Abstract
Background
Accelerated tumor growth during immunotherapy in pre-existing measurable lesions, hyperprogressive disease (HPD), has been reported. However, progression of non-measurable lesions and new lesions are frequently observed in patients with advanced gastric cancer (AGC).
Methods
This retrospective study involved AGC patients at 24 Japanese institutions who had measurable lesions and received nivolumab after ≥ 2 lines of chemotherapy. HPD was defined as a ≥ two-fold increase in the tumor growth rate of measurable lesions. The pattern of disease progression was classified according to new lesions in different organs and ascites appeared/increase of ascites.
Results
Of 245 patients, 147 (60.0%) showed progressive disease (PD) as the best response and 41 (16.7%) showed HPD during nivolumab monotherapy. There was no significant difference in overall survival (OS) between patients with HPD and those with PD other than HPD (median OS 5.0 vs 4.8 months; hazard ratio [HR] 1.0, 95% confidence interval [CI] 0.6–1.5; p = 1.0). Fifty-three patients developed new lesions in different organs and 58 had appearance/increase of ascites; these patients showed shorter OS than those without each of these features (median OS 3.3 vs 7.1 months, HR 1.8, 95% CI 1.2–2.7, p = 0.0031 for new lesions, and 3.0 vs 7.8 months, HR 2.6, 95% CI 1.8–3.8, p < 0.0001 for ascites). Thirty-one patients who had both features showed the worst prognosis (median OS 2.6 months).
Conclusions
New lesions in different organs and appearance/increase of ascites, rather than the original definition of HPD, are the patterns of disease progression associated with poor prognosis in AGC patients receiving nivolumab whose best response was PD.
Similar content being viewed by others
Introduction
Gastric cancer is the fifth most common malignancy and the fourth leading cause of cancer-related death worldwide. The incidence of gastric cancer is two-fold higher in men than in women. In several Asian countries, gastric cancer is the most common cancer in men and the leading cause of cancer-related death [1]. Japan and Korea have a nationwide screening system for gastric cancer. However, with the exception of these two countries, many patients with gastric cancer have unresectable disease at the time of diagnosis, and the cure rate remains low even after surgical resection with or without perioperative adjuvant chemotherapy. The clinical outcome of advanced gastric cancer (AGC) that is unresectable or recurrent remains poor, with median overall survival (OS) of around 1 year despite the various chemotherapeutic agents available.
Several guidelines recommend a combination of platinum and fluoropyrimidine as the first-line treatment for AGC [2,3,4,5,6] with addition of trastuzumab in patients who are positive for human epidermal growth factor receptor 2 [7]. The recommended second-line treatment is a combination of paclitaxel and ramucirumab, a vascular endothelial growth factor receptor 2 antibody [8]. Depending on the patient’s general condition, the recommendations for third-line treatment include trifluridine/tipiracil (TFTD) [9], trastuzumab deruxtecan (T-DXd) [10], irinotecan[11,12,13,14], and an immune checkpoint inhibitor (ICI) targeting the programmed cell death (PD)-1 protein, such as nivolumab [15] or pembrolizumab [16,17,18]. Recently, considerable progress has been made. In the CheckMate-649 study, nivolumab plus chemotherapy achieved significant improvements in OS and progression-free survival (PFS) not only in patients with a combined positive score of PD-ligand 1 ≥ 5 but also in all randomized patients [19]. Accordingly, nivolumab has been approved for use in combination with chemotherapy as first-line treatment for AGC.
However, ICIs may cause a rapid type of tumor growth known as hyperprogressive disease (HPD) [20]. HPD was originally defined as a ≥ two-fold increase in the tumor growth rate (TGR), assessed as the change in volume of a pre-existing measurable lesion per unit time [21], compared with that at the evaluation of disease progression during the previous line of treatment. HPD has attracted attention because it is reported to be associated with poor prognosis. Although the definition of HPD varies slightly from study to study, there have been several reports of HPD during anti-PD-1/PD-L1 therapy. In one study, 12 of 131 patients (9%) with various types of cancer, including melanoma and lung, renal, and colorectal cancer, developed HPD [20], as did 10 of 34 patients (29%) with head and neck cancer [22] and 56 of 406 patients (14%) with lung cancer [23]. There have also been reports on AGC in which 13 of 62 patients (21%) [24], 10 of 34 patients (29%) [25] and 45 of 219 patients (20.5%) [26] developed HPD that was associated with poor prognosis.
