Abstract
Background
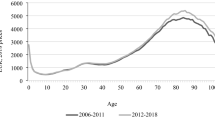
Health care expenditure (HCE) is not distributed evenly over a person’s life course. How much is spent on the elderly is important as they are a population group that is increasing in size. However other factors, such as death-related costs that are known to be high, need be considered as well in any expenditure projections and budget planning decisions.
Objective
This article analyses, for the first time in Scotland, how expenditure projections for acute inpatient care are influenced when applying two different analytical approaches: (1) accounting for healthcare (HC) spending at the end of life and (2) accounting for demographic changes only. The association between socioeconomic status and HC utilisation and costs at the end of life is also estimated.
Methods
A representative, longitudinal data set is used. Survival analysis is employed to allow inclusion of surviving sample members. Cost estimates are derived from a two-part regression model. Future population estimates were obtained for both methods and multiplied separately by cost estimates.
Results
Time to death (TTD), age at death and the interaction between these two have a significant effect on HC costs. As individuals approach death, those living in more deprived areas are less likely to be hospitalised than those individuals living in the more affluent areas, although this does not translate into incurring statistically significant higher costs. Projected HCE for acute inpatient care for the year 2028 was approximately 7 % higher under the demographic approach as compared to a TTD approach.
Conclusion
The analysis showed that if death is postponed into older ages, HCE (and HC budgets) would not increase to the same extent if these factors were ignored. Such factors would be ignored if the population that is in their last year(s) of life were not taken into consideration when obtaining cost estimates.



Similar content being viewed by others

Notes
SMR01 has episode-based patient records that relate to all acute inpatient and day cases. A record is generated when a patient completes an episode of inpatient or day case care and episodes are summarised into ‘Continuous Inpatient Stays’, CIS.
An initial exploration of the data showed that costs increased markedly in the last two quarters of life. Exploratory regression analysis determined when TTD became an insignificant predictor for costs. It was therefore decided to analyse the last 5 years of life, measured in quarters to provide variance for the analysis. Quarters have also been used in previous studies [4, 5].
Since population estimates are only available until 2033 and since it is required for the TTD approach to be able to calculate the proportion of the population in year 1 to 5 before death, the last estimate can be obtained for the year 2028.
References
Payne, G., Laporte, A., Deber, R., Coyte, P.C.: Counting backward to health care’s future: using time-to-death modelling to identify changes in end-of-life morbidity and the impact of aging on health care expenditures. Milbank Q. 85(2), 213–257 (2007)
Zweifel, P., Felder, S., Meiers, M.: Ageing of population and health care expenditure: a red herring? Health Econ. 8(6), 485–496 (1999)
Zweifel, P., Felder, S., Werblow, A.: Population ageing and health care expenditure: new evidence on the ‘red herring’. Geneva Pap. Risk Insur. 29(4), 652–666 (2004)
Seshamani, M., Gray, A.M.: Ageing and health-care expenditure: the red herring argument revisited. Health Econ. 13(4), 303–314 (2004)
Seshamani, M., Gray, A.: Time to death and health expenditure: an improved model for the impact of demographic change on health care costs. Age Ageing 33(6), 556–561 (2004)
Breyer, F., Lorenz, N., Niebel, T.: Health care expenditures and longevity: is there a Eubie Blake effect? Discussion Paper 1226, DIW Berlin (2012)
Moorin, R.E., Holman, C.D.: The cost of in-patient care in Western Australia in the last years of life: a population-based data linkage study. Health Policy 85(3), 380–390 (2008)
Moorin, R., Gibson, D., Holman, D., Hendrie, D.: The contribution of age and time-to-death on health care expenditure for out-of-hospital services. J. Health Serv. Res. Policy 17(4), 197–205 (2012)
