Abstract
Background
Anatomic anal sphincter defects can involve the internal anal sphincter (IAS), the external anal sphincter (EAS), or both muscles. Surgical repair of anteriorly located EAS defects consists of overlapping suture of the EAS or EAS imbrication; IAS imbrication can be added regardless of whether there is IAS injury. The aim of this study was to assess the functional outcome of anal sphincter repair in patients intraoperatively diagnosed with combined EAS/IAS defects compared to patients with isolated EAS defects.
Methods
The medical records of patients who underwent anal sphincter repair between 1988 and 2000 and had follow-up of at least 3 months were retrospectively assessed. Fecal incontinence was assessed using the Cleveland Clinic Florida incontinence score wherein 0 equals perfect continence and 20 is associated with complete incontinence. Postoperative scores of 0–10 were interpreted as success whereas scores of 11–20 indicated failure.
Results
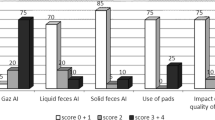
A total of 131 women were included in this study, including 38 with combined EAS/IAS defects (Group I) and 93 with isolated EAS defects (Group II). Thirty-three patients (87%) in Group I had imbrication of a deficient IAS, compared to 83 patients (89%) in Group II. All patients had either overlapping EAS repair (n=121) or EAS imbrication (n=10). Mean follow-up was 30.9 months (range, 3–131 months). There were no statistically significant differences between the two groups relative to age (48.3 vs. 53.0 years; p=0.14), preoperative incontinence score (16.1 vs. 16.7; p=0.38), extent of pudendal nerve terminal motor latency pathology (left, 11.1% vs. 8%; p=0.58; right, 8.6% vs. 15.1%; p=0.84), extent of pathology at electromyography (54.8% vs. 60.1%; p=0.43), and length of follow-up (26.9 vs. 32.5 months; p=0.31). The success rates of sphincter repair were 68.4% for Group I versus 55.9% for Group II (p=NS). Both groups were well matched for incidence of IAS imbrication as well as age, follow-up interval, and physiologic parameters. The success rates of anal sphincter repair were not statistically significant between the two groups.
Conclusion
A pre-existing IAS defect does not preclude successful sphincteroplasty as compared to repair of an isolated EAS defect. Thus, patients with combined anal sphincter defects should not be considered as poor candidates for sphincter repair.
Similar content being viewed by others
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the annual meeting of the Association of Coloproctology of Great Britain and Ireland, 2–5 July 2002, Manchester, UK.
Rights and permissions
About this article
Cite this article
Oberwalder, M., Dinnewitzer, A., Baig, M.K. et al. Do internal anal sphincter defects decrease the success rate of anal sphincter repair?. Tech Coloproctol 10, 94–97 (2006). https://doi.org/10.1007/s10151-006-0259-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-006-0259-0