Abstract
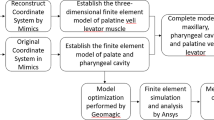
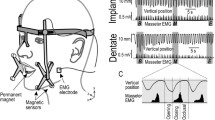
A Hill model-based phenomenological method for muscle activation was used to investigate defectiveness of the palatal muscle tone during sleep for obstructive sleep apnea (OSA) patients. Based on the stretch–stress characteristic of muscle activation when the eccentric contraction is considered, a specifically defined phenomenological strain-energy function was used, as well as the Holzapfel-type strain-energy function for the passive part. A continuum mechanical framework, including the stress tensor and elasticity tensor, was obtained, based on the defined strain-energy function. The model parameters were obtained by fitting the constitutive model to experimental test data. Three-dimensional patient-specific geometry was modeled, accounting for the muscle tissue layer and based on the quantitative histology study of the soft palate. Anatomically representative boundary conditions for the finite element calculation were also considered. Palatal muscle activation level (electromyographic data) versus the negative pressure was defined in the simulations, and the patients’ activation level was set to be lower than for the healthy people. The simulation results showed that reduced in activation level for the patients causes a less negative closing pressure, and this makes the soft palate more prone to collapse. In addition, if we account for the passive–active transfer displayed as the muscle contraction corresponding to the neurogenic reflex in the soft palate, the collapse is prevented. This numerical representation of the reduced activation for the OSA patients may provide increased understanding of OSA physiology.














Similar content being viewed by others
References
Amatoury J, Azarbarzin A, Younes M, Jordan AS, Wellman A, Eckert DJ (2016) Arousal intensity is a distinct pathophysiological trait in obstructive sleep apnea. Sleep 39(12):2091–2100
Berry DA, Moon JB, Kuehn DP (1999) A finite element model of the soft palate. Cleft Palate Craniofacial J 36(3):217–223
Bilston LE, Gandevia SC (2014) Biomechanical properties of the human upper airway and their effect on its behavior during breathing and in obstructive sleep apnea. J Appl Physiol 116(3):314–324
Blemker SS, Pinsky PM, Delp SL (2005) A 3D model of muscle reveals the causes of nonuniform strains in the biceps brachii. J Biomech 38(4):657–665
Brown EC, Cheng S, McKenzie DK, Butler JE, Gandevia SC, Bilston LE (2015) Tongue stiffness is lower in patients with obstructive sleep apnea during wakefulness compared with matched control subjects. Sleep 38(4):537–544
Carberry JC, Jordan AS, White DP, Wellman A, Eckert DJ (2016) Upper airway collapsibility (Pcrit) and pharyngeal dilator muscle activity are sleep stage dependent. Sleep 39(3):511–521
Cheng S, Gandevia SC, Green M, Sinkus R, Bilston LE (2011) Viscoelastic properties of the tongue and soft palate using MR elastography. J Biomech 44(3):450–454
Choi DY, Bae JH, Youn KH, Kim HJ, Hu KS (2014) Anatomical considerations of the longitudinal pharyngeal muscles in relation to their function on the internal surface of pharynx. Dysphagia 29(6):722–730
Deegan PC, McNicholas WT (1995) Pathophysiology of obstructive sleep apnoea. Eur Respir J 8(7):1161–1178
Ehret AE, Böl M, Itskov M (2011) A continuum constitutive model for the active behaviour of skeletal muscle. J Mech Phys Solids 59(3):625–636
Ettema SL, Kuehn DP (1994) A quantitative histologic study of the normal human adult soft palate. J Speech Lang Hear Res 37(2):303–313
Fogel RB, Malhotra A, Pillar G, Edwards JK, Beauregard J, Shea SA, White DP (2001) Genioglossal activation in patients with obstructive sleep apnea versus control subjects: mechanisms of muscle control. Am J Respir Crit Care Med 164(11):2025–2030
Friedman M, Vidyasagar R, Bliznikas D, Joseph NJ (2006) Patient selection and efficacy of pillar implant technique for treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 134(2):187–196
Göktepe S, Menzel A, Kuhl E (2014) The generalized hill model: a kinematic approach towards active muscle contraction. J Mech Phys Solids 72:20–39