McGrail, K., Green, B., Barer, M.L., Evans, R.G., Hertzman, C., Normand, C.: Age, costs of acute and long-term care and proximity to death: evidence for 1987–88 and 1994–95 in British Columbia. Age Ageing 29(3), 249–253 (2000)
Baal, P.H., Wong, A.: Time to death and the forecasting of macro-level healthcare expenditures: some further considerations. J. Health Econ. 31(2012), 876–887 (2012)
Cookson, R., Laudicella, M.: Do the poor cost much more? The relationship between small area income deprivation and length of stay for elective hip replacement in the English NHS from 2001 to 2008. Soc. Sci. Med. 72(2), 173–184 (2011)
WHO World Health Organisation: Health inequality, inequity and social determinants of health. http://www.who.int/social_determinants/resources/interim_statement/csdh_interim_statement_inequity_07.pdf (2007). Accessed Sept 2011
Graham, B., Normand, C.: Proximity to death and acute health care utilisation in Scotland. Final Report, Chief Scientist Office (2001)
Hattersley, L., Boyle, P: The Scottish longitudinal study. An introduction. LSCS working paper 1.0. Edinburgh/St Andrews, Longitudinal Studies Centre Scotland (2007)
Hattersley, L., Raab, G., Boyle, P.: The Scottish longitudinal study. Tracing rates and sample quality for the 1991 census SLS sample. LSCS Working Paper 2.0. Edinburgh/St Andrews: Longitudinal Studies Centre Scotland (2007)
Hattersley, L., Boyle, P.: The Scottish longitudinal study, a technical guide to the creation, quality and linkage of the 2001 census SLS sample. LSCS working paper 3.0. Edinburgh/St Andrews, Longitudinal Studies Centre Scotland (2009)
Hattersley, L., Boyle, P.: The Scottish longitudinal study, The 1991–2001 Scottish longitudinal study census link. LSCS Working paper 4.0. Edinburgh/St Andrews, Longitudinal Studies Centre Scotland (2009)
Geue, C., Lewsey, J., Lorgelly, P., Govan, L., Hart, C., Briggs, A.: Spoilt for choice: implications of using alternative methods of costing hospital episode statistics. Health Econ. 21(10), 1201–1216 (2012)
Cleves, M., Gould, W., Gutierrez, R., Marchenko, Y.: An introduction to survival analysis using STATA, 2nd edn. STATA Press, College Station (2008)
Glick, H.A.: ‘glmdiagnostic.do’. http://www.uphs.upenn.edu/dgimhsr/eeinct_multiv.htm (2008). Accessed Sept 2010
Pregibon, D.: Goodness of link tests for generalized linear models. Appl. Stat. 29, 15 (1980)
Pearson, E.S., Please, N.W.: Relation between the shape of population distribution and the robustness of four simple test statistics. Biometrika 62, 223–241 (1975)
Stearns, S.C., Norton, E.C.: Time to include time to death? The future of health care expenditure predictions. Health Econ. 13(4), 315–327 (2004)
Williams, A.: The rationing debate. Rationing health care by age: the case for. BMJ 314(7083), 820–825 (1997)
Capewell, S., MacIntyre, K., Stewart, S., Chalmers, J.W.T., Boyd, J., Finlayson, A., Redpath, A., Pell, J.P., McMurray, J.J.V.: Age, sex, and social trends in out-of-hospital cardiac deaths in Scotland 1986–95: a retrospective cohort study. Lancet 358, 1213–1217 (2001)
Hakkinen, U., Martikainen, P., Noro, A., Nihtila, E., Peltola, M.: Aging, health expenditure, proximity to death, and income in Finland. Health Econ. Policy Law 3(Pt 2), 165–195 (2008)
Serup-Hansen, N., Wickstroem, J., Kristiansen, I.S.: Future health care costs–do health care costs during the last year of life matter? Health Policy 62(2), 161–172 (2002)
Acknowledgments
The authors would like to thank Fiona Cox, Lee Williamson, Claire Boag and Joan Nolan of the Longitudinal Studies Centre-Scotland (LSCS) for their help provided. The LSCS is supported by the ESRC/JISC, the Scottish Funding Council, the Chief Scientist’s Office and the Scottish Executive. The authors alone are responsible for the interpretation of the data. Census output is Crown copyright and is reproduced with the permission of the Controller of HMSO and the Queen’s Printer for Scotland. This work was supported by a Medical Research Council (MRC) PhD studentship.
Conflict of interest
None.
Ethical standard
Permission was given by the Privacy Advisory Committee of ISD to use linked SMR data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Geue, C., Briggs, A., Lewsey, J. et al. Population ageing and healthcare expenditure projections: new evidence from a time to death approach. Eur J Health Econ 15, 885–896 (2014). https://doi.org/10.1007/s10198-013-0543-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-013-0543-7