Abstract
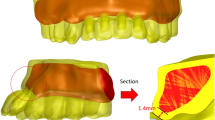
The purpose of this study was to analyze the biomechanical properties of implants made of different materials to replace missing teeth by using three-dimensional finite element analysis and provide a theoretic basis for clinical application. CBCT data was imported into the Mimics and 3-Matic to construct the three-dimensional finite element model of a missing tooth restored by an implant. Then, the model was imported into the Marc Mentat. Based on the variations of the implant materials (titanium, titanium–zirconia, zirconia and poly (ether-ether-ketone) (PEEK)) and bone densities (high and low), a total of eight models were created. An axial load of 150 N was applied to the crown of the implant to simulate the actual occlusal situation. Both the maximum values of stresses in the cortical bone and implant were observed in the Zr-low model. The maximum displacements of the implants were also within the normal range except for the PEEK models. The cancellous bone strains were mainly distributed in the apical area of the implant, and the maximum value (3225 μstrain) was found in PEEK-low model. Under the premise of the same implant material, the relevant data from various indices in low-density bone models were larger than that in high-density bone models. From the biomechanical point of view, zirconia, titanium and titanium–zirconia were all acceptable implant materials for replacing missing teeth and possessed excellent mechanical properties, while the application of PEEK material needs to be further optimized and modified.






Similar content being viewed by others
Data availability
The datasets used and/or analyses during the current study available from the corresponding author on reasonable request.
References
Liu C, Xing Y, Li Y, Lin Y, Xu J, Wu D. Bone quality effect on short implants in the edentulous mandible: a finite element study. BMC Oral Health. 2022;22:139.
Liang C, Liu X, Yan Y, Sun R, Li J, Geng W. Effectiveness and mechanisms of low-intensity pulsed ultrasound on osseointegration of dental implants and biological functions of bone marrow mesenchymal stem cells. Stem Cells Int. 2022;2022:1–16.
Guo T, Scimeca J-C, Ivanovski S, Verron E, Gulati K. Enhanced corrosion resistance and local therapy from nano-engineered titanium dental implants. Pharmaceutics. 2023;15:315.
Haseeb S, Vinaya KC, Vijaykumar N, Sree Durga BA, Kumar A, Sruthi MK. Finite element evaluation to compare stress pattern in bone surrounding implant with carbon fiber-reinforced poly-ether-ether-ketone and commercially pure titanium implants. Natl J Maxillofac Surg. 2022;13:243.
Vijayaraghavan V, Sabane AV, Tejas K. Hypersensitivity to titanium: a less explored area of research. The J Indian Prosthodont Soc. 2012;12:201–7.
Haugen HJ, Chen H. Is there a better biomaterial for dental implants than titanium?—a review and meta-study analysis. J Funct Biomater. 2022;13:46.
Wen CE, Yamada Y, Hodgson PD. Fabrication of novel TiZr alloy foams for biomedical applications. Mater Sci Eng C. 2006;26:1439–44.
Rutkowski R, Smeets R, Neuhöffer L, Stolzer C, Strick K, Gosau M, et al. Success and patient satisfaction of immediately loaded zirconia implants with fixed restorations one year after loading. BMC Oral Health. 2022;22:198.
Choi S-M, Choi H, Lee D-H, Hong M-H. Comparative finite element analysis of mandibular posterior single zirconia and titanium implants: a 3-dimensional finite element analysis. J Adv Prosthodont. 2021;13:396.
Fernandes PRE, Otero AIP, Fernandes JCH, Nassani LM, Castilho RM, de Oliveira Fernandes GV. Clinical performance comparing titanium and titanium–zirconium or zirconia dental implants: a systematic review of randomized controlled trials. Dent J (Basel). 2022;10:83.
