Abstract
Objective
The aim of this study was to observe the demographic and clinical characteristics of immunoglobulin (Ig) G4–related disease (IgG4-RD). We aimed to compare different treatment methods and to identify the risk factors for non-response and relapse after treatment.
Methods
We performed a retrospective study of 201 IgG4-RD patients initially diagnosed and treated at the First Affiliated Hospital of China Medical University from January 2016 to December 2020. Patients’ sex, age, clinical manifestations, baseline biochemical values, the number of organs involved, and the type of organ involvement were recorded. All patients received glucocorticoid (GC) monotherapy or GC + immunosuppressant combination therapy. The serum IgG4 concentration as well as the details of clinical response, relapse, and side effects were recorded at 1, 3, 6, and 12 months after treatment.
Results
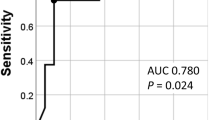
The incidence of IgG4-RD was primarily centered in the age group of 50–70 years old, and the proportion of affected male patients increased with age. The most common clinical symptom was swollen glands or eyes (42.79%). The rates of single- and double-organ involvement were 34.83% and 46.27%, respectively. The pancreas (45.77%) was the most frequently involved organ in cases of single-organ involvement, and the pancreas and biliary tract (45.12%) was the most common organ combination in cases of double-organ involvement. Correlation analysis showed that the number of organs involved was positively related to the serum IgG4 concentration (r = 0.161). The effective rate of GC monotherapy was 91.82%, the recurrence rate was 31.46%, and the incidence of adverse reactions was 36.77%. Meanwhile, the effective rate of GC + immunosuppressant combination therapy was 88.52%, the recurrence rate was 19.61%, and the adverse reaction rate was 41.00%. There were no statistically significant differences in response, recurrence, and adverse reactions. The overall response rate within 12 months was 90.64%. Age (< 50 years old) and aorta involvement were significantly associated with non-response. The overall recurrence rate within 12 months was 26.90%. Age (< 50 years old), low serum C4 concentration, a high number of involved organs, and lymph node involvement were significantly associated with recurrence.
Conclusion
The clinical features vary among different age groups and according to gender. The number of organs involved in IgG4-RD is related to the serum IgG4 concentration. Age (< 50 years old), low serum C4 concentration, a high number of involved organs, and lymph node involvement are risk factors for recurrence.





Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Tarte NN, Ravipati CS, Leondela Rocha JA, Rinker E, Patel NJ. IgG4-related disease with multiorgan involvement: a case-based review. Rheumatol Int. 2021;41(6):1169–74. https://doi.org/10.1007/s00296-021-04848-w.
Liard Y, Nigolian H, Lobrinus JA, et al. ENT and head and neck manifestations of the IgG4-related disease. Rev Med Suisse. 2020;16(709):1870–5.
Cheng Xu, Yongmei H. Immunoglobulin G4-related sclerosing cholangitis mimicking cholangiocarcinoma: a case report and literature review. J Int Med Res. 2020;48(10):300060520959214. https://doi.org/10.1177/0300060520959214.
Floreani A, Okazaki K, Uchida K, Gershwin ME. IgG4-related disease: changing epidemiology and new thoughts on a multisystem disease. J Transl Autoimmun. 2020;4:100074. https://doi.org/10.1016/j.jtauto.2020.100074.
Khosroshahi A, Wallace ZS, Crowe JL, et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015;67(7):1688–99. https://doi.org/10.1002/art.39132.
Lu H, Teng F, Zhang P, et al. Differences in clinical characteristics of IgG4-related disease across age groups: a prospective study of 737 patients. Rheumatology. 2021;60(6):2635–46. https://doi.org/10.1093/rheumatology/keaa651.
Zhang W, Dong LL, Zhu J, et al. Chinese expert consensus on the diagnosis and treatment of IgG 4 related diseases. Zhonghua Nei Ke Za Zhi. 2021;60(3):192–206. https://doi.org/10.3760/cma.j.cn112138-20200803-00726.