Approximately 30%–50% of patients with AGC present with peritoneal metastasis, which is a typical pattern of disease progression in patients with AGC and is well known to be associated with poor prognosis. However, peritoneal metastasis is not included in the original definition of HPD because it is not a measurable lesion. Moreover, there has also been a report suggesting that disease progression accompanied by new lesions has a strong negative impact on the prognosis in patients with AGC [27]. Given the lack of difference in the biological mechanism of ICI-induced rapid progression between measurable lesions and non-measurable/new lesions, exclusion of peritoneal metastasis and new lesions from the definition of HPD may lead to underestimation of accelerated tumor growth during treatment with ICI in patients with AGC.
The aims of this study were to (1) determine the prevalence, background characteristics, and clinical outcomes of HPD in patients with AGC receiving nivolumab monotherapy as salvage treatment and (2) investigate the pattern of disease progression associated with poor prognosis, focusing on peritoneal metastasis and new lesions.
Methods
Patients and treatment
This multicenter retrospective study involved patients with AGC who received nivolumab 3 mg/kg or 240 mg/body intravenously every 2 weeks as a third-line or later treatment at 24 participating Japanese institutions between September 2017 and October 2018.
The inclusion criteria were as follows: age ≥ 20 years; histologically confirmed advanced unresectable or recurrent gastric/gastro-esophageal junction adenocarcinoma; refractory to or intolerant of at least 2 previous lines of chemotherapy (must be refractory to the immediately preceding chemotherapy); at least 1 measurable lesion according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1; and radiologic images available at 2 time points for evaluating disease progression during previous chemotherapy, the latter of which was used as the baseline for evaluation of the response to nivolumab in some patients, and those for first evaluation of response after initiating nivolumab. Patients who had received previous immunotherapy were excluded. The study was approved by the ethics committee of the National Cancer Center and by all participating institutions.
Tumor growth rate
Tumor response was assessed according to RECIST version 1.1. The TGR was assessed by comparing the two images obtained during the immediately preceding therapy and during treatment with nivolumab, respectively.
TGR was calculated using the following method. Taking D as the sum of the largest diameters of the target lesions as per RECIST version 1.1 (new lesions and non-measurable lesions were not included) and virtually representing a single lesion with size D, the tumor volume (V) is approximated as V = 4/3 × π × R3, where R is the radius (D/2) of the sphere. Assuming the tumor grows at an exponential rate, the tumor volume at time t (Vt) can be calculated as Vt = V0 exp(TG·t), where V0 is the volume at baseline and t is the interval time (months) between successive CT scans. Tumor growth (TG) is then calculated as TG = 3 Log(Dt/D0)/t. Finally, TGR, which is the percentage increase in tumor volume per month, is obtained using the following formula: TGR = 100 [exp(TG) − 1] [20, 28,29,30]. The TGR during the previous therapy and that during treatment with nivolumab were compared, and an increase in TGR of ≥ two-fold was defined as HPD [20].
Non-measurable lesions and appearance of new lesions
When evaluating disease progression during treatment with nivolumab, we also investigated factors not included in the original definition of HPD, namely, new lesions appearing in different organs other than those involved before initiating nivolumab and ascites (representing peritoneal metastasis). Definition of appearance/increase of ascites was based on the Response Evaluation Criteria in Solid Tumors (RECIST), which was judged as unequivocal disease progression by each physician. Patterns of progression were classified as follows according to whether new lesions developed in different organs or not and whether ascites appeared/increased or not: group (G) 1 (−/−), G 2 (+/−), G 3 (−/+), and G 4 (+/+).
