Abstract
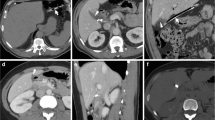
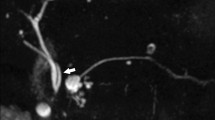
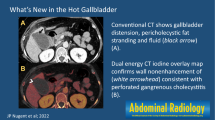
Cholecystectomy is the most performed intra-abdominal surgical procedure in the US, with 1.2 million performed annually, and is predominantly performed laparoscopically. Although largely safe, laparoscopic cholecystectomy results in higher rates of abdominal symptoms consisting of abdominal pain and dyspepsia, which may persist or recur, collectively known as post-cholecystectomy syndrome. This article aims to (1) provide an overview of post-cholecystectomy syndrome with an emphasis on biliary complications and emergent imaging findings, (2) illustrate the spectrum of imaging findings of early and late post-cholecystectomy complications, (3) enumerate the role of various imaging modalities in evaluating post-cholecystectomy complications and address the role of selective trans-catheter coil embolization in managing bile leaks, and (4) discuss pearls and pitfalls in imaging following cholecystectomy. While common first-line imaging modalities for post-cholecystectomy complications include CT and sonography, ERCP and MRCP can delineate the biliary tree with greater detail. Scintigraphy has a higher sensitivity and specificity than CT or sonography for diagnosing bile leak and may preclude the need for ERCP. Post-operative complications include biliary duct injury or leak, biliary obstruction, remnant gallbladder/cystic duct stones and inflammation, biliary dyskinesia, papillary stenosis, and vascular injury. Subtle cases resulting in lethal outcomes, such as hemorrhage from the gallbladder bed without major vessel injury, have also been described. Cases presented will include biliary complications such as post-cholecystectomy stump cholecystitis, nonbiliary complications such as subcapsular hematoma, and normal post-surgical findings such as oxidized regenerated cellulose. Post-operative biliary complications can cause significant morbidity and mortality, and thus familiarity with the expected post-surgical appearance of the gallbladder fossa and biliary tract, as well as understanding the spectrum of complications and associated multimodality imaging findings, are essential for emergency radiologists and those practicing in the acute care setting to direct appropriate patient management. Furthermore, many of the postoperative complications can be managed by noninvasive percutaneous interventional procedures, from drain placement to cystic artery and cystic duct stump embolization.












Similar content being viewed by others
References
Jones MW GE, Deppen JG Open Cholecystectomy. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448176/?report=classic. Accessed 24 Oct 2022
Reynolds W Jr (2001) The first laparoscopic cholecystectomy. Jsls 5(1):89–94
Gadacz TR, Talamini MA (1991) Traditional versus laparoscopic cholecystectomy. Am J Surg 161(3):336–338. https://doi.org/10.1016/0002-9610(91)90591-z
Desai NS, Khandelwal A, Virmani V, Kwatra NS, Ricci JA, Saboo SS (2014) Imaging in laparoscopic cholecystectomy–what a radiologist needs to know. Eur J Radiol 83(6):867–879. https://doi.org/10.1016/j.ejrad.2014.02.016
Catalano OA, Singh AH, Uppot RN, Hahn PF, Ferrone CR, Sahani DV (2008) Vascular and biliary variants in the liver: implications for liver surgery. Radiographics 28(2):359–378. https://doi.org/10.1148/rg.282075099
Wojcicki M, Patkowski W, Chmurowicz T, Bialek A, Wiechowska-Kozlowska A, Stankiewicz R, Milkiewicz P, Krawczyk M (2013) Isolated right posterior bile duct injury following cholecystectomy: report of two cases. World J Gastroenterol 19(36):6118–6121. https://doi.org/10.3748/wjg.v19.i36.6118
