Abstract
Background and objectives
The Lyon Consensus was conducted in 2017, leading to a revision of the diagnostic criteria of GERD. Conclusive GERD was defined as cases in which the distal esophageal acid exposure time (AET) is greater than 6% and there exists either peptic esophagitis, constriction, or long-segment Barrett’s mucosa with a Los Angeles classification of grade C or D. Borderline GERD is defined as cases in which AET is between 4 and 6% and there exists peptic esophagitis with a Los Angeles classification of either grade A or B. All other cases were defined as Inconclusive GERD. We conducted a retrospective investigation of the treatment results of laparoscopic fundoplication (LF) for GERD according to the Lyon Consensus and evaluated whether or not it is an effective treatment predictor.
Materials and methods
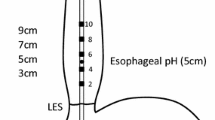
From among the cases of primary LF conducted on patients with GERD-related illnesses at our university hospital from June 2008 to March 2020, the subjects included 215 individuals who underwent upper gastrointestinal endoscopy and 24 h multichannel intraluminal impedance pH (MII-pH) testing prior to surgery. We compared the pathophysiology of the Conclusive GERD Group (Group A), Borderline GERD Group (Group B), and Inconclusive GERD Group (Group C), and then investigated the treatment results of each group. We used AFP classification for pathophysiological evaluation. For the acid reflux evaluation, we conducted MII-pH measurements using Sleuth, manufactured by Sandhill. The postoperative evaluation period was set to 3 months following surgery. The data are expressed using median values, with a statistical significance defined as p < 0.05 using the Kruskal–Wallis, Mann–Whitney, Wilcoxon signed-rank, and Chi-squared tests.
Results
Group A: 92 cases (43%, male 69 cases, age 57), Group B: 48 cases (22%, male 20 cases, age 52), and Group C: 75 cases (35%, male 69 cases, age 57). Regarding the patient backgrounds, while there were no significant differences in terms of gender or disease duration, those in Group A were significantly older than the other two groups, and there was a significant difference in Body Mass Index (BMI) between Group A and Group C. The results of each factor were: A factor (1 vs.1 vs. 1, p < 0.001), F factor (2 vs. 0 vs. 0, p < 0.001), and P factor (2 vs. 1 vs. 0, p < 0.001), with AET of 10.0 vs. 2.9 vs. 0.6, p < 0.001, and the disease had progressed more in Group A. There were also no differences in terms of surgical methods, hemorrhage volume, and intraoperative/postoperative complications; however, the use of mesh was higher and surgery duration was longer in Group A. There were obvious improvements in the A, F, and P factors and AET of each group following surgery (other than F and P of Group C, p < 0.001). The rate of recurrence was 15% in Group A, 8% in Group B, and 6% in Group C. It tended to be higher in Group A, but this was not statistically significant.
Conclusion
The classification of GERD pathophysiology based on the Lyon Consensus is satisfactory, with no significant differences in the rate of effect of LF. The Lyon Consensus is effective for ascertaining the severity and pathophysiology of GERD; however, we were unable to forecast the treatment results of LF.

Similar content being viewed by others
References
Roman S, Gyawali CP, Savarino E, GERD consensus group, et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: update of the porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil. 2017;29(10):1–15.
Gyawali CP, Roman S, Bredenoord AJ, et al. Classification of esophageal motor findings in gastro-esophageal reflux disease: conclusions from an international consensus group. Neurogastroenterol Motil. 2017;29(12):e13104.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67(7):1351–62.
Lin Y, Li Y, Liang M, et al. Acid exposure time > 6% might not improve the therapeutic outcome in chinese gastroesophageal reflux disease patients. J Neurogastroenterol Motil. 2020. https://doi.org/10.5056/jnm19219 (Epub ahead of print).
Ghisa M, Barberio B, Savarino V, et al. The Lyon Consensus: does it differ from the previous ones? J Neurogastroenterol Motil. 2020;26(3):311–21.
Zhang M, Tan N, Li Y, Chen M, Xiao Y. Esophageal physiologic profiles within erosive esophagitis in China: predominantly low-grade esophagitis with low reflux burden. Neurogastroenterol Motil. 2019;31(12):e13702.
Omura N, Kashiwagi H, Yano F, et al. Prediction of recurrence after laparoscopic fundoplication for erosive reflux esophagitis based on anatomy-function-pathology (AFP) classification. Surg Endosc. 2007;21(3):427–30.
Omura N, Yano F, Tsuboi K, et al. Surgical results of laparoscopic Toupet fundoplication for gastroesophageal reflux disease with special reference to recurrence. Esophagus. 2018;15(4):217–23.
Koch OO, Asche KU, Berger J, Weber E, Granderath FA, Pointner R. Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc. 2011;25(4):1024–30.
Tutuian R, Vela MF, Shay SS, Castell DO. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol. 2003;37(3):206–15.
Feussner H, Petri A, Walker S, Bollschweiler E, Siewert JR. The modified AFP score: an attempt to make the results of anti-reflux surgery comparable. Br J Surg. 1991;78(8):942–6.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45(2):172–80.
Hoshino M, Omura N, Yano F, et al. Comparison of laparoscopic Nissen and Toupet fundoplication using a propensity score matching analysis. Surg Today. 2017;47(10):1195–200.
Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62(4):325–32.
Burgerhart JS, van de Meeberg PC, Siersema PD, Smout AJ. Nocturnal and daytime esophageal acid exposure in normal-weight, overweight, and obese patients with reflux symptoms. Eur J Gastroenterol Hepatol. 2014;26(1):6–10.
Hiyama T, Matsuo K, Urabe Y, et al. Meta-analysis used to identify factors associated with the effectiveness of proton pump inhibitors against non-erosive reflux disease. J Gastroenterol Hepatol. 2009;24(8):1326–32.
Armijo PR, Pokala B, Misfeldt M, Pagkratis S, Oleynikov D. Predictors of hiatal hernia recurrence after laparoscopic anti-reflux surgery with hiatal hernia repair: a prospective database analysis. J Gastrointest Surg. 2019;23(4):696–701.
Broeders JA, Draaisma WA, Bredenoord AJ, Smout AJ, Broeders IA, Gooszen HG. Long-term outcome of Nissen fundoplication in non-erosive and erosive gastro-oesophageal reflux disease. Br J Surg. 2010;97(6):845–52.
Omura N, Kashiwagi H, Yano F, et al. Therapeutic effects of laparoscopic fundoplication for nonerosive gastroesophageal reflux disease. Surg Today. 2006;36(11):954–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study.
Conflict of interest
Drs. Masato Hoshino, Nobuo Omura, Fumiaki Yano, Kazuto Tsuboi, Se Ryung Yamamoto, Shunsuke Akimoto, Takahiro Masuda, Yuki Sakashita, Naoko Fukushima, and Hideyuki Kashiwagi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoshino, M., Omura, N., Yano, F. et al. Therapeutic effect of laparoscopic fundoplication for patients with GERD from the viewpoint of Lyon Consensus. Esophagus 18, 915–921 (2021). https://doi.org/10.1007/s10388-021-00843-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00843-z