Abstract
Introduction
To estimate the costs of palliative care for colorectal cancer (CRC) from the perspective of German statutory health insurance and to measure the patients’ quality of life (QoL) for a 2-year time period.
Methods
A prospective observational multicentre study was carried out to estimate the direct costs of care over a 2-year period. Case report forms, medical records, and claims data were all applied to document medical and resource usage data in real-world settings. QoL was measured by using the Short Form-12 Health Survey.
Results
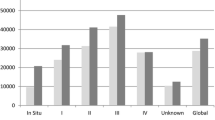
In total 101 patients (mean age 67.09 ± 11.13 years, 68 % male) from 12 different settings were included. The mean costs per patient during the 1st and 2nd years were calculated to be 42,361€ and 32,023€, respectively. Highest mean costs were calculated for the second quarter, which reached an amount of 12,900€ (95 % CI: 11,127€–14,673€). Mean physical summary scores and mean mental summary scores were 41.8 and 49.7, respectively.
Discussion
This is the first study assessing the costs of palliative care and the quality of life of patients with CRC in real-world health-care delivery in Germany. It could be shown that CRC treatment represents an enormous economic burden to the German health-care system. Increased efforts in promoting effective and efficient treatment options, or performance-based medication reimbursement schemes, might be helpful in reducing the costs.
Similar content being viewed by others
References
Robert Koch-Institut: Sterblichkeit, Todesursachen und regionale Unterschiede. Heft 52. Gesundheitsberichtserstattung des Bundes, Berlin (2011)
Robert Koch-Institut: Gesellschaft der epidemiologischen Krebsregister in Deutschland: Krebs in Deutschland 2005/2006: Häufigkeiten und Trends. Gesundheitsberichterstattung des Bundes, Berlin (2010)
Boyle, P., Ferlay, J.: Cancer incidence and mortality in Europe, 2004. Ann. Oncol. 16, 481–488 (2005)
Clerc, L., Jooste, V., Lejeune, C., Schmitt, B., Arveux, P., Quantin, C., Faivre, J., Bouvier, A.M.: Cost of care of colorectal cancers according to health care patterns and stage at diagnosis in France. Eur. J. Health Econom. 9, 361–367 (2008)
Statistisches Bundesamt: Total Cost of Illness in millions of Euro. Classification: years, gender, ICD10, provider (2010)
Jansman, F.G., Postma, M.J., Brouwers, J.R.: Cost considerations in the treatment of colorectal cancer. Pharmacoeconomics 25, 537–562 (2007)
Lopatriello, S., Amoroso, D., Donati, S., Alabiso, O., Forti, L., Fornasiero, A., Smergo, A., Lalli, A., Iacono, C., Lucenti, A., D’Alonzo, L., Negrini, C.: The CAP-CR study: direct medical costs in Italian metastatic colorectal cancer patients on first-line infusional 5-fluorouracil or oral capecitabine. Eur. J. Cancer 44, 2615–2622 (2008)
Com-Ruelle, L., Lucas-Gabrielli, V., Renaud, T.: Le coût du cancer du côlon en Ile-de-France: questions d’économie de la santé. Bulletin d’information en économie de la santé No 98. Institut de recherche et documentation en économie de la santé (2005)
Warren, J., Yabroff, K., Meekins, A., Topor, M., Lamont, E., Brown, M.: Evaluation of trends in the cost of initial cancer treatment. J. Natl Cancer Inst. 100, 888–897 (2008)
Delcò, F., Egger, R., Bauerfeind, P., Beglinger, C.: Hospital health care resource utilization and costs of colorectal cancer during the first 3-year period following diagnosis in Switzerland. Aliment. Pharmacol. Ther. 21, 615–622 (2005)