Mariolis-Sapsakos T, Kalles V, Papatheodorou K, Goutas N, Papapanagiotou I, Flessas I, Kaklamanos I, Arvanitis DL, Konstantinou E, Sgantzos MN (2012) Anatomic variations of the right hepatic duct: results and surgical implications from a cadaveric study. Anat Res Int 2012:838179. https://doi.org/10.1155/2012/838179
Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, Zuiani C (2010) Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol 83(988):351–361. https://doi.org/10.1259/bjr/99865290
Tonolini M, Ierardi AM, Patella F, Carrafiello G (2018) Early cross-sectional imaging following open and laparoscopic cholecystectomy: a primer for radiologists. Insights Imaging 9(6):925–941. https://doi.org/10.1007/s13244-018-0663-9
Thurley PD, Dhingsa R (2008) Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol 191(3):794–801. https://doi.org/10.2214/AJR.07.3485
Turley BR, Taupmann RE, Johnson PL (1994) Postoperative abscess mimicked by surgicel. Abdom Imaging 19(4):345–346. https://doi.org/10.1007/bf00198195
Stringer MD, Dasgupta D, McClean P, Davison S, Ramsden W (2003) “Surgicel abscess” after pediatric liver transplantation: a potential trap. Liver Transpl 9(2):197–198. https://doi.org/10.1053/jlts.2003.50059
Park SM, Kim WS, Bae IH, Kim JH, Ryu DH, Jang LC, Choi JW (2012) Common bile duct dilatation after cholecystectomy: a one-year prospective study. J Korean Surg Soc 83(2):97–101. https://doi.org/10.4174/jkss.2012.83.2.97
Khan MH, Howard TJ, Fogel EL, Sherman S, McHenry L, Watkins JL, Canal DF, Lehman GA (2007) Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: experience at a large tertiary referral center. Gastrointest Endosc 65(2):247–252. https://doi.org/10.1016/j.gie.2005.12.037
Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B (2015) Etiology, diagnosis, and management of bilomas: a current update. Tech Vasc Interv Radiol 18(4):236–243. https://doi.org/10.1053/j.tvir.2015.07.007
Cohen JT, Charpentier KP, Beard RE (2019) An update on iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am 99(2):283–299. https://doi.org/10.1016/j.suc.2018.11.006
Kuligowska E, Schlesinger A, Miller KB, Lee VW, Grosso D (1983) Bilomas: a new approach to the diagnosis and treatment. Gastrointest Radiol 8(3):237–243. https://doi.org/10.1007/BF01948126
Braghetto I, Bastias J, Csendes A, Debandi A (2000) Intraperitoneal bile collections after laparoscopic cholecystectomy: causes, clinical presentation, diagnosis, and treatment. Surg Endosc 14(11):1037–1041. https://doi.org/10.1007/s004649900029
Aduna M, Larena JA, Martin D, Martinez-Guerenu B, Aguirre I, Astigarraga E (2005) Bile duct leaks after laparoscopic cholecystectomy: value of contrast-enhanced MRCP. Abdom Imaging 30(4):480–487. https://doi.org/10.1007/s00261-004-0276-2
Petrillo M, Ierardi AM, Tofanelli L, Maresca D, Angileri A, Patella F, Carrafiello G (2019) Gd-EOB-DTP-enhanced MRC in the preoperative percutaneous management of intra and extrahepatic biliary leakages: does it matter? Gland Surg 8(2):174–183. https://doi.org/10.21037/gs.2019.03.09
Kul M, Erden A, Dusunceli Atman E (2017) Diagnostic value of Gd-EOB-DTPA-enhanced MR cholangiography in non-invasive detection of postoperative bile leakage. Br J Radiol 90(1072):20160847. https://doi.org/10.1259/bjr.20160847
Kantarci M, Pirimoglu B, Karabulut N, Bayraktutan U, Ogul H, Ozturk G, Aydinli B, Kizrak Y, Eren S, Yilmaz S (2013) Non-invasive detection of biliary leaks using Gd-EOB-DTPA-enhanced MR cholangiography: comparison with T2-weighted MR cholangiography. Eur Radiol 23(10):2713–2722. https://doi.org/10.1007/s00330-013-2880-4
Nezami N, Jarmakani H, Arici M, Latich I, Mojibian H, Ayyagari RR, Pollak JS, Perez Lozada JCL (2019) Selective trans-catheter coil embolization of cystic duct stump in post-cholecystectomy bile leak. Dig Dis Sci 64(11):3314–3320. https://doi.org/10.1007/s10620-019-05677-5
