys Med Biol. 2011;56:R1–29.
Bamber JC, Bush NL. Freehand elasticity imaging using speckle decorrelation rate. Acoust Imaging. 1996;22:285–92.
Bamber JC, Barbone PE, Bush NL, et al. Progress in freehand elastography of the breast. IEICE Trans Inf Syst. 2002;E85D:5–14.
Shiina T, Doyley MM, Bamber JC. Strain imaging using combined RF and envelope autocorrelation processing. In: Proceedings of the 1996 IEEE Int Ultrasonics Symposium; 1996. p. 1331–6.
Varghese T, Ophir J. A theoretical framework for performance characterization of elastography: the strainfilter. IEEE Trans Ultrason Ferroelectr Freq Control. 1997;44:164–72.
Hall TJ, Zhu YN, Spalding CS. In vivo real-time freehand palpation imaging. Ultrasound Med Biol. 2003;29:427–35.
Shiina T, Nitta N, Ueno E, et al. Real time elasticity imaging using the combined autocorrelation method. J Med Ultrasonics. 2002;29:119–28.
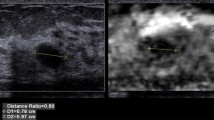
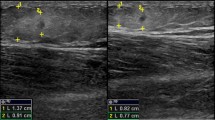
Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239(2):341–50.
Ueno E, Tohno E, Bando H, et al. New quantitative method in breast elastography: fat lesion ration (FLR). Abstract of RSNA 2007; LL-BR2123-H04.
Farrokh A, Wojcinski S, Degenhardt F, et al. Diagnostic value of strain ratio measurement in the differentiation of malignant and benign breast lesion. Ultrashall Med. 2011;32(4):400–5.
Matsumura T. Measurement of elastic property of breast tissue for elasticity imaging. In: Proceedings of the 2009 IEEE Ultrasonics Symposium; 2009. p. 1451–4.
Thomas A, Warm M, Hoopmann M, et al. Tissue Doppler and strain imaging for evaluating tissue elasticity of breast lesions. Acad Radiol. 2007;14(5):522–9.
Nightingale K, Bentley R, Gregg ET. Observations of tissue response to acoustic radiation force: opportunities for imaging. Ultrason Imaging. 2002;24(3):129–38.
Nightingale K, Soo MS, Nightingale R, et al. Acoustic radiation force impulse imaging: in vivo demonstration of clinical feasibility. Ultrasound Med Biol. 2002;28(2):227–35.
Nyborg WLM, Litovitz T, Davis C. Acoustic streaming. In: Mason WP, editor. Physical acoustics. New York: Academic; 1965. p. IIA 265–331.
Torr GR. The acoustic radiation force. Am J Phys. 1984;52:402–8.
Cho Seung Hyun, Lee Jae Young, Han Joon Koo, et al. Acoustic radiation force impulse elastography for the evaluation of focal solid hepatic lesions: preliminary findings. Ultrasound Med Biol. 2010;36(2):202–8.
D’Onofrio M, Gallotti A, Salvia R, et al. Acoustic radiation force impulse (ARFI) ultrasound imaging of pancreatic cystic lesions. Eur J Radiol. 2011;80(2):241–4.
Gallotti A, D’Onofrio M, Mucelli RP. Acoustic radiation force impulse (ARFI) technique in the ultrasound study with virtual touch tissue quantification of the superior abdomen. Radiol Med. 2010;115(6):889–97.
Clevert DA, Stock K, Klein B. Evaluation of acoustic radiation force impulse (ARFI) imaging and contrast-enhanced ultrasound in renal tumors of unknown etiology in comparison to histological findings. Clin Hemorheol Microcirc. 2009;43(1–2):95–107.
Barr RG, Zhang Z. Effects of precompression on elasticity imaging of the breast-development of a clinically useful semiquantitative method of precompression assessment. J Ultrasound Med. 2012;31:895–902.
Barnett SB, Duck F, Ziskin M. Recommendations on the safe use of ultrasound contrast agents. Ultrasound Med Biol. 2007;33:173–4.
Ultrasound Equipment and Safety Committee of The Japan Society of Ultrasonics in Medicine. Safe use of imaging equipment using acoustical radiation force. (http://www.jsum.or.jp/committee/m_and_s/acoustic_radiation.html).
Parker KJ, Huang SR, Musulin RA. Tissue response to mechanical vibrations for sonoelasticity imaging. Ultrasound Med Biol. 1990;16:241–6.
Sandrin L, Tanter M, Gennisson JL, et al. Shear elasticity probe for soft tissues with 1-D transient elastography. IEEE Trans UFFC. 2002;49(4):436–46.
Deffieux T, Montaldo G, Tanter M, et al. Shear wave spectroscopy for in vivo quantification of human soft tissues visco-elasticity. IEEE Trans Med Imaging. 2009;28(3):313–22.
Fujimoto K, Kato M, Kudo M, et al. Novel image analysis method using ultrasound elastography for noninvasive evaluation of hepatic fibrosis in patients with chronic hepatitis C. Oncology. 2013;84(suppl1):3–12.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shiina, T. JSUM ultrasound elastography practice guidelines: basics and terminology. J Med Ultrasonics 40, 309–323 (2013). https://doi.org/10.1007/s10396-013-0490-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-013-0490-z