Statistical analysis
Categorical valuables were compared using Fisher’s exact test and continuous variables using the t test. The neutrophil-to-lymphocyte ratio (NLR) was calculated from the laboratory data obtained immediately before initiating nivolumab. Receiver-operating characteristic curves was used to determine the optimum cut-off value for NLR in association with HPD status. The cut-off for tumor size was set at the median value. Upper limit of normal was cut-off value for alkaline phosphatase (ALP), which was included in the Japan Clinical Oncology Group (JCOG) prognostic factor [31]. OS was defined as the time from initiation of nivolumab until the date of death from any cause or censored at the latest follow-up for surviving patients. PFS was defined as the time from initiation of nivolumab until detection of disease progression or death, and survivors without disease progression were censored at the last contact. Survival functions of OS and PFS were estimated using the Kaplan–Meier method and compared using the log-rank test. Hazard ratios (HRs) were estimated using a univariable Cox proportional hazards model. Adjusted odds ratios (OR) for inability to receive subsequent chemotherapy after disease progression were obtained by multivariable logistic regression analysis. All statistical analyses were performed using EZR software for Windows (version 1.37) and SAS version 9.4 (SAS Institute Incorporated, Cary, NC, USA). A p value of < 0.05 was considered statistically significant.
Results
Patient characteristics
The study population consisted of 245 patients at 24 hospitals who received nivolumab between September 2017 and October 2018 and for whom the TGR immediately before and during nivolumab therapy could be calculated. Baseline characteristics at initiation of nivolumab are shown in Table 1. Median age was 69 years (range 29–94) and 186 patients (75.9%) were male. Eastern Cooperative Oncology Group performance status was 1 or 2 in 176 patients (71.9%). Ninety-three patients (38.0%) had been treated with 3 or more lines of chemotherapy. Peritoneal metastasis was observed in 107 patients (43.7%).
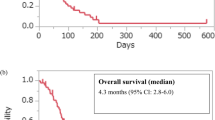
Effect of HPD on clinical outcomes in AGC
After initiation of nivolumab, the median follow-up duration in survivors was 13.0 months (range 11.6–14.2). Median OS was 8.5 months (95% confidence interval [CI] 7.3–9.5) and median PFS was 1.9 months (95% CI 1.9–2.3) (Fig. 1). Of the 245 patients, 36 achieved a partial response (PR), including 2 patients showing pseudo progression (1.0%) at the first evaluation and tumor shrinkage thereafter. No patient achieved a complete response, giving a response rate of 14.7% (95% CI 10.5–19.8). One hundred forty-seven patients (60.0%) showed PD as their best response, in whom median PFS was 1.5 months (95% CI 1.4–1.6) and OS was 4.8 months (95% CI 4.1–6.4). In these 147 patients with PD as the best response, 41 were classified as having HPD (Supplementary Table 1). There were no significant differences in baseline characteristics at initiation of nivolumab between the 41 patients with HPD and the 106 patients with PD other than HPD (non-HPD) (Table 2). Forty-seven (44.3%) of the 106 patients with non-HPD and 19 (46.3%) of the 41 patients with HPD received subsequent chemotherapy after disease progression (Supplementary Table 2).