Liu Y, Zeng Q, Zhu L, et al. Relapse predictors and serologically unstable condition of IgG4-related disease: a large Chinese cohort. Rheumatology. 2020;59(8):2115–23. https://doi.org/10.1093/rheumatology/kez669.
Bledsoe JR, Della-Torre E, Rovati L, Deshpande V. IgG4-related disease: review of the histopathologic features, differential diagnosis, and therapeutic approach. APMIS. 2018;126(6):459–76. https://doi.org/10.1111/apm.12845.
Wallace ZS, Deshpande V, Mattoo H, et al. IgG4-related disease: clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheum. 2015;67(9):2466–75. https://doi.org/10.1002/art.39205.
Inoue D, Yoshida K, Yoneda N, et al. IgG4-related disease: dataset of 235 consecutive patients. Medicine. 2015;94(15):e680. https://doi.org/10.1097/MD.0000000000000680.
Lin W, Lu S, Chen H, et al. Clinical characteristics of immunoglobulin G4-related disease: a prospective study of 118 Chinese patients. Rheumatology. 2015;54(11):1982–90. https://doi.org/10.1093/rheumatology/kev203.
Tang J, Cai S, Ye C, Dong L. Biomarkers in IgG4-related disease: a systematic review. Semin Arthritis Rheum. 2020;50(2):354–9. https://doi.org/10.1016/j.semarthrit.2019.06.018.
Campochiaro C, Ramirez GA, Bozzolo EP, et al. IgG4-related disease in Italy: clinical features and outcomes of a large cohort of patients. Scand J Rheumatol. 2016;45(2):135–45. https://doi.org/10.3109/03009742.2015.1055796.
Yunyun F, Yu C, Panpan Z, et al. Efficacy of Cyclophosphamide treatment for immunoglobulin G4 related disease with addition of glucocorticoids. Sci Rep. 2017;7(1):6195. https://doi.org/10.1038/s41598-017-06520-5.
Phaopraphat K, Ngamjanyaporn P, Narongroeknawin P, Kasitanon N, Katchamart W. Clinical manifestations, clinical course, and outcomes of immunoglobulin G4-related disease. Int J Rheum Dis. 2020;23(11):1468–73. https://doi.org/10.1111/1756-185X.13949.
Ebbo M, Daniel L, Pavic M, et al. IgG4-related systemic disease: features and treatment response in a French cohort: results of a multicenter registry. Medicine. 2012;91(1):49–56. https://doi.org/10.1097/MD.0b013e3182433d77.
Wallace ZS, Deshpande V, Mattoo H, et al. IgG4-related disease: clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheumatol. 2015;67(9):2466–75. https://doi.org/10.1002/art.39205.
Wang L, Zhang P, Zhang X, Lin W, Tang H, Li J. Sex disparities in clinical characteristics and prognosis of immunoglobulin G4-related disease: a prospective study of 403 patients. Rheumatology. 2019;58(5):820–30. https://doi.org/10.1093/rheumatology/key397.
Liu Y, Xue M, Wang Z, et al. Salivary gland involvement disparities in clinical characteristics of IgG4-related disease: a retrospective study of 428 patients. Rheumatology. 2020;59(3):634–40. https://doi.org/10.1093/rheumatology/kez280.
Zhang P, Han X, Li J, et al. IgG4-related fibrosing mediastinitis: clinical presentation, treatment efficacy and comparison with IgG4-RD without fibrosing mediastinitis. Clin Exp Rheumatol. 2020;38(6):1206–14.
Zeng Q, Gao J, Zhang X, et al. Disparities between IgG4-related kidney disease and extrarenal IgG4-related disease in a case-control study based on 450 patients. Sci Rep. 2021;11(1):10397. https://doi.org/10.1038/s41598-021-89844-7.