Choi, K.S., Park, E., Lim, M., Lim, J., Kim, S., Park, J.H., Jeong, S., Park, J.W., Lim, S., Choi, H.S., Jung, K.H., Kim, D.Y., Park, J.: Cost of colorectal cancer care in Korea: a prospective group study with a 2-year follow-up. J. Korean Soc. Coloproctol. 24, 357–366 (2008)
Tilson, L., Sharp, L., Usher, C., Walsh, C., Whyte, S., O’Ceilleachair, A., Stuart, C., Mehigan, B., John Kennedy, M., Tappenden, P., Chilcott, J., Staines, A., Comber, H., Barry, M.: Cost of care for colorectal cancer in Ireland: a health care payer perspective. Eur. J. Health Econom. (2011). doi:10.1007/s10198-011-0325-z
Schmiegel, W., Pox, C., Reinacher-Schick, A., Adler, G., Arnold, D., Fleig, W., Fölsch, U.R., Frühmorgen, P., Graeven, U., Heinemann, V., Hohenberger, W., Holstege, A., Junginger, T., Kopp, I., Kühlbacher, T., Porschen, R., Propping, P., Riemann, J., Rödel, C., Sauer, R., Sauerbruch, T., Schmitt, W., Schmoll, H., Seufferlein, T., Zeitz, M., Selbman, H.: S3 guidelines for colorectal carcinoma: S3-Leitlinie “Kolorektales Karzinom”. Z. Gastroenterol. 48, 65–136 (2010)
Schmiegel, W., Reinacher-Schick, A., Arnold, D., Graeven, U., Heinemann, V., Porschen, R., Riemann, J., Rödel, C., Sauer, R., Wieser, M., Schmitt, W., Schmoll, H., Seufferlein, T., Kopp, I., Pox, C.: Update S3-guideline “Colorectal Cancer” 2008: S3-Leitlinie “Kolorektales Karzinom” Aktualisierung 2008. Z. Gastroenterol. 46, 799–840 (2008)
Lejeune, C., Binquet, C., Bonnetain, F., Mahboubi, A., Abrahamowicz, M., Moreau, T., Raikou, M., Bedenne, L., Quantin, C., Bonithon-Kopp, C.: Estimating the cost related to surveillance of colorectal cancer in a French population. Eur. J. Health Econom. 10, 409–419 (2009)
American Joint Committee on Cancer: Colon and Rectum Cancer Staging. http://www.cancerstaging.org/staging/posters/colon8.5x11.pdf (2009). Accessed 11 Jan 2012
Sobin, L.H., Gospodarowicz, M.K., Wittekind, C.: TNM Classification Of Malignant Tumours. Wiley-Blackwell, Chichester (2009)
American Cancer Society: Colorectal cancer: what is cancer? http://www.cancer.org/acs/groups/cid/documents/webcontent/003096-pdf.pdf (2011). Accessed 11 Jan 2012
Bundesministerium für Gesundheit: Gesetzliche Krankenversicherung: Kennzahlen und Faustformeln (2010)
Kassenärztliche Bundesvereinigung: Einheitlicher Bewertungsmaßstab (EBM): Stand: 4. Quartal 2011. Berlin (2010)
Görner, M., Riemer-Hommel, P.: Adjuvant chemotherapy for colon cancer-analysis of treatment costs from the perspective of statutory sickness funds. Z. Gastroenterol. 46, 681–688 (2008)
InEK—Institut für das Entgeltsystem im Krankenhaus: Fallpauschalen-Katalog 2011: G-DRG-Version 2011. Siegburg (2010)
Müller-Riemenschneider, F., Damm, K., Meinard, C., Bockelbrink, A., Vauth, C., Willich, S., Greiner, G.: Nichmedikamentöse Sekundärprävention der koronaren Herzkrankheit (KHK). HTA-Bericht 95. Deutsche Agentur für Health Technology Assessment, Köln (2009)
Drummond, M., Jefferson, T.O.: Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ 313, 275–283 (1996)
Ware, J.E. Jr., Turner-Bowker, D.M., Gandek, N.K.: User’s manual for the SF-12v2 health survey with a supplement documenting SF-12 health survey. Quality Metric Incorporated, Lincoln, RI (2002)
Bullinger, M., Schmidt, S.: Methoden zur Lebensqualitätsbewertung in der Onkologie. In: Schmoll, HJ., Höffken, K., Possinger, K. (eds.) Kompendium Internistische Onkologie. Standards in Diagnostik und Therapie, pp. 2505–2516. Springer, Heidelberg (2006)