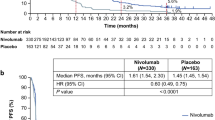
Next, we compared the prognosis of patients with HPD with that of patients with non-HPD, stable disease (SD), or PR (Fig. 2). Median PFS was 1.4 months (95% CI 1.3–1.6) in patients with HPD, 1.6 months (95% CI 1.4–1.7) in those with non-HPD, 5.3 months (95% CI 4.0–6.3) in those with SD, and 11.4 months (95% CI 6.7–NA) in those with PR. Median OS was 5.0 months (95% CI 3.3–7.6) in patients with HPD, 4.8 months (95% CI 4.0–7.1) in those with non-HPD, 11.6 months (95% CI 8.5–16.7) in those with SD, and not reached in those with PR. Although the median PFS was slightly shorter in the 41 patients with HPD than in the 106 with non-HPD (median 1.4 months vs 1.6 months; HR 1.5, 95% CI 1.1–2.2; p = 0.02), there was no significant difference in OS between patients with HPD and those with non-HPD (median 5.0 months vs 4.8 months; HR 1.0, 95% CI 0.6–1.5; p = 1.0). Furthermore, there was no difference in OS between patients with HPD and those with non-HPD even among the patients with 2 lines of previous chemotherapy (median 7.6 months vs 7.8 months; HR 0.9, 95% CI 0.5–1.6; p = 0.6972).
Kaplan–Meier plots showing progression-free survival (PFS) and overall survival (OS). Purple lines indicate patients with hyperprogressive disease (HPD), green lines indicate patients with progressive disease (PD) (non-HPD), blue lines indicate patients with stable disease (SD), and red lines indicate patients with a partial response (PR). a PFS curves after initiation of nivolumab. b OS curves after initiation of nivolumab
Clinical outcomes in patients with new lesions in different organs
New lesions appeared at the time of disease progression during nivolumab in 73 (49.7%) of 147 patients whose best response was PD. There was no significant difference in median OS between the 73 patients with appearance of new lesions regardless of anatomic sites and the 74 with PD in pre-existing lesions without new lesions (4.1 months vs 6.3 months; HR 1.1, 95% CI 0.8–1.7; p = 0.5053) (Supplementary Fig. 1). There was also no significant difference in OS according to the number of new lesions (data not shown). In contrast, new lesions appeared in different organs in 53 of these patients (36.1%) of 147 patients with PD as the best response. OS was significantly worse in the 53 patients in whom new lesions appeared in different organs than in the 94 in whom they did not (median 3.3 months vs 7.1 months; HR 1.8, 95% CI 1.2–2.7; p = 0.0031) (Fig. 3a); there were no significant differences in baseline characteristics at initiation of nivolumab between these groups (Supplementary Table 3).
Kaplan–Meier plots showing overall survival (OS). a OS curves after initiation of nivolumab according to whether or not new lesions appeared in different organs. Blue lines indicate patients with new lesions in different organs and red lines indicate patients with no such lesions. b OS curves after initiation of nivolumab according to whether or not there was a change in amount of ascites. Blue lines indicate patients in whom ascites appeared/increased and red lines indicate patients in whom ascites remained stable/decreased. c OS curves after initiation of nivolumab according to whether or not new lesions appeared in different organs and/or ascites appeared/increased: group 1 (−/−), group 2 (+/−), group 3 (−/+), and group 4 (+/+). Red lines indicate patients in group 1, blue lines indicate patients in group 2, green lines indicate patients in group 3, and purple lines indicate patients in group 4
Clinical outcomes in patients with an appearance/increase of ascites
Ascites appeared/increased in 58 (39.5%) of the 147 patients whose best response was PD; in 29 of these 58 patients, ascites appeared as a new lesion. OS was significantly shorter in these 58 patients with appearance/increase of ascites than in the 89 patients with stable/decreased ascites (median 3.0 months vs 7.8 months; HR 2.6, 95% CI 1.8–3.8; p < 0.0001) (Fig. 3b). Large tumor size, presence of peritoneal metastasis, unresectable disease (stage IV), more previous lines of chemotherapy, and high NLR at baseline tended to be more common in the 58 patients with appearance/increase of ascites (Supplementary Table 4). Patients with an increase in ascites had more difficulty receiving subsequent chemotherapy after disease progression than the other groups of patients (51.7% [46/89] vs 75.9% [44/58]; p = 0.03). In multivariable analysis, appearance/increase of ascites was associated with inability to receive chemotherapy after disease progression (Supplementary Table 2).
