Abstract
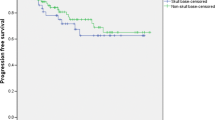
To identify differences between skull base meningiomas (SBM) and non-skull base meningiomas (NSBM). All adult patients (18.0–69.9 years) operated for intracranial meningiomas between 1990 and 2010 at our institution were investigated. Al-Mefty’s definition was used to dichotomize tumors into SBM and NSBM. Overall, 1148 consecutive patients were identified. Median age at surgery was 54.2 years [18.1–69.9]. Median follow-up was 7.4 years [0.0–20.9]. There were 562 patients (49%) with SBM and 586 (51%) with NSBM. The two groups were similar with respect to patient age, follow-up time, and number of patients. Overall female-to-male ratio was 2.6:1, but 3.2:1 in SBM and 2.2:1 in NSBM (p < 0.005). With respect to presenting symptoms, SBMs had more often neurological deficits (risk ratio (RR) 1.4; p < 0.0001) and less often seizures (RR 0.4; p < 0.0001). Gross total resections were less frequent in SBM than NSBM (62 vs 84%) (RR 1.3; p < 0.0001). SBMs had a lower risk of WHO grades II and III histology (4.5 vs 9.5%) (RR 0.5; p < 0.001). Worsening of neurological function was more frequent in SBM (21 vs 121%) (RR 1.8; p < 0.001). Retreatment-free survival at 5, 10, and 15 years, respectively, was 80, 70, and 62% for SBM versus 90, 82, and 74% for NSBM (p < 0.0001). Overall survival at 5, 10, and 15 years, respectively, was 93, 85, and 78% for SBM and 96, 91, and 79% for NSBM (p = 0.14). Patients with SBMs had more new-onset neurological deficits and significantly shorter retreatment-free survivals, but this did not adversely affect the overall survival.


Similar content being viewed by others
References
Adegbite AB, Khan MI, Paine KW, Tan LK (1983) The recurrence of intracranial meningiomas after surgical treatment. J Neurosurg 58:51–56. https://doi.org/10.3171/jns.1983.58.1.0051
Asano K, Nakano T, Takeda T, Ohkuma H (2009) Risk factors for postoperative systemic complications in elderly patients with brain tumors. Clinical article. J Neurosurg 111:258–264. https://doi.org/10.3171/2008.10.17669
Beks JW, de Windt HL (1988) The recurrence of supratentorial meningiomas after surgery. Acta Neurochir 95:3–5. https://doi.org/10.1007/BF01793074
Bir SC, Konar SK, Maiti TK, Thakur JD, Guthikonda B, Nanda A (2016) Utility of neuronavigation in intracranial meningioma resection: a single-center retrospective study. World Neurosurg 90:546–555.e541. https://doi.org/10.1016/j.wneu.2015.12.101
Black PM, Morokoff AP, Zauberman J (2008) Surgery for extra-axial tumors of the cerebral convexity and midline. Neurosurgery 62:1115–1121; discussion 1121-1113. https://doi.org/10.1227/01.neu.0000333778.66316.38
Boviatsis EJ, Bouras TI, Kouyialis AT, Themistocleous MS, Sakas DE (2007) Impact of age on complications and outcome in meningioma surgery. Surg Neurol 68:407–411; discussion 411. https://doi.org/10.1016/j.surneu.2006.11.071
Chaichana KL, Pendleton C, Zaidi H, Olivi A, Weingart JD, Gallia GL, Lim M, Brem H, Quinones-Hinojosa A (2012) Seizure control for patients undergoing meningioma surgery. World Neurosurg 79:515–524. https://doi.org/10.1016/j.wneu.2012.02.051
Chan RC, Thompson GB (1984) Morbidity, mortality, and quality of life following surgery for intracranial meningiomas. A retrospective study in 257 cases. J Neurosurg 60:52–60. https://doi.org/10.3171/jns.1984.60.1.0052