Gandek, B., Ware, J., Aaronson, N., Apolone, G., Bjorner, J., Brazier, J., Bullinger, M., Kaasa, S., Leplege, A., Prieto, L., Sullivan, M.: Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. J. Clin. Epidemiol. 11, 1171–1178 (1998)
Bullinger, M., Kirchberger, I.: SF-36. Fragebogen zum Gesundheitszustand. Handanweisung. Hogrefe, Göttingen (1998)
Dijkers, M.: Correlates of life satisfaction among people with spinal cord injury. Arch. Phys. Med. Rehabil. 8, 867–876 (1999)
Lin, M.R., Hwang, H.F., Chen, C.Y., Chiu, W.T.: Comparisons of the brief form of the World Health Organization Quality of Life and Short Form-36 for persons with spinal cord injuries. Am. J. Phys. Med. Rehabil. 86, 104–113 (2007)
Hill, M.R., Noonan, V.K., Sakakibara, B.M., Miller, W.C.: Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord 48, 438–450 (2010)
Delgado-Sanz, M.C., García-Mendizábal, M.J., Pollán, M., Forjaz, M.J., López-Abente, G., Aragonés, N., Pérez-Gómez, B.: Heath-related quality of life in Spanish breast cancer patients: a systematic review. Health Qual. Life Outcomes. (2011). doi:10.1186/1477-7525-9-3
Grozdev, I., Kast, D., Cao, L., Carlson, D., Pujari, P., Schmotzer, B., Babineau, D., Ker, E., McCormick, T., Cooper, K.D., Korman, N.J.: Physical and mental impact of psoriasis severity as measured by the compact short form-12 health survey (SF-12) Quality of Life Tool. J. Invest. Dermatol. (2011). doi:10.1038/jid.2011.427
Nagel, S.N., Teichgräber, U.K.M., Kausche, S., Lehmann, A.: Satisfaction and quality of life: a survey-based assessment in patients with a totally implantable venous port system. Eur. J. Cancer Care. (2011). doi:10.1111/j.1365-2354.2011.01275.x
Schunk, M., Reitmeir, P., Schipf, S., Völzke, H., Meisinger, C., Thorand, B., Kluttig, A., Greiser, KH., Berger, K., Müller, G., Ellert, U., Heuhauser, H., Tamayo, T., Rathmann, W., Holle, R.: Health-related quality of life in subjects with and without Type 2 diabetes: pooled analysis of five population-based surveys in Germany. Diabetic Med. (2011). doi:10.1111/j.1464-5491.2011.03465.x. (Accepted Article)
Nickel, S., Thiedemann, B., von dem Knesebeck, O.: The effects of integrated inpatient health care on patient satisfaction and health-related quality of life: results of a survey among heart disease patients in Germany. Health Policy 2–3, 156–163 (2010)
König, H., Heider, D., Lehnert, T., Riedel-Heller, S., Angermeyer, C., Matschinger, H., Vilagut, G., Bruffaerts, R., Haro, J., de Girolamo, G., de Graaf, R., Kovess, V., Jordi, A.: Health status of the advanced elderly in six European countries: results from a representative survey using EQ-5D and SF-12. Health Qual. Life Outcomes (2010). doi:10.1186/1477-7525-8-143
Bruns, H., Krätschmer, K., Hinz, U., Brechtel, A., Keller, M., Bücheler, M., Schemmer, P.: Quality of life after curative liver resection: a single center analysis. World J. Gastroenterol. 16, 2388–2395 (2010)
Müller-Nordhorn, J., Roll, S., Willich, S.N.: Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart 90, 523–527 (2004)
Schmidt, A., Bramlage, P., Limberg, R., Kreutz, R.: Quality of life in hypertension management using olmesartan in primary care. Expert Opin. Pharmacother. 9, 1641–1653 (2008)
Müller-Nordhorn, J., Nolte, C., Rossnagel, K., Jungehülsing, G., Reich, A., Roll, S., Villringer, A., Willich, S.: The use of the 12-item short-form health status instrument in a longitudinal study of patients with stroke and ransient ischaemic attack. Neuroepidemiology 24, 196–202 (2005)
