Abstract
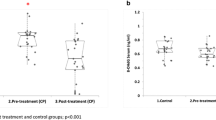
This cross-section study was designed to assess the effect of topical application of melatonin to the gingiva on salivary RANKL, osteoprotegrin (OPG) and melatonin levels as well as plasma melatonin in 30 patients with diabetes and periodontal disease and in a control group of 30 healthy subjects. Salivary RANKL and OPG were measured by enzyme-linked immunosorbent assay and salivary and plasma melatonin by radioimmunoassay using commercial kits. Periodontograms were performed using the Florida Probe®. Diabetic patients were treated with topical application of melatonin (1 % orabase cream formula) once daily for 20 days. Patients with diabetes showed significantly higher mean levels of salivary RANKL than healthy subjects as well as significantly lower values of salivary OPG and salivary and plasma melatonin. After treatment with melatonin, there was a statistically significant decrease of the gingival index, pocket depth and salivary levels of RANKL, and a significant rise in salivary values of OPG. Changes of salivary OPG levels before and after topical melatonin treatment correlated significantly with changes in the gingival index and pocket depth. Treatment with topical melatonin was associated with an improvement in the gingival index and pocket depth, a reduction in salivary concentrations of RANKL and increase in salivary concentrations of OPG, which indicates that melatonin has a favorable effect in slowing osteoclastogenesis, improving the quality of alveolar bone and preventing the progression of periodontal disease.




Similar content being viewed by others
References
Ridgeway EE. Periodontal disease: diagnosis and management. J Am Acad Nurse Pract. 2000;12:79–84.
Loesche WJ. Bacterial mediators in periodontal disease. Clin Infect Dis. 1993;16(Suppl 4):S203–10.
Yasuda H, Shima N, Nakagawa N, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci USA. 1998;95:3597–602.
Mogi M, Otogoto J, Ota N, Togari A. Differential expression of RANKL and osteoprotegerin in gingival crevicular fluid of patients with periodontitis. J Dent Res. 2004;83:166–9.
Lu HK, Chen YL, Chang HC, Li CL, Kuo My. Identification of the osteoprotegerin/receptor activator of nuclear factor-kappa B ligand system in gingival crevicular fluid and tissue of patients with chronic periodontitis. J Periodontal Res. 2006;41:354–60.
Vernal R, Chaparro A, Graumann R, Puente J, Valenzuela MA, Gamonal J. Levels of cytokine receptor activator of nuclear factor kappaB ligand in gingival crevicular fluid in untreated chronic periodontitis patients. J Periodontol. 2004;75:1586–91.
Khosla S. Minireview: The OPG/RANKL/RANK system. Endocrinology. 2001;142:5050–5.
Belibasakis GN, Bostanci N. The RANKL-OPG system in clinical periodontology. J Clin Periodontol. 2011. doi:10.1111/j.1600-051X.2011.01810.x.
Kajiya M, Giro G, Taubman MA, Han X, Mayer MP, Kawai T. Role of periodontal pathogenic bacteria in RANKL-mediated bone destruction in periodontal disease. J Oral Mocrobiol 2010; 2. doi:10.3402/jom.v20.5532.
Boyce BF, Xing L. The RANKL/RANK/OPG pathway. Curr Osteoporos Rep. 2007;5:98–104.
Liu D, Xu JK, Figliomeni L, et al. Expression of RANKL and OPG mRNA in periodontal disease: possible involvement in bone destruction. Int J Mol Med. 2003;11:17–21.
Crotti T, Smith MD, Hirsch R, et al. Receptor activator NF kappaB ligand [RANKL) and osteoprotegerin [OPG) protein expression in periodontitis. J Periodontal Res. 2003;38:380–7.
Stehle JH, Saade A, Rawashdeh O, et al. A survey of molecular details in the human pineal gland in the light of phylogeny, structure, function and chronobiological diseases. J Pineal Res. 2011;51:17–43.
Tan DX, Chen LD, Poeggeler B, et al. Melatonin: a potent endogenous hydroxyl radical scavenger. Endocr J. 1993;1:56–60.
Reiter RJ, Tan DX, Manchester LC, Qi W. Biochemical reactivity of melatonin with reactive oxygen and nitrogen species: a review of the evidence. Cell Biochem Biophys. 2001;34:237–56.
Galano A, Tan DX, Reiter RJ. Melatonin as a natural ally against oxidative stress: a physicochemical examination. J Pineal Res. 2011;51:1–16.
Reiter RJ, Calvo JR, Karbownik M, Qi W, Tan DX. Melatonin and its relation to the immune system and inflammation. Ann NY Acad Sci. 2000;917:376–86.
Radogna F, Diederich M, Ghibelli L. Melatonin: a pleiotropic molecule regulating inflammation. Biochem Pharmacol. 2010;80:1844–52.
Cardinali DP, Ladizesky MG, Boggio V, Cutrera RA, Mautalen C. Melatonin effects on bone: experimental facts and clinical perspectives. J Pineal Res. 2003;34:81–7.
Sánchez-Barceló EJ, Mediavilla MD, Tan DX, Reiter RJ. Scientific basis for the potential use of melatonin in bone diseases: osteoporosis and adolescent idiopathic scoliosis. J Osteoporosis. 2010. doi:10.4061/2010/830231.
Park KH, Kang JW, Lee EM, et al. Melatonin promotes osteoblastic differentiation through the BMP/ERK/Wnt signaling pathways. J Pineal Res. 2011;51:187–94.