Clinical outcomes of four patterns of disease progression classified by new lesions in different organs and an appearance/increase of ascites
The 147 patients whose best response was PD were then classified into 4 groups of disease progression patterns according to whether or not new lesions appeared in different organs before initiation of nivolumab and according to whether or not ascites appeared/increased (group 1 [−/−] n = 67, group 2 [+/−] n = 22, group 3 [−/+] n = 27, and group 4 [+/+] n = 31). Patients in group 4 tended to have larger tumors, more previous lines of chemotherapy, and a higher NLR at baseline (Table 3). Patients in group 4 had the poorest median OS (2.6 months vs 8.0 months in group 1; HR 3.2, 95% CI 2.0–5.3; p < 0.0001) (Table 4, Fig. 3c). Patients were divided into eight groups according to presence or absence of an increase in TGR of ≥ two-fold, new lesions in different organs and appearance/increase of ascites: group 1 [+/+/+], group 2 [+/+/−], group 3 [+/−/+], group 4 [+/−/−], group 5 [−/+/+], group 6 [−/+/−], group 7 [−/−/+] and group 8 [−/−/−] (Supplementary Fig. 2). Comparing between group 1 and 5 (median OS, 2.5 and 2.6 months), between group 2 and 6 (median OS, 4.7 and 4.5 months), between group 3 and 7 (median OS, 3.6 and 3.2 months) and group 4 and 8 (median OS, 8.0 and 8.2 months), there were no differences in OS depending on TGR of ≥ two-fold. The prognosis of AGC patients receiving nivolumab was found to be influenced by new lesions in different organs and appearance/increase of ascites, not by increase in TGR of ≥ two-fold.
Discussion
The main finding in this study was that the pattern of progression associated with poor prognosis in patients with AGC receiving nivolumab whose best response was PD, was appearance of new lesions in different organs and appearance/increase of ascites, not HPD. Appearance/increase of ascites was a particularly important prognostic factor.
In previous studies, HPD during anti-PD-1/PD-L1 therapy has been observed in 9–29% of patients with various types of cancer [20, 22, 23]. The incidence of HPD in patients with AGC has been reported to be 20–30% [24,25,26] and is associated with poor prognosis. While HPD has also been observed during third-line chemotherapy with irinotecan, the incidence of HPD was found to be higher on nivolumab than on irinotecan and the prognosis was found to be poorer for HPD than for non-HPD in patients on nivolumab but not those on irinotecan [25]. HPD was observed in 16.7% of our patients with AGC treated with nivolumab consistently with previous studies; however, there was no difference in OS between patients with HPD and those with non-HPD. In the ATTRACTION-2 trial which compared nivolumab with placebo as salvage therapy, survival was better from the beginning in the nivolumab group [15] although it is assumed that HPD, if it occurred, might cause more early death in patients receiving nivolumab than in those receiving placebo. Furthermore, a recent report has suggested that disease progression is not more rapid on nivolumab than on placebo [32]. Therefore, it is controversial whether ICIs lead to HPD and poor prognosis in patients with AGC.
Appearance of new lesions was not included in the original definition of HPD, which is based on the sum of the largest diameters of pre-existing measurable lesions. In this study, while new lesions regardless their sites did not have an impact on survival, patients in whom new lesions appeared in different organs had poor prognosis (Supplementary Fig. 1). In contrast, colorectal cancer patients with PD after first-line chemotherapy who developed new lesions regardless the sites were reported to have a significantly poorer prognosis than their counterparts without new lesions [33]. In that study, there was no significant difference in the prognosis between patients with new lesions in different organs and those with new lesions in the pre-existing organs before initiation of chemotherapy. Therefore, debate continues about the clinical significance of the anatomic sites of new lesions. However, in view of previous reports that the number of metastatic sites is a prognostic factor [33] and that progression accompanied by new lesions has a strong negative impact on the prognosis of AGC [27], not including new lesions in the sum of tumor diameters may lead to underestimation of tumor burden. New lesions especially in an organ different from that involved before initiation of nivolumab could be included in the calculation of TGR and HPD in patients with AGC.
