Abstract
Purpose
We investigated the differences in displacement of the outer and inner macular retina toward the optic disc after vitrectomy with internal limiting membrane (ILM) peeling for epiretinal membrane (ERM). Foveal avascular zone (FAZ) area changes were also investigated.
Study design
Retrospective observational study
Methods
This retrospective observational case series included 45 eyes of 43 patients that underwent vitrectomy with ERM and ILM peeling for ERM and 38 normal eyes. The locations of the centroid of the FAZ (C-FAZ, center of the foveal inner retina) and foveal bulge (center of the foveal outer retina) were determined using 3×3mm superficial optical coherence tomography angiography. C-FAZ and foveal bulge displacements, and the pre- and postoperative FAZ areas and their associated factors, were investigated.
Results
Postoperative C-FAZ dislocated significantly more toward the optic disc than in pre-operative or normal eyes (P<0.001). C-FAZ and foveal bulge displaced toward the optic disc after surgery; C-FAZ showed significantly greater displacement than foveal bulge (P<0.001). The pre- and postoperative FAZ areas were correlated (P=0.01). Preoperative FAZ areas ≧0.10mm2 were reduced after surgery, and FAZ areas < 0.10mm2 were increased, independent of foveal displacement.
Conclusion
ILM peeling during vitrectomy for ERM caused larger displacement of the inner and smaller displacement of the outer retinas, towards the optic disc. Postoperative changes in the FAZ area were dependent on the baseline FAZ area, but not on the foveal displacement. ILM may physiologically exert centrifugal tractional forces on the fovea.






Similar content being viewed by others
Data availability
The datasets analyzed during the current study are not publicly available because of the hospital’s policy to protect personal information of the participants but are available from the corresponding author on reasonable request.
References
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J. Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology. 1999;106:1392–8.
Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939–48.
Kadonosono K, Itoh N, Uchio E, Nakamura S, Ohno S. Staining of internal limiting membrane in macular hole surgery. Arch Ophthalmol. 2000;118:1116–8.
Smiddy WE, Feuer W, Cordahi G. Internal limiting membrane peeling in macular hole surgery. Ophthalmology. 2001;108:1471–6.
Haritoglou C, Gass CA, Schaumberger M, Ehrt O, Gandorfer A, Kampik A. Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol. 2001;132:363–8.
Kumagai K, Furukawa M, Ogino N, Uemura A, Demizu S, Larson E. Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina. 2004;24:721–7.
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, et al. Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling. Retina. 2006;26:631–6.
Almony A, Nudleman E, Shah GK, Blinder KJ, Eliott DB, Mittra RA, et al. Techniques, rationale, and outcomes of internal limiting membrane peeling. Retina. 2012;32:877–91.
Bovey EH, Uffer S, Achache F. Surgery for epimacular membrane: impact of retinal internal limiting membrane removal on functional outcome. Retina. 2004;24:728–35.
Kwok AKH, Lai TYY, Yuen KSC. Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Exp Ophthalmol. 2005;33:379–85.
Hattori K, Kataoka K, Takeuchi J, Ito Y, Terasaki H. Predictive Factors of Surgical Outcomes in Vitrectomy for Myopic Traction Maculopathy. Retina. 2018;38(Suppl 1):S23–30.
Taniuchi S, Hirakata A, Itoh Y, Hirota K, Inoue M. Vitrectomy with or without internal limiting membrane peeling for each stage of myopic traction maculopathy. Retina. 2013;33:2018–25.
Shimada N, Sugamoto Y, Ogawa M, Takase H, Ohno-Matsui K. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012;154:693–701.
Shiraki N, Wakabayashi T, Ikuno Y, Matsumura N, Sato S, Sakaguchi H, et al. Fovea-sparing versus standard internal limiting membrane peeling for myopic traction maculopathy: a study of 102 consecutive cases. Ophthalmol Retina. 2020;4:1170–80.
Iwasaki M, Miyamoto H, Okushiba U, Imaizumi H. Fovea-sparing internal limiting membrane peeling versus complete internal limiting membrane peeling for myopic traction maculopathy. Jpn J Ophthalmol. 2020;64:13–21.
Ho TC, Yang CM, Huang JS, Yang CH, Yeh PT, Chen TC, et al. Long-term outcome of foveolar internal limiting membrane nonpeeling for myopic traction maculopathy. Retina. 2014;34:1833–40.
Kawano K, Ito Y, Kondo M, Ishikawa K, Kachi S, Ueno S, et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye (Lond). 2013;27:871–7.
Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol. 2014;157:971–7.
Akahori T, Iwase T, Yamamoto K, Ra E, Kawano K, Ito Y, et al. Macular displacement after vitrectomy in eyes with idiopathic macular hole determined by optical coherence tomography angiography. Am J Ophthalmol. 2018;189:111–21.
Yoshikawa M, Murakami T, Nishijima K, Uji A, Ogino K, Horii T, et al. Macular migration toward the optic disc after inner limiting membrane peeling for diabetic macular edema. Invest Ophthalmol Vis Sci. 2013;54:629–35.
Tadayoni R, Paques M, Massin P, Mouki-Benani S, Mikol J, Gaudric A. Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology. 2001;108:2279–83.
Ito Y, Terasaki H, Takahashi A, Yamakoshi T, Kondo M, Nakamura M. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology. 2005;112:1415–20.
Mitamura Y, Ohtsuka K. Relationship of dissociated optic nerve fiber layer appearance to internal limiting membrane peeling. Ophthalmology. 2005;112:1766–70.
Spaide RF. “Dissociated optic nerve fiber layer appearance” after internal limiting membrane removal is inner retinal dimpling. Retina. 2012;32:1719–26.