Guerrero-Gironés J, López-García S, Pecci-Lloret MR, Pecci-Lloret MP, García-Bernal D. Influence of dual-cure and self-cure abutment cements for crown implants on human gingival fibroblasts biological properties. Ann Anat Anatomischer Anzeiger. 2022;239:151829.
Roehling S, Astasov-Frauenhoffer M, Hauser-Gerspach I, Braissant O, Woelfler H, Waltimo T, et al. In vitro biofilm formation on titanium and zirconia implant surfaces. J Periodontol. 2017;88:298–307.
Schwarz F, Derks J, Monje A, Wang H-L. Peri-implantitis. J Clin Periodontol. 2018;45:S246–66.
Wang C-F, Huang H-L, Lin D-J, Shen Y-W, Fuh L-J, Hsu J-T. Comparisons of maximum deformation and failure forces at the implant–abutment interface of titanium implants between titanium-alloy and zirconia abutments with two levels of marginal bone loss. Biomed Eng Online. 2013;12:45.
Papathanasiou I, Kamposiora P, Papavasiliou G, Ferrari M. The use of PEEK in digital prosthodontics: a narrative review. BMC Oral Health. 2020;20:217.
Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodont Res. 2016;60:12–9.
Su JJ, Lin YJ, Xing XJ, Chen J. Research progress of polyetheretherketone and its composites in the field of dental implant. Zhonghua Kou Qiang Yi Xue Za Zhi. 2022;57:1084–90.
Darawsheh HM, Safronova AA, Vasil’ev YuL, Makarova NI, Diachkova EY, Saleeva GT, et al. Choosing the optimal mandible position for inferior alveolar nerve block (IANB) using finite element analysis. Ann Anat Anatomischer Anzeiger. 2023;247:152055.
Xie B, Chen J, Zhao T, Shen J, Dörsam I, He Y. Three-dimensional finite element analysis of anterior fixed partial denture supported by implants with different materials. Ann Anat Anatomischer Anzeiger. 2022;243:151943.
Katranji A, Misch K, Wang HL. Cortical bone thickness in dentate and edentulous human cadavers. J Periodontol. 2007;78(5):874–8.
Dörsam I, Bauroth A, Keilig L, Bourauel C, Heinemann F. Definition of a drilling protocol for mini dental implants in different bone qualities. Ann Anat Anatomischer Anzeiger. 2020;231:151511.
Wang L, Fu Z, Hu Z, Li M, Qiu L, Gao Z. Biomechanical behaviour of implant prostheses and adjacent teeth according to bone quality: a finite element analysis. Eur J Oral Sci. 2022;130.
Burstein J, Mastin C, Le B. Avoiding injury to the inferior alveolar nerve by routine use of intraoperative radiographs during implant placement. J Oral Implantol. 2008;34:34–8.
Kochar SP, Reche A, Paul P. The etiology and management of dental implant failure: a review. Cureus. 2022;14(10):e30455.
Misch CE, Crawford EA. Predictable mandibular nerve location–a clinical zone of safety. Dent Today. 1990;9:32–5.
Truhlar RS, Orenstein IH, Morris HF, Ochi S. Distribution of bone quality in patients receiving endosseous dental implants. J Oral Maxillofac Surg. 1997;55:38–45.
García-Braz, Prados-Privado, Zanatta, Calvo-Guirado, Prados-Frutos, Gehrke. A finite element analysis to compare stress distribution on extra-short implants with two different internal connections. J Clin Med. 2019;8:1103.
Jin Z-H, Peng M-D, Li Q. The effect of implant neck microthread design on stress distribution of peri-implant bone with different level: a finite element analysis. J Dent Sci. 2020;15:466–71.
Ogura R, Kato H, Okada D, Foxton R, Ikeda M, Miura H. The relationship between bite force and oral sensation during biting in molars. Aust Dent J. 2012;57:292–9.
Pisani MX, Presotto AGC, Mesquita MF, Barão VAR, Kemmoku DT, Del Bel Cury AA. Biomechanical behavior of 2-implant– and single-implant–retained mandibular overdentures with conventional or mini implants. J Prosthet Dent. 2018;120:421–30.