Zhang L, Su P, Xu C, et al. Melatonin inhibits adipogenesis and enhances osteogenesis of human mesenchymal stem cells by suppressing PPARy expression and enhancing Runx2 expression. J Pineal Res. 2011;49:364–72.
Koyama H, Nakade O, Takada Y, Kaku T, Lau KH. Melatonin at pharmacologic doses increases bone mass by suppressing resorption through down-regulation of the RANKL-mediated osteoclast formation and activation. J Bone Mineral Res. 2002;17:1219–29.
Ostrowska Z, Ziora K, Kos-Kudta B, et al. Melatonin, the RANKL/RANK/OPG system, and bone metabolism in girls with anorexia nervosa. Endokrynol Pol. 2010;61:117–23.
Satomura K, Tobiume S, Tokuyama R, et al. Melatonin at pharmacological doses enhances human osteoblastic differentiation in vitro and promotes mouse cortical bone formation in vivo. J Pineal Res. 2007;42:231–9.
Roth JA, Kim BG, Lin WL, Cho MI. Melatonin promotes osteoblast differentiation and bone formation. J Biol Chem. 1999;274:22041–7.
Gómez-Moreno G, Guardia J, Ferrera MJ, Cutando A, Reiter RJ. Melatonin in diseases of the oral cavity. Oral Dis. 2009. doi:10.1111/j.1601-0825.2009.01610.x.
Blasiak J, Kasznicki J, Drzewoski J, Pawlowska E, Szczepanska J, Reiter RJ. Perspectives on the use of melatonin to reduce cytotoxic and genotoxic effects of methacrylate-based dental materials. J Pineal Res. 2011;51:157–62.
Cutando A, Gómez-Moreno G, Villalba J, Ferrera MJ, Escames G, Acuña-Castroviejo D. Relationship between salivary melatonin levels and periodontal status in diabetic patients. J Pineal Res. 2003;35:239–44.
Miles A, Thomas DR, Grey JE, Pugh AJ. Salivary melatonin assay in laboratory medicine—longitudinal profiles of secretion in healthy men. Clin Chem. 1987;33:1957–9.
Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol. 2001;6:99–112.
Bascones-Martinez A, Matesanz-Perez P, Escribano-Bermejo M, González-Moles MÁ, Bascones-Ilundain J, Meurman JH. Periodontal disease and diabetes—review of the literature. Med Oral Patol Oral Cir Bucal. 2011;16:e722–9.
Mealey BL, Oates TW. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77:1289–303.
World Health Organization. Oral health surveys: basic methods, 4th edition. Geneva: World Health Organization 1987. pp. 31–32.
Shirakawa S, Tsuchiya S, Tsutsumi Y, et al. Time course of saliva and serum melatonin levels after ingestion of melatonin. Psychiatry Clin Neurosci. 1998;52:266–7.
Gómez-Moreno G, Cutando-Soriano A, Arana C, et al. Melatonin expression in periodontal disease. J Periodont Res. 2007;42:536–40.
Cutando A, Galindo P, Gómez-Moreno G, et al. Relationship between salivary melatonin and severity of periodontal disease. J Periodontol. 2006;77:1533–8.
Secchiero P, Corallini F, Pandolfi A, et al. An increased osteoprotegerin serum release characterizes the early onset of diabetes mellitus and may contribute to endothelial cell dysfunction. Am J Pathol. 2006;169:2236–44.
Galluzzi F, Stagi S, Salti R, et al. Osteoprotegerin serum levels in children with type 1 diabetes: a potential modulating role in bone status. Eur J Endocrinol. 2005;153:879–85.
Knudsen ST, Foss CH, Poulsen PL, Andersen NH, Mogensen CE, Rasmussen LM. Increased plasma concentrations of osteoprotegerin in type 2 diabetic patients with microvascular complications. Eur J Endocrinol. 2003;149:39–52.
Anand DV, Lahiri A, Lim E, Hopkins D, Corder R. The relationship between plasma osteoprotegerin levels and coronary artery calcification in uncomplicated type 2 diabetic subjects. J Am Coll Cardiol. 2006;47:1850–7.
Yamaguchi M, Takada R, Kambe S, et al. Evaluation of time-course changes of gingival crevicular fluid glucose levels in diabetics. Biomed Microdevices. 2005;7:53–8.
Silva JA, Lopes Ferrucci D, Peroni LA, et al. Periodontal disease-associated compensatory expression of osteoprotegerin is lost in type 1 diabetes mellitus and correlates with alveolar bone destruction by regulating osteoclastogenesis. Cells Tissues Organs. 2012. doi:10.1159/000330879.
Duarte PM, Neto JB, Casati MZ, Sallum EA, Nociti FH Jr. Diabetes modulates gene expression in the gingival tissues of patients with chronic periodontitis. Oral Dis. 2007;13:594–9.
Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol. 2008;79(8 Suppl 1):1569–76.
Lakschevitz F, Aboodi G, Tenenbaum H, Glogauer M. Diabetes and periodontal diseases: interplay and links. Curr Diabetes Rev. 2011;7:433–9.
Nagorny C, Lyssenko V. Tired of diabetes genetics? Circadian rhythms and diabetes: the MTNR1B story? Curr Diab Rep. 2012;12:667–72.
Acknowledgments
The authors thank Marta Pulido, MD, for editing the manuscript and editorial assistance.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cutando, A., López-Valverde, A., de Diego, R.G. et al. Effect of topical application of melatonin to the gingiva on salivary osteoprotegerin, RANKL and melatonin levels in patients with diabetes and periodontal disease. Odontology 102, 290–296 (2014). https://doi.org/10.1007/s10266-013-0122-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-013-0122-5