Han D, Ye J, Wang Q, Yang J, Lin Y, Wang J (2002) Determining the site of airway obstruction in obstructive sleep apnea with airway pressure measurements during sleep. Laryngoscope 112(11):2081–2085
Hawkins D, Bey M (1994) A comprehensive approach for studying muscle-tendon mechanics. J Biomech Eng 116:51
Hill AV (1938) The heat of shortening and the dynamic constants of muscle. Proc R Soc Lond B Biol Sci 126(843):136–195
Holzapfel GA (2000) Nonlinear solid mechanics. a continuum approach for engineering. Wiley, Chichester
Holzapfel GA, Gasser TC, Ogden RW (2000) A new constitutive framework for arterial wall mechanics and a comparative study of material models. J Elast Phys Sci Solids 61(1):1–48
Huang MH, Lee ST, Rajendran K (1997) Structure of the musculus uvulae: functional and surgical implications of an anatomic study. Cleft Palate Craniofacial J 34(6):466–474
Huang Y, Malhotra A, White DP (2005) Computational simulation of human upper airway collapse using a pressure-/state-dependent model of genioglossal muscle contraction under laminar flow conditions. J Appl Physiol 99(3):1138–1148
Hunter PJ, Nash MP, Sands GB (1997) Computational electromechanics of the heart. Comput Biol Heart 12:347–407
Inouye JM, Pelland CM, Lin KY, Borowitz KC, Blemker SS (2015) A computational model of velopharyngeal closure for simulating cleft palate repair. J Craniofacial Surg 26(3):658–662
Johansson T, Meier P, Blickhan R (2000) A finite-element model for the mechanical analysis of skeletal muscles. J Theor Biol 206(1):131–149
Keenan B, Wang S, Leinwand SE, Pack A, Schwab RJ, Feng Y (2017) Dynamic upper airway characteristics during awake respiration in obese subjects with and without obstructive sleep apnea. Am J Respir Crit Care Med 195:A7269
Kuehn DP, Kahane JC (1990) Histologic study of the normal human adult soft palate. Cleft Palate Craniofacial J 27(1):26–35
Marcucci L, Reggiani C, Natali AN, Pavan PG (2017) From single muscle fiber to whole muscle mechanics: a finite element model of a muscle bundle with fast and slow fibers. Biomech Model Mechanobiol 16(6):1833–1843
McGinley BM, Schwartz AR, Schneider H, Kirkness JP, Smith PL, Patil SP (2008) Upper airway neuromuscular compensation during sleep is defective in obstructive sleep apnea. J Appl Physiol 105(1):197–205
Mezzanotte WS, Tangel DJ, White DP (1992) Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism). J Clin Investig 89(5):1571
Mezzanotte WS, Tangel DJ, White DP (1996) Influence of sleep onset on upper-airway muscle activity in apnea patients versus normal controls. Am J Respir Crit Care Med 153(6):1880–1887
Mortimore IL, Douglas NJ (1997) Palatal muscle emg response to negative pressure in awake sleep apneic and control subjects. Am J Respir Crit Care Med 156(3):867–873
Mortimore IL, Mathur R, Douglas NJ (1995) Effect of posture, route of respiration, and negative pressure on palatal muscle activity in humans. J Appl Physiol 79(2):448–454
Moxness MHS, Wülker F, Skallerud BH, Nordgård S (2018) Simulation of the upper airways in patients with obstructive sleep apnea and nasal obstruction: a novel finite element method. Laryngoscope Investig Otolaryngol 3(2):82–93
Nishino T (2000) Physiological and pathophysiological implications of upper airway reflexes in humans. Jpn J Physiol 50(1):3–14
Odegard GM, Donahue TLH, Morrow DA, Kaufman KR (2008) Constitutive modeling of skeletal muscle tissue with an explicit strain-energy function. J Biomech Eng 130(6):061017
Patil SP, Schneider H, Schwartz AR, Smith PL (2007) Adult obstructive sleep apnea: pathophysiology and diagnosis. Chest 132(1):325–337
Prot V, Skallerud B (2009) Nonlinear solid finite element analysis of mitral valves with heterogeneous leaflet layers. Comput Mech 43(3):353–368
Rachev A, Hayashi K (1999) Theoretical study of the effects of vascular smooth muscle contraction on strain and stress distributions in arteries. Ann Biomed Eng 27(4):459–468
Roux A, Laporte S, Lecompte J, Gras LL, Iordanoff I (2016) Influence of muscle-tendon complex geometrical parameters on modeling passive stretch behavior with the discrete element method. J Biomech 49(2):252–258
