Abstract
Objective
The objective of the study is to identify the risk factors associated with recurrent/persistent disease and cervical stenosis after conization.
Methods
Five hundred twenty-two (522) cases of high-grade intraepithelial lesions treated by conization were retrospectively reviewed. Risk factors associated with recurrent/persistent disease were analyzed by univariate and multivariate analysis using a Cox hazard regression model. Factors that could potentially affect the risk of cervical stenosis were examined by univariate and by multivariate analysis using the χ 2 test and logistic regression, respectively.
Results
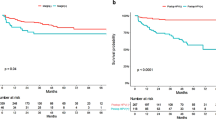
Recurrent/persistent diseases and cervical stenosis occurred in 4.8% and 5.4% of the patients, respectively. Age ≥46 years [hazard ratio (HR) 3.6, 95% CI 1.36–10.3, p = 0.0092] and surgical margin involvement (HR 13.44, 95% CI 5.07–46.37, p < 0.001) were independent predictors for recurrent/persistent diseases. Age ≥46 years [odds ratio (OR) 4.27, 95% CI 1.88–10.07, p < 0.001] and shortened interval after childbirth to conization (within 12 months) (OR 5.42, 95% CI 1.42–17.41, p = 0.016) were independent risk factors for cervical stenosis.
Conclusion
Elderly patients (aged ≥46 years) are at high risk of recurrence and cervical stenosis, which may lead to unsatisfactory follow-up. Subsequent hysterectomy is beneficial to patients aged 46 or older with surgical margin involvement. Clinicians should recognize the possibility of cervical stenosis after conization during the breastfeeding period, leading to secondary infertility or hematometra.



Similar content being viewed by others
References
Ostor AG (1993) Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol 12:186–192
Martin-Hirsch PP, Paraskevaidis E, Bryant A et al (2013) Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev. doi:10.1002/14651858.CD001318.pub2
Matsumura M, Ota T, Takeshima N et al (2010) Shimodaira–Taniguchi conization method: its utility and reliability. Int J Gynecol Cancer 20:1025–1030
Miyoshi Y, Miyatake T, Ueda Y et al (2012) Prediction, based on resection margins, of long-term outcome of cervical intraepithelial neoplasia 3 treated by Shimodaira–Taniguchi conization. Arch Gynecol Obstet 285:1427–1432
Santesso N, Mustafa RA, Wiercioch W et al (2016) Systematic reviews and meta-analyses of benefits and harms of cryotherapy, LEEP, and cold knife conization to treat cervical intraepithelial neoplasia. Int J Gynaecol Obstet 132:266–271
Kitchener HC, Walker PG, Nelson L et al (2008) HPV testing as an adjunct to cytology in the follow up of women treated for cervical intraepithelial neoplasia. Br J Obstet Gynecol 115:1001–1007
Park JY, Lee KH, Dong SM et al (2008) The association of pre-conization high-risk HPV load and the persistence of HPV infection and persistence/recurrence of cervical intraepithelial neoplasia after conization. Gynecol Oncol 108:549–554
Kang WD, Oh MJ, Kim SM et al (2010) Significance of human papillomavirus genotyping with high-grade cervical intraepithelial neoplasia treated by a loop electrosurgical excision procedure. Am J Obstet Gynecol 203(72):e1–e6
Penna C, Fambrini M, Fallani MG et al (2005) Laser CO2 conization in postmenopausal age: risk of cervical stenosis and unsatisfactory follow-up. Gynecol Oncol 96:771–775
Bornstein J, Bentley J, Bosze P et al (2012) 2011 Colposcopic terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol 120:166–172
Hiramatsu K, Ueda Y, Yoshino K et al (2013) Conization using the Shimodaira–Taniguchi procedure for adenocarcinoma in situ of the uterine cervix. Eur J Obstet Gynecol Reprod Biol 168:218–221
Solomon D, Davey D, Kurman R et al (2002) The 2001 Bethesda system: terminology for reporting results of cervical cytology. JAMA 287:2114–2119
Kudoh A, Sato S, Itamochi H et al (2016) Human papillomavirus type-specific persistence and reappearance after successful conization in patients with cervical intraepithelial neoplasia. Int J Clin Oncol 21:580–587
Vintermyr OK, Iversen O, Thoresen S et al (2014) Recurrent high-grade cervical lesion after primary conization is associated with persistent human papillomavirus infection in Norway. Gynecol Oncol 33:159–166
Zhu M, He Y, Baak JP et al (2015) Factors that influence persistence or recurrence of high-grade squamous intraepithelial lesion with positive margins after the loop electrosurgical excision procedure: a retrospective study. BMC Cancer 15:744
Ghaem-Maghami S, Sagi S, Majeed G et al (2007) Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol 8:985–993
Houlard S, Perrotin F, Fourquet F et al (2002) Risk factors for cervical stenosis after laser cone biopsy. Eur J Obstet Gynecol Reprod Biol 104:144–147
Baldauf JJ, Dreyfus M, Ritter J et al (1996) Risk of cervical stenosis after large loop excision or laser conization. Obstet Gynecol 88:933–938
Xiang L, Li J, Yang W et al (2015) Conization using an electrosurgical knife for cervical intraepithelial neoplasia and microinvasive carcinoma. PLoS One 10:e0131790
Grund D, Kohler C, Krauel H et al (2007) A new approach to preserve fertility by using a coated nitinol stent in a patient with recurrent cervical stenosis. Fertil Steril 87(1212):e13–e16
Koyama S, Kobayashi M, Tanaka Y et al (2014) Complete cervical stenosis after conization: timing for the minimally invasive reconstructive surgery. Gynecol Minim Invasive Ther 3:57–60
Nasu K, Narahara H (2010) Management of severe cervical stenosis after conization by detention of nylon threads tied up to intrauterine contraceptive device. Arch Gynecol Obstet 281:887–889
Acknowledgements
We thank Dr. G.S. Buzard for his constructive critique and editing of our manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
About this article
Cite this article
Tanaka, Y., Ueda, Y., Kakuda, M. et al. Predictors for recurrent/persistent high-grade intraepithelial lesions and cervical stenosis after therapeutic conization: a retrospective analysis of 522 cases. Int J Clin Oncol 22, 921–926 (2017). https://doi.org/10.1007/s10147-017-1124-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1124-z