Performance status, liver metastases, peritoneal metastases, number of metastatic sites, previous gastrectomy, and the ALP level have been reported to be prognostic factors in patients with AGC on first-line treatment [31, 34, 35]. The peritoneum is one of the most frequent metastatic sites in AGC and becomes increasingly common during the clinical course of the disease. Although peritoneal metastasis is well known to be a poor prognostic factor in AGC, it cannot be measured and is not included in the original definition of HPD. Peritoneal metastasis should be considered when investigating the prognostic impact of the pattern of disease progression in AGC. However, given that it is often difficult to determine progression of peritoneal metastasis objectively, we assessed the appearance/increase of ascites as a surrogate in this study and found that these patients had poor prognosis. Furthermore, in our study, the proportion of patients with appearance/increase of ascites was significantly higher in the group with new lesions in different organs than in the group with new lesions in the same organs (58% [31/53] vs 25% [5/20]; p = 0.0183). We suggest that appearance/increase of ascites is a factor that influences the prognosis in patients with AGC. Appearance/increase of ascites may represent progression of peritoneal metastasis and could be taken into consideration as part of HPD in AGC.
Patients with peritoneal metastasis are reported to derive less benefit from nivolumab as third-line therapy than from placebo [36, 37]. The proportion of Treg cells has been found to be higher among lymphocytes in malignant ascites than in peripheral blood [38]. Patients in our group 4, who had both appearance/increase of ascites and new lesions in different organs had the worst prognosis. These patients tended to have larger tumors, more previous lines of chemotherapy, and a higher NLR at baseline. A previous study found that tumor size correlated with low accumulation of tumor-infiltrating lymphocytes and with poor prognosis in patients with AGC [39], while there is a report that clinical failure on blockade of programmed cell death 1 may result from an imbalance between T-cell reinvigoration and tumor burden in melanoma [40]. The NLR is also a predictor response to chemotherapy. PFS and OS have been found to be significantly shorter in patients with AGC who have a high NLR than in those who have a low NLR [41]. Therefore, multiple adverse prognostic factors are likely to affect the outcome of patients with AGC treated with nivolumab.
While it has been reported that subsequent treatment after failure of nivolumab may have a prognostic impact, most of patients in whom there was an increase in ascites could not receive subsequent chemotherapy after disease progression. Many patients whose overall condition deteriorates after disease progression cannot receive treatment regimens such as irinotecan and TFTD (Supplementary Table 2). Because HPD leading to deterioration of patient’s condition and inability to receive subsequent therapy are confounding, it remains unclear how much impacts on poor prognosis the acceleration of tumor growth by itself and worsening of the patient’s condition unfit for subsequent therapy might have respectively.
New aspects of ICIs are becoming apparent as treatment with these agents evolves. In the KEYNOTE-062 trial, Kaplan–Meier estimates showed that survival during the initial 6–9 months was poorer in patients treated with pembrolizumab monotherapy than in those treated with chemotherapy [42]. However, combination of pembrolizumab with chemotherapy reduced the initial mortality [42]. This finding suggests that combination of chemotherapy with an ICI may prevent HPD. Nevertheless, it is important to know the risks and benefits when choosing an ICI for third-line therapy because ICIs have shown efficacy comparable with that of cytotoxic agents in this setting [43]. In present clinical practice, response evaluation with a short interval and careful observation may detect appearance/ increase of ascites not to miss the appropriate timing for switching to subsequent treatment [35] (Table 3, Supplementary Table 3, 4). Given that there are no established biomarkers of an ICI for AGC, combined positive score may select patients who achieve a substantial survival benefit in the first-line treatment. However, there is no biomarkers for negative selection of non-responders, especially for HPD in ICI monotherapy. Therefore, a clinically relevant definition of HPD is essential not only to clarify clinical risk factors and biomarkers predicting HPD but also to develop new treatment to prevent HPD in near future.