Zhao Z, Mou D, Wang Z, et al. Clinical features and relapse risks of IgG4-related ophthalmic disease: a single- center experience in China. Arthritis Res Ther. 2021;23(1):98. https://doi.org/10.1186/s13075-021-02489-9.
Matsumoto H, Fujita Y, Matsuoka N, et al. Serum checkpoint molecules in patients with IgG4-related disease (IgG4-RD). Arthritis Res Ther. 2021;23(1):148. https://doi.org/10.1186/s13075-021-02527-6.
Okazaki K, Kawa S, Kamisawa T, et al. Clinical diagnostic criteria of autoimmune pancreatitis: revised proposal. J Gastroenterol. 2006;41(7):626–31. https://doi.org/10.1007/s00535-006-1868-0.
Maslinska M, Dmowska-Chalaba J, Jakubaszek M. The role of IgG4 in autoimmunity and rheumatic diseases. Front Immunol. 2022;12:787422. https://doi.org/10.3389/fimmu.2021.787422.
Abad S, Martin A, Héran F, et al. IgG4-related disease in patients with idiopathic orbital inflammation syndrome: data from the French SIOI prospective cohort. Acta Ophthalmol. 2019;97(4):e648–56. https://doi.org/10.1111/aos.13968.
Wallace ZS, Deshpande V, Mattoo H, et al. IgG4-related disease: clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheumatol. 2015;67(9):2466–75. https://doi.org/10.1002/art.39205.
Yamada K, Yamamoto M, Saeki T, et al. New clues to the nature of immunoglobulin G4-related disease:a retrospective Japanese multicenter study of baseline clinical features of 334 cases. Arthritis Res Ther. 2017;19(1):262. https://doi.org/10.1186/s13075-017-1467-x.
Hart PA, Kamisawa T, Brugge WR, et al. Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 2013;62(1):771–6.
Yiwen W, Zheng Z, Dai G, et al. Additive effect of leflunomide and glucocorticoids compared with glucocorticoids monotherapy in preventing relapse of IgG4-related disease: a randomized clinical trial. Gut. 2013;62(12):1771–6. https://doi.org/10.1136/gutjnl-2012-303617.
Sekiguchi H, Horie R, Kanai M, Suzuki R, Yi ES, Ryu JH. IgG4-related disease: retrospective analysis of one hundred sixty-six patients. Arthritis Rheumatol. 2016;68(9):2290–9. https://doi.org/10.1002/art.39686.
Miki M, Fujimori N, Oono T, et al. Relapse patterns and predictors of IgG4-related diseases involved with autoimmune pancreatitis: a single-center retrospective study of 115 patients. J Dig Dis. 2019;20(3):152–8. https://doi.org/10.1111/1751-2980.12708.
Peng Y, Li JQ, Zhang PP, et al. Clinical outcomes and predictive relapse factors of IgG4-related disease following treatment: a long-term cohort study. J Intern Med. 2019;286(5):542–52. https://doi.org/10.1111/joim.12942.
Peng L, Lu H, Zhou J, et al. Clinical characteristics and outcome of IgG4-related disease with hypocomplementemia: a prospective cohort study. Arthritis Res Ther. 2021;23(1):102. https://doi.org/10.1186/s13075-021-024.
Acknowledgements
No applicable.
Funding
No applicable.
Author information
Authors and Affiliations
Contributions
YL designed the study; NW, YW, JT and BC collected the data; XZ, XJ, HT, DH, YW and HC organized data; XZ and ZZ wrote the original draft; XZ, YL and LG reviewed and edited; All authors read, revised and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The study was conducted in accordance with Declaration Helsinki. The ethics committee waived the requirement for informed consent because of the retrospective nature of the study. But the protocol was approved by the Ethics Committee of the First Hospital of China Medical University ([2022]20).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Zeng, Z., Tian, H. et al. Clinical features and relapse risks factors of IgG4 related disease: a single-center retrospective study. Clin Exp Med 23, 3527–3538 (2023). https://doi.org/10.1007/s10238-023-01123-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01123-z