Watkins, D.J., Chau, I., Cunningham, D., Mudan, S.S., Karanjia, N., Brown, G., Ashley, S., Norman, A.R., Gillbanks, A.: Defining patient outcomes in stage IV colorectal cancer: a prospective study with baseline stratification according to disease resectability status. Br. J. Cancer 102, 255–261 (2010)
Wein, A., Riedel, C., Brückl, W., Merkel, S., Ott, R., Hanke, B., Baum, U., Fuchs, F., Günther, K., Reck, T., Papadopoulos, T., Hahn, E.G., Hohenberger, W.: Neoadjuvant treatment with weekly high-dose 5-fluorouracil as 24-hour infusion, folinic acid and oxaliplatin in patients with primary resectable liver metastases of colorectal cancer. Oncology 64, 131–138 (2003)
Wein, A., Riedel, C., Köckerling, F., Martus, P., Baum, U., Brueckl, W.M., Reck, T., Ott, R., Hänsler, J., Bernatik, T., Becker, D., Schneider, T., Hohenberger, W., Hahn, E.G.: Impact of surgery on survival in palliative patients with metastatic colorectal cancer after first line treatment with weekly 24-hour infusion of high-dose 5-fluorouracil and folinic acid. Ann. Oncol. 12, 1721–1727 (2001)
Carlson, J.J., Sullivan, S.D., Garrison, L.P., Neumann, P.J., Veenstra, D.L.: Linking payment to health outcomes: a taxonomy and examination of performance-based reimbursement schemes between healthcare payers and manufacturers. Health Policy 96, 179–190 (2010)
van Herck, P., De Smedt, D., Annemans, L., Remmen, R., Rosenthal, M.B., Sermeus, W.: Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv. Res. 10, 247 (2010)
Christianson, J.B., Leatherman, S., Sutherland, K.: Lessons from evaluations of purchaser pay-for-performance programs a review of the evidence. Med. Care Res. Rev. 65, 5S–35S (2008)
Fung, C.H., Lim, Y.W., Mattke, S., Damberg, C., Shekelle, P.G.: Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann. Intern. Med. 148, 111–123 (2008)
Flodgren, G., Eccles, M.P., Shepperd, S., Scott, A., Parmelli, E., Beyer, F.R.: An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst. Rev. 7, CD009255 (2011)
Eijkenaar, F.: Key issues in the design of pay for performance programs. Eur. J. Health Econom. (2011). doi:10.1007/s10198-011-0347-6
Rhoads, K.F., Konety, B.M., Dudley, R.A.: Performance measurement, public reporting, and pay-for-performance. Urol. Clin. North Am. 36, 37–48, vi (2009)
Rosenthal, M.B., Landon, B.E., Howitt, K., Song, H.R., Epstein, A.M.: Climbing up the pay-for-performance learning curve: where are the early adopters now? Health Aff. 26, 1674–1682 (2007)
Emmert, M., Eijkenaar, F., Kemter, H., Esslinger, AS., Schöffski, O.: Economic evaluation of pay-for-performance in health care: a systematic review. Eur. J. Health Econom. (2011). doi:10.1007/s10198-011-0329-8
Wheeler, J.R., White, B., Rauscher, S., Nahre, T.A., Reiter, K.L., Curtin, K.M., Damberg, C.L.: Pay-for-performance as a method to establish the business case for quality. J. Health Care Finance 33, 17–30 (2007)
Acknowledgments
This study was supported by AOK Bayern, Pfizer, Roche, Medac, MerckSerono, and Fresenius.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Emmert, M., Pohl-Dernick, K., Wein, A. et al. Palliative treatment of colorectal cancer in Germany: cost of care and quality of life. Eur J Health Econ 14, 629–638 (2013). https://doi.org/10.1007/s10198-012-0408-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-012-0408-5