Sera T, Uesugi K, Yagi N, Yokota H (2015) Numerical simulation of airflow and microparticle deposition in a synchrotron micro-CT-based pulmonary acinus model. Comput Methods Biomech Biomed Eng 18(13):1427–1435
Skallerud B, Prot V, Nordrum IS (2011) Modeling active muscle contraction in mitral valve leaflets during systole: a first approach. Biomech Model Mechanobiol 10(1):11–26
Sung SJ, Jeong SJ, Yu YS, Hwang CJ, Pae EK (2006) Customized three-dimensional computational fluid dynamics simulation of the upper airway of obstructive sleep apnea. Angle Orthodontist 76(5):791–799
Tang CY, Zhang G, Tsui CP (2009) A 3D skeletal muscle model coupled with active contraction of muscle fibres and hyperelastic behaviour. J Biomech 42(7):865–872
Tangel DJ, Mezzanotte WS, Sandberg EJ, White DP (1992) Influences of NREM sleep on the activity of tonic vs. inspiratory phasic muscles in normal men. J Appl Physiol 73(3):1058–1066
Tangel DJ, Mezzanotte WS, White DP (1995) Influences of NREM sleep on activity of palatoglossus and levator palatini muscles in normal men. J Appl Physiol 78(2):689–695
Vita RD, Grange R, Nardinocchi P, Teresi L (2017) Mathematical model for isometric and isotonic muscle contractions. J Theor Biol 425:1–10
Wang Y, Elghobashi S (2014) On locating the obstruction in the upper airway via numerical simulation. Respir Physiol Neurobiol 193:1–10
White DP (2005) Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med 172(11):1363–1370
Zhao M, Barber T, Cistulli P, Sutherland K, Rosengarten G (2013a) Computational fluid dynamics for the assessment of upper airway response to oral appliance treatment in obstructive sleep apnea. J Biomech 46(1):142–150
Zhao M, Barber T, Cistulli PA, Sutherland K, Rosengarten G (2013b) Simulation of upper airway occlusion without and with mandibular advancement in obstructive sleep apnea using fluid–structure interaction. J Biomech 46(15):2586–2592
Funding
This study was funded in part from a grant from the Research Council of Norway and a grant from NTNU, Norway.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A
Appendix A
The analytical solution for the created constitutive model is achieved in the incompressible case. In the incompressible case, the strain-energy function (7) can be rewritten as
where, p is Lagrange multiplier. The detailed description for the active part reads
with
Note that, since the active part is assumed incompressible, the constant parameters \(\bar{I}_\mathrm {4min}\) and \(\bar{I}_\mathrm {4opt}\) have the same value as \(I_\mathrm {4min}\) and \(I_\mathrm {4opt}\). Then, being similar to Eq. (10) and Eq. (15), the second Piola–Kirchhoff stress in the incompressible case reads
Based on Eq. (16)\(_{1}\) and \(J=1\) for the incompressible case, the Cauchy stress is calculated as
Hence, setting the fiber direction as \(\mathbf {a}_{0}=[1,0,0]\) and defining the deformation gradient for uniaxial test in the fiber direction as
the analytical solution for the uniaxial test can be achieved and fitted with the numerical simulation.
In addition, since \(\mathrm {tr}[\mathbf {a}\otimes \mathbf {a}]=I_{4}=\lambda _{\mathrm {fiber}}^{2}\) (\(\lambda _{\mathrm {fiber}}\) denotes the fiber stretch), the active Cauchy stress in the fiber direction in (39)\(_{3}\) is displayed as
Then, the nominal stress (\(\mathbf {P}=J\mathbf {F}^{-1}\varvec{\sigma }\)) for the fiber activation part is deduced as
With this, for the constitutive parameters, satisfying fitting results to the experimental data used nominal stress can be achieved. This also explains how the added term, \(1/\sqrt{\bar{I}_{4}}\), in Eq. (9) works in the transformation between the nominal stress and Cauchy stress.
Rights and permissions
About this article
Cite this article
Liu, H., Prot, V.E. & Skallerud, B.H. Soft palate muscle activation: a modeling approach for improved understanding of obstructive sleep apnea. Biomech Model Mechanobiol 18, 531–546 (2019). https://doi.org/10.1007/s10237-018-1100-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-018-1100-1