Abstract
Background
In Japan, the majority of patients with gastroesophageal reflux disease have low-grade reflux esophagitis (RE), including minimal changes, and the modified Los Angeles (LA) classification is widely used. However, there have been few evaluations of interobserver agreement with this classification. This study was performed to elucidate the level of interobserver agreement for diagnosis low-grade RE, including minimal changes, and to identify any clinical factors that influenced the results.
Methods
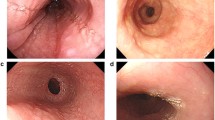
A total of 114 endoscopists from university hospitals, community hospitals, and private practice participated. They assessed the grade of esophagitis in 8 patients by viewing endoscopic images. The images were projected onto a screen, and all of the endoscopists reviewed images together. The diagnosis was selected from the following five categories: grade M, grade A, short-segment columnar-lined esophagus, diagnosis difficult due to poor image quality, and others. After discussiing the endoscopic diagnosis, the images were projected in a random order and the endoscopists viewed them again. Kappa coefficients of reliability were calculated before and after the discussion, and we also evaluated factors influencing the results.
Results
The kappa values obtained before and after discussion were 0.41 and 0.70, respectively. We found three factors that influenced interobserver agreement: specialty, years of experience with endoscopic examination, and mean esophageal observation time per endoscopic examination.
Conclusions
The modified LA classification is reliable for diagnosing low-grade RE (including minimal changes) in Japan, although several factors can influence interobserver agreement.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- GERD:
-
Gastroesophageal reflux disease
- JGES:
-
Japan Gastroenterological Endoscopy Society
- LA classification:
-
The Los Angeles classification
- LSBE:
-
Long-segment Barrett’s esophagus
- NERD:
-
Non-erosive reflux disease
- SSBE:
-
Short-segment Barrett’s esophagus
- SS-CLE:
-
Short-segment columnar-lined esophagus
References
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20.
Manabe N, Haruma K, Mihara M, Miyoshi E, Hamada H, Kido S, et al. The increasing incidence of reflux esophagitis during the past 20 years in Japan. Gastroenterology. 1999;166:A244.
Mishima I, Adachi K, Arima N, Amano K, Takashima T, Moritani M, et al. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese. Scand J Gastroenterol. 2005;40:1005–9.
Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92.
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Fujiwara Y, Higuchi K, Watanabe Y, Shiba M, Watanabe T, Tominaga K, et al. Prevalence of gastroesophageal reflux disease and gastroesophageal reflux disease symptoms in Japan. J Gastroenterol Hepatol. 2005;20:26–9.
Inamori M, Togawa J, Nagase H, Abe Y, Umezawa T, Nakajima A, et al. Clinical characteristics of Japanese reflux esophagitis patients as determined by Los Angeles classification. J Gastroenterol Hepatol. 2003;18:172–6.
Fujimoto K, Iwakiri R, Okamoto K, Oda K, Tanaka A, Tsunada S, Sakata H, et al. Characteristics of gastroesophageal reflux disease in Japan: increased prevalence in elderly women. J Gastroenterol. 2003;38(Suppl 15):3–6.
Fujimoto K. Review article: prevalence and epidemiology of gastro-oesophageal reflux disease in Japan. Aliment Pharmacol Ther. 2004;20(Suppl 8):5–8.
Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006;41:95–9.
Hoshihara Y, Hashimoto M. Endoscopic classification of reflux esophagitis. Nippon Rinsho. 2000;58:1808–12 (in Japanese with English abstract).
Amano Y, Ishimura N, Furuta K, Okita K, Masaharu M, Azumi T, et al. Interobserver agreement on classifying endoscopic diagnoses of nonerosive esophagitis. Endoscopy. 2006;38:1032–5.
Kusano M, Ino K, Yamada T, Kawamura O, Toki M, Ohwada T, et al. Interobserver and intraobserver variation in endoscopic assessment of GERD using the “Los Angeles” classification. Gastrointest Endosc. 1999;49:700–4.
Hoshihara Y, Kogure T, Yamamoto T, Hashimoto M, Yamamoto N, Tanaka T, et al. Diagnosis of short segment Barrett’s esophagus. Stom Intest. 1999;34:133–9.
Schnell T, Sontag S, Chejfec G. Adenocarcinoma arising in tongues or in short segments of Barrett’s esophagus. Dig Dis Sci. 1992;37:137–43.
Nandurkar S, Tally NJ, Martin CJ, Ng THK, Adams S. Short segment Barrett’s oesophagus: prevalence, diagnosis and associations. Gut. 1997;40:710–5.
de Mas CR, Kramer M, Seifert E, Rippin G, Vieth M, Stolte M. Short Barrett: prevalence and risk factors. Scand J Gastroenterol. 1999;34:1065–70.
Harada M, Nagashima R, Takeda H, Takahashi T. Endoscopic resection of adenocarcinoma arising in a tongue of Barrett’s esophagus. Gastrointest Endosc. 2000;52:427–9.
