Abstract
Introduction
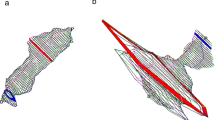
Different trials have investigated the role of conventional anal manometry in the diagnosis of pelvic floor disorders. The aim of the present study is to define the role and the effectiveness of vector anal manometry and vector asymmetry index scoring in the assessment of pelvic floor disorders i.e. fecal incontinence and obstructed defecation.
Methods
Between 2005 and 2007, 387 patients underwent clinical and manometric evaluation in the Department of Surgery, University Hospital Tor Vergata, Rome, Italy, and were included in the present prospective cohort study. All the patients underwent clinical examination, Wexner incontinence scoring, and anal vector manometry and were classified into three groups. Group I included patients with normal resting anal pressure values (195 patients). Groups II and III consisted of patients with resting anal pressure higher and lower than normal values, respectively (90 and 102 patients, respectively). All patients were classified into asymmetric and non-asymmetric according to the vector asymmetry index using a cut-off of 20%. We investigated the correlation between anal asymmetry and pelvic floor disorders, i.e. fecal incontinence due to sphincter injury, rectal prolapse, and obstructed defecation.
Results
In Group III, the number of asymmetric patients was significantly higher than non-asymmetric ones (P < 0.0001). Asymmetry values were significantly higher in group III than in groups I and II considering squeeze (P < 0.0001) or resting pressures (P < 0.0001). Furthermore, there was a statistically significant association between anal asymmetry and both anal incontinence (P < 0.0001) and rectal prolapse (P = 0.0270). No such association was found between anal asymmetry and obstructed defecation.
Conclusion
Anal vector manometry using vector analysis of resting and squeeze pressures is complementary to endoanal ultrasonography, as it provides information on anal sphincter function and integrity. The vector asymmetry index >20% correlates with fecal incontinence due to anal sphincter lesions. Therefore, anal vector manometry may be useful as an independent method of screening for pregnant women at risk of sphincter injury and for patients undergoing anorectal surgery with risk factors for incontinence, like previous anorectal surgery or a history of two or more previous vaginal deliveries.







Similar content being viewed by others
References
Perry RE, Blatchford GJ, Christensen MA, Thorson AG, Attwood SEA (1990) Manometric diagnosis of anal sphincter injuries. Am J Surg 159:112–117
Fynes MM, Behan M, O’Herlihy C, O’Connell PR (2000) Anal vector volume analysis complements endoanal ultrasonographic assessment of postpartum anal sphincter injury. Br J Surg 87:1209–1214
Williams N, Barlow J, Hobson A, Scott N, Irving M (1995) Manometric asymmetry in the anal canal in controls and patients with fecal incontinence. Dis Colon Rectum 38:1275–1280
Jorge A, Habr Gama A (2000) The value of sphincter asymmetry index in anal incontinence. Int J Colorectal Dis 15:303–310
Braun JC, Treutner KH, Dreuw B, Klimaszewski M, Schumpelick V (1994) Vectormanometry for differential diagnosis of fecal incontinence. Dis Colon Rectum 37:989–996
Samarasekera DN, Wright Y, Lowndes RH, Stanley KP, Preston P, Speakman CTM (2008) Comparison of vector symmetry index and endoanal ultrasonography in the diagnosis of anal sphincter disruption. Tech Coloproctol 12:211–215
Gundling F, Seidl H, Scalercio N, Schmidt T, Schepp W, Pehl C (2010) Influence of gender and age on anorectal function: normal values from anorectalm manometry in a large caucasian population. Digestion 81:207–213
Azpiroz F, Enck P, Whitehead WE (2002) Anorectal functional testing: review of collective experience. Am J Gastroenterol 97:232–240
Lestar B, Penninckx F, Kerremans R (1989) The composition of anal basal pressure. An in vitro study in man. Int J Colorect Dis 4:118–122
Sentovich SM, Blatchford GJ, Rivela LJ, Lin K, Thorson AG, Christensen MA (1997) Diagnosing anal sphincter injury with transanal ultrasound and manometry. Dis Colon Rectum 40:1430–1434
Cali RL, Blatchford GJ, Perry RE, Pitsch RM, Thorson AG, Christensen MA (1992) Normal variation in anorectal manometry. Dis Colon Rectum 35:1161–1164
Lindsey I, Jones OM, Smilgin-Humpreys MM, Cunningham C, Mortensen NJ (2004) Patterns of fecal incontinence after anal surgery. Dis Colon Rectum 47:1643–1649
Sultan AH, Kamm MA, Nicholls RJ, Batram CI (1994) Prospective study of the extent of internal anal sphincter division during lateral sphincterotomy. Dis Colon Rectum 37:1031–1033
Corby H, Donnelly VS, O’Herlihy C, O’Connell PR (1997) Anal canal pressures are low in women with postpartum anal fissure. Br J Surg 84:86–88
Liu J, Guaderrama N, Nager CW, Pretorius DH, Master S, Mittal RK (2006) Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am J Gastroenterol 101:1092–1097
Abcarian H (1980) Surgical correction of chronic anal fissure: results of lateral internal sphincterotomy vs fissurectomy-midline sphincterotomy. Dis Colon Rectum 23:31–36
Ferrara A, Lujan JH, Cebrian J et al (2001) Clinical, manometric, and EMG characteristics of patients with fecal incontinence. Tech Coloproctol 5:13–18
Floyd WF, Walls EW (1953) Electromyography of the sphincter ani externus in man. J Physiol 122:599–609
Damon H, Henry L, Roman S, Barth X, Mion F (2003) Influence of rectal prolapse on the asymmetry of the anal sphincter in patients with anal incontinence. BMC Gastroenterol 3:23
Gammarota FV, Farouk R, Duthie GS, Bartolo DC (1992) The functional recovery of the internal anal sphincter and the restoration of continence after rectopexy for rectal prolapse. G Chir 13:527–531
Birnbaum EH, Stamm L, Rafferty JF, Fry RD, Kodner IJ, Fleshman JW (1996) Pudendal nerve terminal motor latency influences surgical outcome in treatment of rectal prolapse. Dis Colon Rectum 39:1215–1221
Zbar AP, Beer-Gabel M, Chiappa AC, Aslam M (2001) Fecal incontinence after minor anorectal surgery. Dis Colon Rectum 44:1610–1619 (Discussion 1619–1623)
Zbar AP, Kmiot WA, Aslam M et al (1999) Use of vector volume manometry and endoanal magnetic resonance imaging in the adult female for assessment of anal sphincter dysfunction. Dis Colon Rectum 42:1411–1418
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grande, M., Cadeddu, F., Sileri, P. et al. Anal vector volume analysis: an effective tool in the management of pelvic floor disorders. Tech Coloproctol 15, 31–37 (2011). https://doi.org/10.1007/s10151-010-0658-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-010-0658-0