Abstract
Purpose
To conduct a systematic review and meta-analysis of publications to evaluate the analgesic efficacy and safety of percutaneous thermal ablation (PTA) plus percutaneous cementoplasty (PCP) (PTA + PCP) for painful bone metastases.
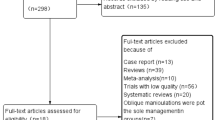
Methods
We searched PubMed, Cochrane Library and Embase for articles published up to October 2022. Outcomes were a 10-point pain scale, morphine equivalents daily dose (MEDD) and complications. A subgroup confined to spinal bone metastases was analyzed.
Results
Twenty-one articles were selected for the analysis. The 21 selected articles involved a total of 661 cases. The pooled pain scales at pre-PTA + PCP, 1 day, 1 week and 1-, 3-, and 6 months post-PTA + PCP were 7.60 (95% confidence interval [CI], 7.26–7.95, I2 = 89%), 3.30 (95% CI, 2.25–4.82, I2 = 98%), 2.58 (95% CI, 1.99–3.35, I2 = 94%), 2.02 (95% CI, 1.50–2.71, I2 = 93%), 1.78 (95% CI, 1.26–2.53, I2 = 95%), and 1.62 (95% CI, 1.14–2.31, I2 = 88%), and in the subgroup, 7.97 (95% CI, 7.45–8.52, I2 = 86%), 3.01 (95% CI, 1.43–6.33, I2 = 98%), 2.95 (95% CI, 1.93–4.51, I2 = 95%), 2.34 (95% CI, 1.82–3.01, I2 = 68%), 2.18 (95% CI, 1.57–3.03, I2 = 78%), and 2.01 (95% CI, 1.16–3.48, I2 = 86%). Mean MEDD decreased up to 3 months post-PTA + PCP in 4 articles. The overall pooled major complication rate was 4% (95% CI, 2–6%, I2 = 2%).
Conclusions
The updated systematic review and meta-analysis indicates that PTA + PCP for painful bone metastases is safe, and can lead to rapid and sustained pain reduction.








Similar content being viewed by others
References
Cetin K, Christiansen CF, Jacobsen JB et al (2014) Bone metastasis, skeletal-related events, and mortality in lung cancer patients: a Danish population-based cohort study. Lung Cancer 86:247–254
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12:6243s–6249s
Kelly PD, Zuckerman SL, Than KD et al (2019) Metastatic spine disease in lung cancer patients: national patterns of radiation and surgical care. J Spine Surg 5:320–328
Soeharno H, Povegliano L, Choong PF (2018) Multimodal treatment of bone metastasis-a surgical perspective. Front Endocrinol (Lausanne) 9:518
Gdowski AS, Ranjan A, Vishwanatha JK (2017) Current concepts in bone metastasis, contemporary therapeutic strategies and ongoing clinical trials. J Exp Clin Cancer Res 36:108
Tomasian A, Jennings JW (2019) Percutaneous minimally invasive thermal ablation for management of osseous metastases: recent advances. Int J Hyperthermia 36:3–12
Saliou G, el Kocheida M, Lehmann P et al (2010) Percutaneous vertebroplasty for pain management in malignant fractures of the spine with epidural involvement. Radiology 254:882–890
Anselmetti GC, Manca A, Ortega C et al (2008) Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol 31:1165–1173
Network NCC (2023) NCCN clinical practice guidelines in oncology (NCCN Guidelines®): adult cancer pain [v. 1.2023]. Accessed on 10 June 2023
Alexander ES, Hankins CA, Machan JT et al (2013) Rib fractures after percutaneous radiofrequency and microwave ablation of lung tumors: incidence and relevance. Radiology 266:971–978
Jiao D, Yao Y, Li Z et al (2022) Simultaneous c-arm computed tomography-guided microwave ablation and cementoplasty in patients with painful osteolytic bone metastases: a single-center experience. Acad Radiol 29:42–50
Pusceddu C, De Francesco D, Melis L et al (2021) The role of a navigational radiofrequency ablation device and concurrent vertebral augmentation for treatment of difficult-to-reach spinal metastases. Curr Oncol 28:4004–4015
Wallace AN, Huang AJ, Vaswani D et al (2016) Combination acetabular radiofrequency ablation and cementoplasty using a navigational radiofrequency ablation device and ultrahigh viscosity cement: technical note. Skeletal Radiol 45:401–405
Masala S, Chiocchi M, Taglieri A et al (2013) Combined use of percutaneous cryoablation and vertebroplasty with 3D rotational angiograph in treatment of single vertebral metastasis: comparison with vertebroplasty. Neuroradiology 55:193–200
Sun Y, Zhang H, Xu HR et al (2019) Analgesia of percutaneous thermal ablation plus cementoplasty for cancer bone metastases. J Bone Oncol 19:100266
Tian QH, Han K, Wang T et al (2022) Percutaneous sacroplasty with or without radiofrequency ablation for treatment of painful sacral metastases. AJNR Am J Neuroradiol 43:1222–1227
Senol N, Oguzoglu AS, Goksel HM (2022) Radiofrequency ablation and augmentation in the management of spinal metastases: clinical experience in 41 patients. World Neurosurg 163:e420–e425
Pusceddu C, De Francesco D, Ballicu N et al (2022) Safety and feasibility of steerable radiofrequency ablation in combination with cementoplasty for the treatment of large extraspinal bone metastases. Curr Oncol 29:5891–5900
Hu TY, Zhang G, Ye H et al (2022) Pain relief and safety of microwave ablation combined with percutaneous vertebroplasty for vertebral metastasis: a pilot study. J Neurol Surg A Cent Eur Neurosurg. https://doi.org/10.1055/s-0042-1758121
Zhang X, Ye X, Zhang K et al (2021) Computed tomography-guided microwave ablation combined with osteoplasty for the treatment of bone metastases: a multicenter clinical study. J Vasc Interv Radiol 32:861–868