Sakimoto S, Ikuno Y, Fujimoto S, Sakaguchi H, Nishida K. Characteristics of the retinal surface after internal limiting membrane peeling in highly myopic eyes. Am J Ophthalmol. 2014;158(762–8): e1.
Amouyal F, Shah SU, Pan CK, Schwartz SD, Hubschman JP. Morphologic features and evolution of inner retinal dimples on optical coherence tomography after internal limiting membrane peeling. Retina. 2014;34:2096–102.
Fukukita H, Ito Y, Iwase T, Kaneko H, Yasuda S, Kataoka K, et al. Inner macular changes after vitrectomy with internal limiting membrane peeling for rhegmatogenous retinal detachment: similarity with alport syndrome. Retina. 2019;39:2332–40.
Tuifua TS, Abraham JR, Srivastava SK, Kaiser PK, Reese J, Ehlers JP. Longitudinal ellipsoid zone and outer retinal integrity dynamics after epiretinal membrane surgery. Retina. 2022;42:265–73.
Kuppuswamy Parthasarathy M, Bhende M. Deviation in the position of foveal bulge from foveal center in normal subjects measured using spectral-domain OCT. Ophthalmol Retina. 2018;2:337–42.
Hasegawa T, Ueda T, Okamoto M, Ogata N. Relationship between presence of foveal bulge in optical coherence tomographic images and visual acuity after rhegmatogenous retinal detachment repair. Retina J Retinal Vitreous Dis. 2014;34:1848–53.
Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99–113.
Kitagawa Y, Shimada H, Shinojima A, Nakashizuka H. Foveal avascular zone area analysis using optical coherence tomography angiography before and after idiopathic epiretinal membrane surgery. Retina. 2019;39:339–46.
Okawa Y, Maruko I, Kawai M, Hasegawa T, Arakawa H, Iida T. Foveal structure and vasculature in eyes with idiopathic epiretinal membrane. PLoS ONE. 2019;14: e0214881.
Kumagai K, Furukawa M, Suetsugu T, Ogino N. Foveal avascular zone area after internal limiting membrane peeling for epiretinal membrane and macular hole compared with that of fellow eyes and healthy controls. Retina. 2018;38:1786–94.
Momota A, Iwase T, Akahori T, Goto K, Yamamoto K, Ra E, et al. Association between displacement and thickness of macula after vitrectomy in eyes with epiretinal membrane. Sci Rep. 2020;10:13227.
Kunikata H, Yasuda M, Aizawa N, Osada U, Nishiguchi KM, Abe T, et al. Retinal sensitivity and vessel density after macular hole surgery with the superior inverted internal limiting membrane flap technique. Retina. 2021;41:45–53.
Kaneko H, Hirata N, Shimizu H, Kataoka K, Nonobe N, Mokuno K, et al. Effect of internal limiting membrane peeling on visual field sensitivity in eyes with epiretinal membrane accompanied by glaucoma with hemifield defect and myopia. Jpn J Ophthalmol. 2021;65:380–7.
Tsuchiya S, Higashide T, Sugiyama K. Visual field changes after vitrectomy with internal limiting membrane peeling for epiretinal membrane or macular hole in glaucomatous eyes. PLoS ONE. 2017;12: e0177526.
Acknowledgements
This work was supported in part by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Numbers 19K09989 to HT and 16K11265 to YI.
Funding
Japan Society for the Promotion of Science,16K11265,Yasuki Ito, 19K09989, Hiroko Terasaki.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y. Taki, None; Y. Ito, Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Canon, Kowa, Santen, Bayer, ZEISS, Novartis, Pfizer); J. Takeuchi, None; H. Ito, None; Y. Nakano, None; A. F. Sajiki, None; E. Horiguchi, None; H. Ohta, None; K. Kataoka, Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Novartis, Senju, Santen, Boehringer Ingelheim, Bayer); H. Terasaki, Grants or contracts (ZEISS, Kowa, Otsuka, Senju, Santen, Alcon, Sanofi, Novartis, ROHTO, Bayer, Wakamoto, HOYA, Johnson & Johnson), Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Otsuka, Kowa, Santen, Senju, Sanofi, Alcon, ROHTO, Novartis, Wakamoto, Bayer), Support for attending meetings and/or travel (Bayer).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Yasuki Ito
Supplementary Information
Below is the link to the electronic supplementary material.
10384_2022_964_MOESM1_ESM.tif
Supplementary Fig. 1 Retinal layer thickness measurement. Foveal thickness and retinal layer thickness of the entire retina, the inner retina (the inner limiting membrane to the outer plexiform layer), and the outer retina (the outer nuclear layer to the retinal pigment epithelium) were measured manually at 1 mm both nasally and temporally to the foveal center (foveal bulge) by using the caliper function of the built-in software of the swept source optical coherence tomography (SS-OCT) device. Supplementary file1 (TIF 20894 KB)
10384_2022_964_MOESM2_ESM.tif
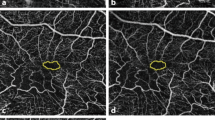
Supplementary Fig. 2 Adjustment of the location of the pre- and postoperative optical coherence tomography (OCT) angiography images. Location of pre- and postoperative en face superficial OCT angiography images were overlaid (a and c), after adjusting the landmarks on choroidal OCT angiography images (b and d, yellow dotted line). Supplementary file2 (TIF 9212 KB)
About this article
Cite this article
Taki, Y., Ito, Y., Takeuchi, J. et al. Displacement of the retina and changes in the foveal avascular zone area after internal limiting membrane peeling for epiretinal membrane. Jpn J Ophthalmol 67, 74–83 (2023). https://doi.org/10.1007/s10384-022-00964-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-022-00964-7