Seewald S, Groth S, Sriram PV, Xikun H, Akaraviputh T, Mendoza G, Brand B, Seitz U, Thonke F, Soehendra N (2002) Endoscopic treatment of biliary leakage with n-butyl-2 cyanoacrylate. Gastrointest Endosc 56(6):916–919. https://doi.org/10.1067/mge.2002.129873
Schelhammer F, Dahl SV, Heintges T, Furst G (2007) A multimodal approach in coil embolization of a bile leak following cholecystectomy. Cardiovasc Intervent Radiol 30(3):529–530. https://doi.org/10.1007/s00270-006-0090-z
Kaushik R (2010) Bleeding complications in laparoscopic cholecystectomy: incidence, mechanisms, prevention and management. J Minim Access Surg 6(3):59–65. https://doi.org/10.4103/0972-9941.68579
Sureka B, Mukund A (2017) Review of imaging in post-laparoscopy cholecystectomy complications. Indian J Radiol Imaging 27(4):470–481. https://doi.org/10.4103/ijri.IJRI_489_16
Yao CA, Arnell TD (2010) Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Am J Surg 199(1):e10-11. https://doi.org/10.1016/j.amjsurg.2009.03.014
Moloney BM, Hennessy N, Malley EO, Orefuwa F, McCarthy PA, Collins CG (2017) Subcapsular haematoma following laparoscopic cholecystectomy. BJR Case Rep 3(2):20160118. https://doi.org/10.1259/bjrcr.20160118
Schafer M, Lauper M, Krahenbuhl L (2000) A nation’s experience of bleeding complications during laparoscopy. Am J Surg 180(1):73–77. https://doi.org/10.1016/s0002-9610(00)00416-5
Saad E, O’Connell L, Browne AM, Khan W, Waldron R, Barry K, Khan IZ (2020) Giant intrahepatic subcapsular haematoma: a rare complication following laparoscopic cholecystectomy-a case report and literature review. Case Rep Surg 2020:6410790. https://doi.org/10.1155/2020/6410790
Ikoma N, Anderson CL, Ohanian M, Juneja HS, MacFadyen BV, Shah SK, Bajwa KS (2014) Portal vein thrombosis after laparoscopic cholecystectomy. JSLS 18(1):125–127. https://doi.org/10.4293/108680813X13654754535674
Calhoun SK, Piechowiak RL (2010) Recurrent cholecystitis and cholelithiasis in a gallbladder remnant 14 years after a converted cholecystectomy. Radiol Case Rep 5(1):332. https://doi.org/10.2484/rcr.v5i1.332
Tantia O, Jain M, Khanna S, Sen B (2008) Post cholecystectomy syndrome: role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg 4(3):71–75. https://doi.org/10.4103/0972-9941.43090
Cawich SO, Wilson C, Simpson LK, Baker AJ (2014) Stump cholecystitis: laparoscopic completion cholecystectomy with basic laparoscopic equipment in a resource poor setting. Case Rep Med 2014:787631. https://doi.org/10.1155/2014/787631
Kar A, Gulati S, Mohammed S, Valappil MV, Sarala BB, Ghatak S, Bhattacharyya A (2018) Surgical management of cystic duct stump stone or gall bladder remnant stone. Indian J Surg 80(3):284–287. https://doi.org/10.1007/s12262-018-1724-5
Mageed SAA, Omar MA, Redwan AA (2018) Remnant gall bladder and cystic duct stump stone after cholecystectomy: tertiary multicenter experience. Int Surg J
Perera E, Bhatt S, Dogra VS (2011) Cystic duct remnant syndrome. J Clin Imaging Sci 1:2. https://doi.org/10.4103/2156-7514.73500
Almadi MA, Barkun JS, Barkun AN (2012) Management of suspected stones in the common bile duct. CMAJ 184(8):884–892. https://doi.org/10.1503/cmaj.110896
Kim JY, Kim KW, Ahn CS, Hwang S, Lee YJ, Shin YM, Lee MG (2008) Spectrum of biliary and nonbiliary complications after laparoscopic cholecystectomy: radiologic findings. AJR Am J Roentgenol 191(3):783–789. https://doi.org/10.2214/AJR.07.3602
Lee DH, Ahn YJ, Lee HW, Chung JK, Jung IM (2016) Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis. Ann Surg Treat Res 91(5):239–246. https://doi.org/10.4174/astr.2016.91.5.239
Ratanaprasatporn L, Uyeda JW, Wortman JR, Richardson I, Sodickson AD (2018) Multimodality imaging, including dual-energy CT, in the evaluation of gallbladder disease. Radiographics 38(1):75–89. https://doi.org/10.1148/rg.2018170076