Kastler A, Barbé DA, Alemann G et al (2021) Bipolar radiofrequency ablation of painful spinal bone metastases performed under local anesthesia: feasibility regarding patient’s experience and pain outcome. Medicina (Kaunas) 57:966
He Y, Han S, Wu C et al (2021) Comparison of the postoperative pain change and spinal stenosis rate between percutaneous vertebroplasty combined with radiofrequency ablation and with (125)I particle implantation in the treatment of metastatic spinal cord compression: a retrospective study. J Interv Med 4:197–202
Yan T, Zhao Z, Tang X et al (2019) Improving functional outcome and quality of life for patients with metastatic lesion of acetabulum undergoing cement augmentation. Medicine (Baltimore) 98:e17029
Filippiadis DK, Binkert C, Pellerin O et al (2017) Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol 40:1141–1146
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Kim SY, Park JE, Lee YJ et al (2013) Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol 66:408–414
Zhao W, Wang H, Hu JH et al (2018) Palliative pain relief and safety of percutaneous radiofrequency ablation combined with cement injection for bone metastasis. Jpn J Clin Oncol 48:753–759
Reyes M, Georgy M, Brook L et al (2018) Multicenter clinical and imaging evaluation of targeted radiofrequency ablation (t-RFA) and cement augmentation of neoplastic vertebral lesions. J Neurointerv Surg 10:176–182
Fares A, Shaaban MH, Reyad RM et al (2018) Combined percutaneous radiofrequency ablation and cementoplasty for the treatment of extraspinal painful bone metastases: a prospective study. J Egypt Natl Canc Inst 30:117–122
Pusceddu C, Sotgia B, Fele RM et al (2016) Combined microwave ablation and cementoplasty in patients with painful bone metastases at high risk of fracture. Cardiovasc Intervent Radiol 39:74–80
Wei Z, Zhang K, Ye X et al (2015) Computed tomography-guided percutaneous microwave ablation combined with osteoplasty for palliative treatment of painful extraspinal bone metastases from lung cancer. Skeletal Radiol 44:1485–1490
Tian QH, Wu CG, Gu YF et al (2014) Combination radiofrequency ablation and percutaneous osteoplasty for palliative treatment of painful extraspinal bone metastasis: a single-center experience. J Vasc Interv Radiol 25:1094–1100
Clarençon F, Jean B, Pham HP et al (2013) Value of percutaneous radiofrequency ablation with or without percutaneous vertebroplasty for pain relief and functional recovery in painful bone metastases. Skeletal Radiol 42:25–36
Masala S, Guglielmi G, Petrella MC et al (2011) Percutaneous ablative treatment of metastatic bone tumours: visual analogue scale scores in a short-term series. Singapore Med J 52:182–189
Munk PL, Rashid F, Heran MK et al (2009) Combined cementoplasty and radiofrequency ablation in the treatment of painful neoplastic lesions of bone. J Vasc Interv Radiol 20:903–911
van der Linden E, Kroft LJM, Dijkstra PDS (2007) Treatment of vertebral tumor with posterior wall defect using image-guided radiofrequency ablation combined with vertebroplasty: preliminary results in 12 patients. J Vasc Interv Radiol 18:741–747
Hoffmann RT, Jakobs TF, Trumm C et al (2008) Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J Vasc Interv Radiol 19:419–425
Dupuy DE, Liu D, Hartfeil D et al (2010) Percutaneous radiofrequency ablation of painful osseous metastases: a multicenter American college of radiology imaging network trial. Cancer 116:989–997
Baerlocher MO, Nikolic B, Sze DY (2023) Adverse event classification: clarification and validation of the society of interventional radiology specialty-specific system. J Vasc Interv Radiol 34:1–3
Higgins J, Altman D, Sterne J (2011) Assessing risk of bias in included studies. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1. 0 (updated March 2011) the cochrane collaboration, 2011. Wiley, pp 243–296 (Available from handbook cochrane org)
Hadjipavlou AG, Tzermiadianos MN, Katonis PG et al (2005) Percutaneous vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures and osteolytic tumours. J Bone Joint Surg Br 87:1595–1604
Yildizhan S, Boyaci MG, Rakip U et al (2021) Role of radiofrequency ablation and cement injection for pain control in patients with spinal metastasis. BMC Musculoskelet Disord 22:912
Orgera G, Krokidis M, Matteoli M et al (2014) Percutaneous vertebroplasty for pain management in patients with multiple myeloma: is radiofrequency ablation necessary? Cardiovasc Intervent Radiol 37:203–210
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Tomohiro Matsumoto, Marina Osaki, Junki Shibata and Rika Yoshimatsu. The first draft of the manuscript was written by Tomohiro Matsumoto and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no financial interests.
Ethics approval and consent to participate
Not applicable. This study did not involve human participants.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original publication has been updated for inclusion of Electronic Supplementary Material.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Matsumoto, T., Yoshimatsu, R., Osaki, M. et al. Analgesic efficacy and safety of percutaneous thermal ablation plus cementoplasty for painful bone metastases: a systematic review and meta-analysis. Int J Clin Oncol 29, 372–385 (2024). https://doi.org/10.1007/s10147-023-02458-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02458-z