Chen CM, Huang AP, Kuo LT, Tu YK (2011) Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34:281–296; discussion 296. https://doi.org/10.1007/s10143-011-0321-x
Chen WC, Magill ST, Englot DJ, Baal JD, Wagle S, Rick JW, McDermott MW (2017) Factors associated with pre- and postoperative seizures in 1033 patients undergoing supratentorial meningioma resection. Neurosurgery 81:297–306. https://doi.org/10.1093/neuros/nyx001
Cohen-Inbar O, Lee CC, Schlesinger D, Xu Z, Sheehan JP (2015) Long-term results of stereotactic radiosurgery for skull base meningiomas. Neurosurgery 79:58–68. https://doi.org/10.1227/neu.0000000000001045
Curry WT, McDermott MW, Carter BS, Barker FG 2nd (2005) Craniotomy for meningioma in the United States between 1988 and 2000: decreasing rate of mortality and the effect of provider caseload. J Neurosurg 102:977–986. https://doi.org/10.3171/jns.2005.102.6.0977
D’Amico RS, Banu MA, Petridis P, Bercow AS, Malone H, Praver M, Wang TJC, Isaacson SR, Sisti MB (2017) Efficacy and outcomes of facial nerve-sparing treatment approach to cerebellopontine angle meningiomas. J Neurosurg 127:1231–1241. https://doi.org/10.3171/2016.10.jns161982
da Silva CE, Peixoto de Freitas PE (2016) Recurrence of skull base meningiomas: the role of aggressive removal in surgical treatment. J Neurol Surg Part B, Skull Base 77:219–225. https://doi.org/10.1055/s-0035-1566251
DeMonte F, McDermott MW, Al-Mefty O (2011) Al-Mefty’s meningiomas, 2nd edn. Thieme Medical, New York
Gallagher MJ, Jenkinson MD, Brodbelt AR, Mills SJ, Chavredakis E (2016) WHO grade 1 meningioma recurrence: are location and Simpson grade still relevant? Clin Neurol Neurosurg 141:117–121. https://doi.org/10.1016/j.clineuro.2016.01.006
Hasseleid BF, Meling TR, Ronning P, Scheie D, Helseth E (2012) Surgery for convexity meningioma: Simpson Grade I resection as the goal: clinical article. J Neurosurg 117:999–1006. https://doi.org/10.3171/2012.9.jns12294
Heald JB, Carroll TA, Mair RJ (2013) Simpson grade: an opportunity to reassess the need for complete resection of meningiomas. Acta Neurochir 156:383–388. https://doi.org/10.1007/s00701-013-1923-6
Ichinose T, Goto T, Ishibashi K, Takami T, Ohata K (2010) The role of radical microsurgical resection in multimodal treatment for skull base meningioma. J Neurosurg 113:1072–1078. https://doi.org/10.3171/2010.2.jns091118
Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH (1948) The use of the nitrogen mustards in the palliative treatment of carcinoma—with particular reference to bronchogenic carcinoma. Cancer 1:634–656
Kasuya H, Kubo O, Kato K, Krischek B (2012) Histological characteristics of incidentally-found growing meningiomas. J Med Investig : JMI 59:241–245. https://doi.org/10.2152/jmi.59.241
Kasuya H, Kubo O, Tanaka M, Amano K, Kato K, Hori T (2006) Clinical and radiological features related to the growth potential of meningioma. Neurosurg Rev 29:293–296; discussion 296-297. https://doi.org/10.1007/s10143-006-0039-3
Konglund A, Rogne SG, Lund-Johansen M, Scheie D, Helseth E, Meling TR (2013) Outcome following surgery for intracranial meningiomas in the aging. Acta Neurol Scand 127:161–169. https://doi.org/10.1111/j.1600-0404.2012.01692.x
Kshettry VR, Ostrom QT, Kruchko C, Al-Mefty O, Barnett GH, Barnholtz-Sloan JS (2015) Descriptive epidemiology of World Health Organization grades II and III intracranial meningiomas in the United States. Neuro-Oncology 17:1166–1173. https://doi.org/10.1093/neuonc/nov069
