Abstract
Background
Milligan–Morgan hemorrhoidectomy (MMH) is the procedure of choice in the management of hemorrhoidal disease. However, this procedure is associated with significant postoperative pain. Tissue selecting technique (TST) is a segmental stapled hemorrhoidopexy, which aims to reduce the postoperative pain, rectovaginal fistula (RVF) and rectal stenosis. The aim of the present study was to compare the clinical outcomes between TST and MMH.
Methods
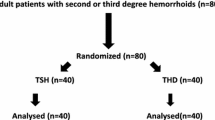
A case–control study was undertaken to investigate the difference in clinical characteristics between the patients treated with TST and those treated with MMH. Intraoperative and postoperative parameters in both groups were collected and compared.
Results
One hundred and ninety-five eligible patients underwent either TST (n = 121) or MMH (n = 74). The pain score was significantly less in the TST group than that in the MMH group at the first defecation and at 12 h, day 3 and day 7 postoperatively (P = 0.001). Further analysis revealed that, at the time point of 12 h, day 3, day 7 and during first defecation, the pain score in the TST group and TST + STE group was less than that in the MMH group (P = 0.001). No patient in either group developed postoperative rectal stenosis. Furthermore, no case of RVF was identified in the TST group. The 1-year recurrence rate was 3.3 % (4/121) and 2.7 % (2/74), respectively, in TST and MMH groups (P = 1.0).
Conclusions
The 1-year recurrence rate after TST and MMH for the treatment of patients with grade III–IV hemorrhoids is similar. It is encouraging that TST is associated with less postoperative pain and no RVF or rectal stenosis.

Similar content being viewed by others
References
Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG (1992) Symptomatic hemorrhoids: current incidence and complications of operative surgery. Dis Colon Rectum 35:477–481
Ho YH, Buettner PG (2007) Open compared with closed hemorrhoidectomy: meta-analysis of randomized controlled trials. Tech Coloproctol 11:135–143
Reese GE, von Roon AC, Tekkis PP (2009) Hemorrhoids: clinical evidence
Pescatori M, Gagliardi G (2008) Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol 12:7–19
Lin HC, Ren DL, He QL et al (2012) Partial stapled hemorrhoidopexy versus circular stapled hemorrhoidopexy for grade III–IV prolapsing hemorrhoids: a two-year prospective controlled study. Tech Coloproctol 16:337–343
Lin HC, He QL, Ren DL et al (2012) Partial stapled hemorrhoidopexy: a minimally invasive technique for hemorrhoids. Surg Today 42:868–875
Lin HC, Lian L, Xie SK, Peng H, Tai JD, Ren DL (2013) The tissue selecting technique: partial stapled hemorrhoidopexy. Dis Colon Rectum 56:1320–1324
Goligher JC (1980) Surgery of the anus rectum and colon, 4th edn. Bailliere Tindall, London, pp 93–149
Milligan ETC, Morgan CN, Nanton LE et al (1937) Surgical anatomy of the anal canal and the operative treatment of hemorrhoids. Lancet 2:111
Gravié JF, Lehur PA, Huten N et al (2005) Stapled hemorrhoidopexy versus Milligan–Morgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg 242:29–35
Kim JS, Vashist YK, Thieltges S et al (2013) Stapled hemorrhoidopexy versus Milligan–Morgan hemorrhoidectomy in circumferential third-degree hemorrhoids: long-term results of a randomized controlled trial. J Gastrointest Surg 17:1292–1298
Fueglistaler P, Guenin MO, Montali I et al (2007) Long-term results after stapled hemorrhoidopexy: high patient satisfaction despite frequent postoperative symptoms. Dis Colon Rectum 50:204–212
Gerjy R, Nyström PO (2007) Excision of residual skin tags during stapled anopexy does not increase postoperative pain. Colorectal Dis 9:754–757
Ganio E, Altomare DF, Milito G, Gabrielli F, Canuti S (2007) Long-term outcome of a multicentre randomized clinical trial of stapled haemorrhoidopexy versus Milligan–Morgan haemorrhoidectomy. Br J Surg 94:1033–1037
Lan P, Wu X, Zhou X, Wang J, Zhang L (2006) The safety and efficacy of stapled hemorrhoidectomy in the treatment of hemorrhoids: a systematic review and meta-analysis of ten randomized control trials. Int J Colorectal Dis 21:172–178
Shao WJ, Li GC, Zhang ZH, Yang BL, Sun GD, Chen YQ (2008) Systematic review and meta-analysis of randomized controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy. Br J Surg 95:147–160
Beattie GC, McAdam TK, McIntosh SA, Loudon MA (2006) Day case stapled haemorrhoidopexy for prolapsing haemorrhoids. Colorectal Dis 8:56–61
Mlakar B, Kosorok P (2003) Complications and results after stapled haemorrhoidopexy as a day surgical procedure. Tech Coloproctol 7:164–168
Corsetti M, De Nardi P, Di Pietro S, Passaretti S, Testoni PA, Staudacher C (2008) Rectal distensibility and symptoms after stapled and Milligan–Morgan operation for hemorrhoids. J Gastrointest Surg 13:2245–2251
Au-Yong I, Rowsell M, Hemingway DM (2004) Randomised controlled clinical trial of stapled haemorrhoidectomy vs conventional haemorrhoidectomy; a three and a half year follow up. Colorectal Dis 6:37–38
Sielezneff I, Salle E, Lécuyer J, Brunet C, Sarles JC, Sastre B (1997) Early postoperative morbidity after hemorrhoidectomy using the Milligan–Morgan technic. A retrospective studies of 1,134 cases. J Chir (Paris) 134:243–247
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lin, HC., Luo, HX., Zbar, A.P. et al. The tissue selecting technique (TST) versus the Milligan–Morgan hemorrhoidectomy for prolapsing hemorrhoids: a retrospective case–control study. Tech Coloproctol 18, 739–744 (2014). https://doi.org/10.1007/s10151-014-1187-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-014-1187-z