John J, Rangarajan V, Savadi RC, Satheesh Kumar KS, Satheesh KP. A finite element analysis of stress distribution in the bone, around the implant supporting a mandibular overdenture with ball/o ring and magnetic attachment. J Indian Prosthodont Soc. 2012;12:37–44.
Maeda Y, Horisaka M, Yagi K. Biomechanical rationale for a single implant-retained mandibular overdenture: an in vitro study. Clin Oral Implants Res. 2008;19:271–5.
Lyakhov PA, Dolgalev AA, Lyakhova UA, Muraev AA, Zolotayev KE, Semerikov DY. Neural network system for analyzing statistical factors of patients for predicting the survival of dental implants. Front Neuroinform. 2022;16.
Koch FP, Weng D, Krämer S, Biesterfeld S, Jahn-Eimermacher A, Wagner W. Osseointegration of one-piece zirconia implants compared with a titanium implant of identical design: a histomorphometric study in the dog. Clin Oral Implants Res. 2010;21:350–6.
Hasan I, Röger B, Heinemann F, Keilig L, Bourauel C. Influence of abutment design on the success of immediately loaded dental implants: experimental and numerical studies. Med Eng Phys. 2012;34:817–25.
Almugla YM. Prevalence of missing first permanent molars in a selected population in a university dental clinic setting: a retrospective radiographic study. Int J Clin Pediatr Dent. 2021;14:269–72.
Shigli K, Hebbal M, Angadi GS. Relative contribution of caries and periodontal disease in adult tooth loss among patients reporting to the Institute of Dental Sciences, Belgaum, India. Gerodontology. 2009;26:214–8.
Mosavar A, Ziaei A, Kadkhodaei M. The effect of implant thread design on stress distribution in anisotropic bone with different osseointegration conditions: a finite element analysis. Int J Oral Maxillofac Implants. 2015;30:1317–26.
Lovatto ST, Bassani R, Sarkis-Onofre R, dos Santos MBF. Influence of different implant geometry in clinical longevity and maintenance of marginal bone: a systematic review. J Prosthodont. 2019;28:e713–21.
Talmazov G, Veilleux N, Abdulmajeed A, Bencharit S. Finite element analysis of a one-piece zirconia implant in anterior single tooth implant applications. PLoS ONE. 2020;15:e0229360.
Akca K, Iplikcioglu H. Finite element stress analysis of the effect of short implant usage in place of cantilever extensions in mandibular posterior edentulism. J Oral Rehabil. 2002;29:350–6.
Depprich R, Naujoks C, Ommerborn M, Schwarz F, Kübler NR, Handschel J. Current findings regarding zirconia implants. Clin Implant Dent Relat Res. 2014;16:124–37.
Altuna P, Lucas-Taulé E, Gargallo-Albiol J, Figueras-Álvarez O, Hernández-Alfaro F, Nart J. Clinical evidence on titanium–zirconium dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45(7):842–50.
Kobayashi E, Matsumoto S, Doi H, Yoneyama T, Hamanaka H. Mechanical properties of the binary titanium–zirconium alloys and their potential for biomedical materials. J Biomed Mater Res. 1995;29(8):943–50.
Da Silva GG, Shimano MVW, Macedo AP, Da Costa Valente ML, Dos Reis AC. In vitro assessment of polyetheretherketone for an attachment component for an implant-retained overdenture. J Prosthet Dent. 2022;127(2):319.e1-319.e8.
Pratheep K, Abraham A, Annapoorni H, Vigneshwaran S. Comparative evaluation of stresses in tooth implant connected fixed partial denture by varying the implant design and position: A 3D finite element study. Indian J Dent Res. 2013;24:439.
Frost HM. Bone’s mechanostat: a 2003 update. Anat Rec. 2003;275A:1081–101.