Lassen B, Helseth E, Ronning P, Scheie D, Johannesen TB, Maehlen J, Langmoen IA, Meling TR (2011) Surgical mortality at 30 days and complications leading to recraniotomy in 2630 consecutive craniotomies for intracranial tumors. Neurosurgery 68:1259–1268; discussion 1268-1259. https://doi.org/10.1227/NEU.0b013e31820c0441
Linsler S, Keller C, Urbschat S, Ketter R, Oertel J (2016) Prognosis of meningiomas in the early 1970s and today. Clin Neurol Neurosurg 149:98–103. https://doi.org/10.1016/j.clineuro.2016.08.007
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Mansouri A, Klironomos G, Taslimi S, Kilian A, Gentili F, Khan OH, Aldape K, Zadeh G (2016) Surgically resected skull base meningiomas demonstrate a divergent postoperative recurrence pattern compared with non-skull base meningiomas. J Neurosurg 125:431–440. https://doi.org/10.3171/2015.7.jns15546
Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL (1985) Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 62:18–24. https://doi.org/10.3171/jns.1985.62.1.0018
Modha A, Gutin PH (2005) Diagnosis and treatment of atypical and anaplastic meningiomas: a review. Neurosurgery 57:538–550; discussion 538-550. https://doi.org/10.1227/01.NEU.0000170980.47582.A5
Morokoff AP, Zauberman J, Black PM (2008) Surgery for convexity meningiomas. Neurosurgery 63:427–433; discussion 433-424. https://doi.org/10.1227/01.neu.0000310692.80289.28
Nanda A, Bir SC, Maiti TK, Konar SK, Missios S, Guthikonda B (2016) Relevance of Simpson grading system and recurrence-free survival after surgery for World Health Organization Grade I meningioma. J Neurosurg 126:201–211. https://doi.org/10.3171/2016.1.jns151842
Nanda A, Javalkar V, Banerjee AD (2010) Petroclival meningiomas: study on outcomes, complications and recurrence rates. J Neurosurg 114:1268–1277. https://doi.org/10.3171/2010.11.jns10326
Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009-2013. Neuro-Oncology 18:v1–v75. https://doi.org/10.1093/neuonc/now207
Otero-Rodriguez A, Tabernero MD, Munoz-Martin MC, Sousa P, Orfao A, Pascual-Argente D, Gonzalez-Tablas M, Ruiz-Martin L (2016) Re-evaluating Simpson grade I, II, and III resections in neurosurgical treatment of World Health Organization grade I meningiomas. World Neurosurg 96:483–488. https://doi.org/10.1016/j.wneu.2016.09.007
Palmer JD, Sparrow OC, Iannotti F (1994) Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery 35:1061–1064 discussion 1064-1065
Patibandla MR, Lee CC, Sheehan J (2017) Stereotactic radiosurgery of central skull base meningioma’s—volumetric evaluation and long-term outcomes. World Neurosurg. 108:176–184. https://doi.org/10.1016/j.wneu.2017.08.166
Pettersson-Segerlind J, Orrego A, Lonn S, Mathiesen T (2012) Long-term 25-year follow-up of surgically treated parasagittal meningiomas. World Neurosurg 76:564–571. https://doi.org/10.1016/j.wneu.2011.05.015
Sanai N, Sughrue ME, Shangari G, Chung K, Berger MS, McDermott MW (2009) Risk profile associated with convexity meningioma resection in the modern neurosurgical era. J Neurosurg 112:913–919. https://doi.org/10.3171/2009.6.jns081490
Savardekar AR, Patra DP, Bir S, Thakur JD, Mohammed N, Bollam P, Georgescu MM, Nanda A (2017) Differential tumor progression patterns in skull base versus non-skull base meningiomas: a critical analysis from a long-term follow-up study and review of literature. World Neurosurg. https://doi.org/10.1016/j.wneu.2017.12.035