Kim CW, Chang JH, Lim YS, Kim TH, Lee IS, Han SW (2013) Common bile duct stones on multidetector computed tomography: attenuation patterns and detectability. World J Gastroenterol 19(11):1788–1796. https://doi.org/10.3748/wjg.v19.i11.1788
Shirah BH, Shirah HA, Zafar SH, Albeladi KB (2018) Clinical patterns of postcholecystectomy syndrome. Ann Hepatobiliary Pancreat Surg 22(1):52–57. https://doi.org/10.14701/ahbps.2018.22.1.52
Busireddy KK, AlObaidy M, Ramalho M, Kalubowila J, Baodong L, Santagostino I, Semelka RC (2014) Pancreatitis-imaging approach. World J Gastrointest Pathophysiol 5(3):252–270. https://doi.org/10.4291/wjgp.v5.i3.252
Manikkavasakar S, AlObaidy M, Busireddy KK, Ramalho M, Nilmini V, Alagiyawanna M, Semelka RC (2014) Magnetic resonance imaging of pancreatitis: an update. World J Gastroenterol 20(40):14760–14777. https://doi.org/10.3748/wjg.v20.i40.14760
Shanbhogue AK, Tirumani SH, Prasad SR, Fasih N, McInnes M (2011) Benign biliary strictures: a current comprehensive clinical and imaging review. AJR Am J Roentgenol 197(2):W295-306. https://doi.org/10.2214/AJR.10.6002
Singh A, Gelrud A, Agarwal B (2015) Biliary strictures: diagnostic considerations and approach. Gastroenterol Rep (Oxf) 3(1):22–31. https://doi.org/10.1093/gastro/gou072
Gorsi U, Gupta P, Kalra N, Kang M, Singh R, Gupta R, Gupta V, Khandelwal N (2015) Multidetector computed tomography evaluation of post cholecystectomy complications: a tertiary care center experience. Trop Gastroenterol 36(4):236–243. https://doi.org/10.7869/tg.297
Ward J, Sheridan MB, Guthrie JA, Davies MH, Millson CE, Lodge JP, Pollard SG, Prasad KR, Toogood GJ, Robinson PJ (2004) Bile duct strictures after hepatobiliary surgery: assessment with MR cholangiography. Radiology 231(1):101–108. https://doi.org/10.1148/radiol.2311030017
Chong VH, Chong CF (2010) Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg 14(4):688–696. https://doi.org/10.1007/s11605-009-1131-0
Entel RJ, Peebles MW (1996) Migratory surgical clip in the common bile duct: CT diagnosis. Abdom Imaging 21(4):329–330. https://doi.org/10.1007/s002619900074
Moga D, Perisanu S, Popentiu A, Sora D, Magdu H (2016) Right retroperitoneal and subhepatic abscess; late complications due to spilled stones during laparoscopic cholecystectomy - case report. Chirurgia (Bucur) 111(1):67–70
Robinson JR, Wright JK, Geevarghese SK (2015) Dropped gallstones causing a perihepatic abscess and empyema. Case Rep Surg 2015:629704. https://doi.org/10.1155/2015/629704
Diez J, Arozamena C, Gutierrez L, Bracco J, Mon A, Sanchez Almeyra R, Secchi M (1998) Lost stones during laparoscopic cholecystectomy. HPB Surg 11(2):105–108. https://doi.org/10.1155/1998/95874. (discuss 108-109)
Woodfield JC, Rodgers M, Windsor JA (2004) Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. Surg Endosc 18(8):1200–1207. https://doi.org/10.1007/s00464-003-8260-4
Zehetner J, Shamiyeh A, Wayand W (2007) Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg 193(1):73–78. https://doi.org/10.1016/j.amjsurg.2006.05.015
Viera FT, Armellini E, Rosa L, Ravetta V, Alessiani M, Dionigi P, Rossi S (2006) Abdominal spilled stones: ultrasound findings. Abdom Imaging 31(5):564–567. https://doi.org/10.1007/s00261-005-0241-8
Nayak L, Menias CO, Gayer G (2013) Dropped gallstones: spectrum of imaging findings, complications and diagnostic pitfalls. Br J Radiol 86(1028):20120588. https://doi.org/10.1259/bjr.20120588
Funding
Carrie Hoff received unrelated grant funding from NHTSA/CIREN.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maddu, K., Polireddy, K., Hsu, D. et al. Do not get stumped: multimodality imaging findings of early and late post-cholecystectomy complications. Emerg Radiol 30, 351–362 (2023). https://doi.org/10.1007/s10140-023-02131-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-023-02131-y