Abstract
Purpose
To investigate if the presence of systemic inflammatory response syndrome (SIRS) in patients with urinary tract obstruction at time of presentation to the emergency department correlates with a subsequent positive urine culture and to determine if it could be used as a tool to predict the urgency of a percutaneous nephrostomy (PCN). The secondary aim of the study was to assess the incidence of in-hour and after-hour emergent PCNs performed in a tertiary center which has both interventional radiological and urological expertise.
Methods and materials
Emergent adult PCN cases referred from the emergency department between 2011 and 2016 were identified retrospectively. Urine culture results, clinical features of SIRS, timing of procedure, and radiological findings were analyzed.
Results
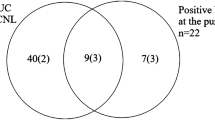
A total of 110 patients met the inclusion criteria. There were a total of 60 male and 50 female patients with a mean age of 62 (age range 18–99 years). Ninety-two (83%) PCN patients were referred and performed on after-hours with the remaining 18 patients performed in-hours. There were 53 (48%) patients that met the criteria for obstruction with SIRS and 57 (52%) patients with obstruction without SIRS. The number of after-hours PCN performed in both groups was equal at 46 patients each. The most common cause of obstruction in the SIRS group was stone related in 31 (58%) patients. Whereas, the most common cause of obstruction in the non-SIRS group was due to malignancy in 26 (45%) cases. An elevated temperature and heart rate were the most common features of SIRS at 96 and 83% respectively in the SIRS group. An organism was isolated in 35 (67%) out of the 52 urine culture results obtained for the SIRS group. No organism was isolated in 42 (95%) out of the 44 urine culture results obtained in the non-SIRS group. Statistical analysis using Fisher’s test revealed that the association between obstruction without SIRS and a negative urine culture result was statistically significant (p < 0.0001).
Conclusion
A large percentage (50%) of PCN cases performed after-hours could have been performed during daytime hours instead due to the absence of infection. This would be in line with the practices of some centers that consider an infected obstructed kidney as the only absolute indication for emergent decompression overnight. The study also demonstrates that the absence of a SIRS in a patient with urinary tract obstruction correlates well with a negative urine culture result from the nephrostomy specimen which has a high negative predictive value for excluding pyonephrosis.


Similar content being viewed by others
References
Sierakowski R, Finlayson B, Landes RR, Finlayson CD, Sierakowski N (1978) The frequency of urolithiasis in hospital discharge diagnoses in the United States. Investig Urol 15(6):438–441
Lameire N, Van Biesen W, Vanholder R. Acute renal failure. Lancet (London, England) 2005; 365(9457):417–430
Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, Knoll T, Lingeman JE, Nakada SY, Pearle MS, Sarica K, Türk C, Wolf JS Jr, EAU/AUA Nephrolithiasis Guideline Panel (2007) 2007 guideline for the management of ureteral calculi. J Urol 178(6):2418–2434
Goodwin WE, Casey WC, Woolf W (1955) Percutaneous trocar (needle) nephrostomy in hydronephrosis. J Am Med Assoc 157(11):891–894
Ahmad I, Saeed Pansota M, Tariq M, Shahzad Saleem M, Ali Tabassum S, Hussain A (2013) Comparison between double J (DJ) ureteral stenting and percutaneous nephrostomy (PCN) in obstructive Uropathy. Pakistan J Med Sci 29(3):725–729
Pearle MS, Pierce HL, Miller GL, Summa JA, Mutz JM, Petty BA et al (1998) Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol 160(4):1260–1264
Ramsey S, Robertson A, Ablett MJ, Meddings RN, Hollins GW, Little B (2010) Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol 24(2):185–189
Wagenlehner FM, Lichtenstern C, Rolfes C, Mayer K, Uhle F, Weidner W, Weigand MA (2013) Diagnosis and management for urosepsis. Int J Urology: Off J Japan Urol Assoc 20(10):963–970
Borofsky MS, Walter D, Shah O, Goldfarb DS, Mues AC, Makarov DV (2013) Surgical decompression is associated with decreased mortality in patients with sepsis and ureteral calculi. J Urol 189(3):946–951
Liu J-J, Shortliffe LMD. 50- renal abscess and other complex renal infections A2 Long SS. Principles and practice of pediatric infectious diseases (fourth edition). London: Content Repository Only!; 2012 p 343-5.e1
Dagli M, Ramchandani P (2011) Percutaneous nephrostomy: technical aspects and indications. Semin Interv Radiol 28(4):424–437
Regalado SP (2006) Emergency percutaneous nephrostomy. Semin Interv Radiol 23(3):287–294
Lucarelli G, Ditonno P, Bettocchi C, Grandaliano G, Gesualdo L, Selvaggi FP, Battaglia M (2013) Delayed relief of ureteral obstruction is implicated in the long-term development of renal damage and arterial hypertension in patients with unilateral ureteral injury. J Urol 189(3):960–965
Papagiannopoulos D, Whelan P, Ahmad W, Rybak J, Hota B, Deane L, Nehra A (2016) Procalcitonin is a strong predictor of urine culture results in patients with obstructing ureteral stones: a prospective, pilot study. Urol Annals 8(3):277–280
Grabe MB-JT, Botto H et al (2015) Guidelines on urological infections 2015. European Association of Urology
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Critical care medicine 20(6):864–874
Burrell AR, McLaws ML, Fullick M, Sullivan RB, Sindhusake D (2016) SEPSIS KILLS: early intervention saves lives. Med J Aust 204(2):73.e1–73.e7
Dreger NM, Degener S, Ahmad-Nejad P, Wobker G, Roth S. Urosepsis—etiology, diagnosis, and treatment. Deutsches Arzteblatt international 2015; 112(49):837–847; quiz 48
Lewis S, Patel U (2004) Major complications after percutaneous nephrostomy—lessons from a department audit. Clin Radiol 59(2):171–179
Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA (2004) Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med 351(18):1838–1848
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Local institutional low risk ethics approval was obtained (17-000-553Q).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Koh, D., Lau, K.K. & Teoh, E. Are all urgent nephrostomies that urgent?. Emerg Radiol 25, 381–386 (2018). https://doi.org/10.1007/s10140-018-1598-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-018-1598-7