Scheitzach J, Schebesch KM, Brawanski A, Proescholdt MA (2013) Skull base meningiomas: neurological outcome after microsurgical resection. J Neuro-Oncol 116:381–386. https://doi.org/10.1007/s11060-013-1309-x
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. doi:https://doi.org/10.1136/jnnp.20.1.22
Sindou MP, Alvernia JE (2006) Results of attempted radical tumor removal and venous repair in 100 consecutive meningiomas involving the major dural sinuses. J Neurosurg 105:514–525. https://doi.org/10.3171/jns.2006.105.4.514
Starke RM, Williams BJ, Hiles C, Nguyen JH, Elsharkawy MY, Sheehan JP (2011) Gamma knife surgery for skull base meningiomas. J Neurosurg 116:588–597. https://doi.org/10.3171/2011.11.jns11530
Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, Parsa AT (2010) The relevance of Simpson Grade I and II resection in modern neurosurgical treatment of World Health Organization Grade I meningiomas. J Neurosurg 113:1029–1035. https://doi.org/10.3171/2010.3.jns091971
Talacchi A, Biroli A, Soda C, Masotto B, Bricolo A (2012) Surgical management of ventral and ventrolateral foramen magnum meningiomas: report on a 64-case series and review of the literature. Neurosurg Rev 35:359–367; discussion 367-358. https://doi.org/10.1007/s10143-012-0381-6
van Alkemade H, de Leau M, Dieleman EM, Kardaun JW, van Os R, Vandertop WP, van Furth WR, Stalpers LJ (2012) Impaired survival and long-term neurological problems in benign meningioma. Neuro-Oncology 14:658–666. https://doi.org/10.1093/neuonc/nos013
Voss KM, Spille DC, Sauerland C, Suero Molina E, Brokinkel C, Paulus W, Stummer W, Holling M, Jeibmann A, Brokinkel B (2017) The Simpson grading in meningioma surgery: does the tumor location influence the prognostic value? J Neuro-Oncol 133:641–651. https://doi.org/10.1007/s11060-017-2481-1
Waldron JS, Sughrue ME, Hetts SW, Wilson SP, Mills SA, McDermott MW, Dowd CF, Parsa AT (2010) Embolization of skull base meningiomas and feeding vessels arising from the internal carotid circulation. Neurosurgery 68:162–169; discussion 169. https://doi.org/10.1227/NEU.0b013e3181fe2de9
Whittle IR, Smith C, Navoo P, Collie D (2004) Meningiomas. Lancet (London, England) 363:1535–1543. https://doi.org/10.1016/s0140-6736(04)16153-9
Winther TL, Torp SH (2016) Significance of the extent of resection in modern neurosurgical practice of World Health Organization grade I meningiomas. World Neurosurg 99:104–110. https://doi.org/10.1016/j.wneu.2016.11.034
Zouaoui S, Darlix A, Rigau V, Mathieu-Daude H, Bauchet F, Bessaoud F, Fabbro-Peray P, Tretarre B, Figarella-Branger D, Taillandier L, Loiseau H, Bauchet L (2015) Descriptive epidemiology of 13,038 newly diagnosed and histologically confirmed meningiomas in France: 2006-2010. Neuro-Chirurgie 64:15–21. https://doi.org/10.1016/j.neuchi.2014.11.013
Acknowledgements
The authors would like to thank Bernt Filip Hasseleid, MD; Andreas Mathisen, MD; Andreas Hessen Schei, MD; and Kristina M Ødegaard, MD, for their valuable contributions in collecting data for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Meling, T.R., Da Broi, M., Scheie, D. et al. Meningiomas: skull base versus non-skull base. Neurosurg Rev 42, 163–173 (2019). https://doi.org/10.1007/s10143-018-0976-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0976-7