Yagi K, Nakamura A, Sekine A, Tamiya Y, Oyamatsu M. Magnified view of adenocarcinoma in short segment Barrett’s esophagus treated by endoscopic mucosal resection. Gastrointest Endosc. 2002;55:278–81.
Aoki T, Kawamura Y, Kouzu T. Definition of Barrett esophagus (epithelium). Rep Jpn Soc Esophageal Dis. 2000;20–3 (in Japanese).
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46.
Siegel S, Castellan NJ Jr. Nonparametric statistics for the behavioral sciences. 2nd ed. New York: McGraw-Hill Book Co.; 1988. p. 285–91.
McDougall NI, Johnston BT, Collins JS, McFarland RJ, Love AH. Disease progression in gastro-oesophageal reflux disease as determined by repeat oesophageal pH monitoring and endoscopy 3 to 4.5 years after diagnosis. Eur J Gastroenterol Hepatol. 1997;9:1161–7.
Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–7.
Joh T, Miwa H, Higuchi K, Shimatani T, Manabe N, Adachi K, ARS Research Group, et al. Validity of endoscopic classification of nonerosive reflux disease. J Gastroenterol. 2007;42:444–9.
Kusano M, Shirai N, Yamaguchi K, Hongo M, Chiba T, Kinoshita Y, Acid-Related Symptom (ARS) Research Group. It is possible to classify non-erosive reflux disease (NERD) patients into endoscopically normal groups and minimal change groups by subjective symptoms and responsiveness to rabeprazole—a report from a study with Japanese patients. Dig Dis Sci. 2008;53:3082–94.
Miwa H, Yokoyama T, Hori K, Sakagami T, Oshima T, Tomita T, et al. Interobserver agreement in endoscopic evaluation of reflux esophagitis using a modified Los Angeles classification incorporating grades N and M: a validation study in a cohort of Japanese endoscopists. Dis Esophagus. 2008;21:355–63.
Vieth M, Fiocca R, Haringsma J, Delarive J, Wiesel PH, Tam W, et al. Radial distribution of dilated intercellular spaces of the esophageal squamous epithelium in patients with reflux disease exhibiting discrete endoscopic lesions. Dig Dis. 2004;22:208–12.
Caviglia R, Ribolsi M, Maggiano N, Gabbrielli AM, Emerenziani S, Guarino MP, et al. Dilated intercellular spaces of esophageal epithelium in nonerosive reflux disease patients with physiological esophageal acid exposure. Am J Gastroenterol. 2005;100:543–8.
Narayani RI, Burton MP, Young GS. Utility of esophageal biopsy in the diagnosis of nonerosive reflux disease. Dis Esophagus. 2003;16:187–92.
Falk GW. Is conventional endoscopic identification of non-erosive reflux disease adequate? Digestion. 2008;78(Suppl 1):17–23.
Pandolfino JE, Vakil NB, Kahrilas PJ. Comparison of inter- and intraobserver consistency for grading of esophagitis by expert and trainee endoscopists. Gastrointest Endosc. 2002;56:639–43.
Bytzer P, Havelund T, Hansen JM. Interobserver variation in the endoscopic diagnosis of reflux esophagitis. Scand J Gastroenterol. 1993;28:119–25.
Wu JC. Endoscopic grading of reflux esophagitis in Asia: it’s time to start. J Gastroenterol Hepatol. 2009;24:1–2.
Acknowledgments
The Committee for Assessment of Endoscopic Finding of GERD comprises the following investigators: Junichi Akiyama from International Medical Center of Japan, Tokyo, Japan; Yuji Amano from Division of Endoscopy, Shimane University Hospital, Izumo-shi, Japan; Shuichi Ohara from Tohoku Rosai Hospital, Sendai, Japan; Mitsuru Kaise from Toranomon Hospital, Tokyo, Japan; Mototsugu Kato and Katsuhiro Mabe from Hokkaido University Hospital, Sapporo, Japan; Tetsuyuki Kawano from Tokyo Medical and Dental University, Tokyo, Japan; Motoyasu Kusano from Gunma University Hospital, Maebashi, Japan; Kaiyo Takubo from Tokyo Metropolitan Geriatric Hospital, Tokyo, Japan; Hideki Toyota from Happy GI Clinic, Kameyamashi-honmachi, Japan; Kiyoshi Ashida from Saiseikai Nakatsu Hospital, Osaka, Japan; Hiroto Miwa from Hyogo College of Medicine, Nishinomiya, Japan; Kazuyoshi Yagi from Niigata Prefectural Yoshida Hospital, Yoshida-machi, Japan; Haruhiro Yamashita from Okayama Medical Center, Okayama, Japan.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manabe, N., Haruma, K., Hoshihara, Y. et al. Interobserver agreement on endoscopic diagnosis of low-grade reflux esophagitis, including minimal changes. Esophagus 9, 9–16 (2012). https://doi.org/10.1007/s10388-011-0307-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-011-0307-3