Robling AG, Castillo AB, Turner CH. Biomechanical and molecular regulation of bone remodeling. Annu Rev Biomed Eng. 2006;8:455–98.
Sarot JR, Contar CMM, da Cruz ACC, de Souza MR. Evaluation of the stress distribution in CFR-PEEK dental implants by the three-dimensional finite element method. J Mater Sci Mater Med. 2010;21:2079–85.
Cook SD, Weinstein AM, Klawitter JJ, Kent JN. Quantitative histologic evaluation of LTI carbon, carbon-coated aluminum oxide and uncoated aluminum oxide dental implants. J Biomed Mater Res. 1983;17:519–38.
Almasi D, Iqbal N, Sadeghi M, Sudin I, Abdul Kadir MR, Kamarul T. Preparation methods for improving PEEK’s bioactivity for orthopedic and dental application: a review. Int J Biomater. 2016;2016:1–12.
Premnath K, Sridevi J, Kalavathy N, Nagaranjani P, Sharmila MR. Evaluation of stress distribution in bone of different densities using different implant designs: a three-dimensional finite element analysis. J Indian Prosthodont Soc. 2013;13:555–9.
Heinemann F, Hasan I, Bourauel C, Biffar R, Mundt T. Bone stability around dental implants: treatment related factors. Ann Anat Anatomischer Anzeiger. 2015;199:3–8.
Tribst JM, de Morais D, Alonso A, Piva A de OD, Borges AS. Comparative three-dimensional finite element analysis of implant-supported fixed complete arch mandibular prostheses in two materials. J Indian Prosthodont Soc. 2017;17:255.
Solberg K, Heinemann F, Pellikaan P, Keilig L, Stark H, Bourauel C, et al. Finite element analysis of different loading conditions for implant-supported overdentures supported by conventional or mini implants. Comput Methods Biomech Biomed Eng. 2017;20:770–82.
Houdaifa R, Alzoubi H, Jamous I. Three-dimensional finite element analysis of worn molars with prosthetic crowns and onlays made of various materials. Cureus. 2022;14(10):e30240.
He Y, Hasan I, Keilig L, Chen J, Pan Q, Huang Y, et al. Combined implant-residual tooth supported prosthesis after tooth hemisection: a finite element analysis. Ann Anat Anatomischer Anzeiger. 2016;206:96–103.
Mesnard M, Ramos A, Simões JA. Influences of implant condyle geometry on bone and screw strains in a temporomandibular implant. J Cranio-Maxillofac Surg. 2014;42:194–200.
Qian Y, Fan Y, Liu Z, Zhang M. Numerical simulation of tooth movement in a therapy period. Clin Biomech. 2008;23:S48-52.
Funding
This study was funded by the Science & Technology Department of Sichuan Province, China (No. 2022YFS0282), Office of Science & Technology and Talent Work of Luzhou, China (NO. 2021-JYJ-67), Southwest Medical University (2021ZKZD007), and the cooperative project between Xuzhou District People's Government and Southwest Medical University (2021XZXNYD02).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. YG established the research model, calculated the research indexes of models and was the major contributor in writing the manuscript. XH and WX contributed to analysis and methodology. YD and ZX contributed to validation and formal analysis. JC contributed to data curation and performed the analysis with constructive discussions. YH supervised and revised the manuscript as the corresponding author. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
This study was approved by the Institutional Ethics Committee of the Affiliated Stomatological Hospital of Southwest Medical University (certificate number, 20220525001) and conducted in accordance with the Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Cone-beam computed tomography (CBCT) scans of the adult patient with mandibular first molar loss were obtained, and the patient signed the informed consent and agreed to use the relevant data of imaging examination.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, Y., He, X., Xu, W. et al. Three-dimensional finite element analysis of the biomechanical properties of different material implants for replacing missing teeth. Odontology (2024). https://doi.org/10.1007/s10266-024-00942-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10266-024-00942-0