This study had several limitations, which stem mainly from its retrospective design. First, we did not compare patients according to whether they received nivolumab or other cytotoxic chemotherapy (irinotecan, TFTD, or T-DXd). Therefore, it is not clear whether the pattern of disease progression associated with poor prognosis found in this study is specific to nivolumab or common with other cytotoxic chemotherapy. Second, numbers of previous chemotherapy differed among the four groups classified by new lesions in different organs and appearance/increase of ascites (Table 3). Prognosis of patients with 3 or more lines of previous chemotherapy was worse than those with 2 lines (Supplementary Table 5) regardless progression pattern. Previous lines of chemotherapy might be a confounding factor of poor prognosis. However, multivariate analysis showed appearance/increase of ascites is an independent factor for not receiving subsequent chemotherapy. Third, the images used to evaluate TGR were obtained by the attending physician as part of routine clinical practice rather than at protocol-specified time points. Therefore, the time interval between successive CT scans differed among the patients. Finally, we did not analyze biomarkers in tissues and blood, which could lead to the discovery of the mechanism(s) of HPD.
In conclusion, the appearance of new lesions in different organs and appearance/increase of ascites, but not the original definition of HPD based on the TGR of pre-existing measurable lesions, were patterns of disease progression associated with poor prognosis in patients with AGC receiving nivolumab monotherapy whose best response was PD. Assuming that mechanism of disease progression accelerated by ICI are common regardless metastatic sites and measurability of lesions, the clinically relevant definition of HPD, including new lesions and non-measurable lesions, should be considered especially for AGC which metastasizes to the peritoneum frequently.
Abbreviations
- AGC:
-
Advanced gastric cancer
- ALP:
-
Alkaline phosphatase
- CPS:
-
Combined positive score
- CT:
-
Computed tomography
- DCR:
-
Disease control rate
- HER2:
-
Human epidermal growth factor receptor 2
- HPD:
-
Hyperprogressive disease
- HR:
-
Hazard ratio
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- RR:
-
Response rate
- SD:
-
Stable disease
- T-Dxd:
-
Trastuzumab deruxtecan
- TFTD:
-
Trifluridine/tipiracil
- TGR:
-
Tumor growth rate
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Al-Batran SE, Hartmann JT, Probst S, Schmalenberg H, Hollerbach S, Hofheinz R, et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol. 2008;26:1435–42.
Bouche O, Raoul JL, Bonnetain F, Giovannini M, Etienne PL, Lledo G, et al. Randomized multicenter phase II trial of a biweekly regimen of fluorouracil and leucovorin (LV5FU2), LV5FU2 plus cisplatin, or LV5FU2 plus irinotecan in patients with previously untreated metastatic gastric cancer: a Federation Francophone de Cancerologie Digestive Group Study–FFCD 9803. J Clin Oncol. 2004;22:4319–28.
Enzinger PC, Burtness BA, Niedzwiecki D, Ye X, Douglas K, Ilson DH, et al. CALGB 80403 (Alliance)/E1206: a randomized phase ii study of three chemotherapy regimens plus cetuximab in metastatic esophageal and gastroesophageal junction cancers. J Clin Oncol. 2016;34:2736–42.
Kang YK, Kang WK, Shin DB, Chen J, Xiong J, Wang J, et al. Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III noninferiority trial. Ann Oncol. 2009;20:666–73.
Kim GM, Jeung HC, Rha SY, Kim HS, Jung I, Nam BH, et al. A randomized phase II trial of S-1-oxaliplatin versus capecitabine–oxaliplatin in advanced gastric cancer. Eur J Cancer. 2012;48:518–26.
Bang Y-J, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97.
Wilke H, Muro K, Van Cutsem E, Oh S-C, Bodoky G, Shimada Y, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15:1224–35.
Shitara K, Doi T, Dvorkin M, Mansoor W, Arkenau H-T, Prokharau A, et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19:1437–48.
Shitara K, Bang YJ, Iwasa S, Sugimoto N, Ryu MH, Sakai D, et al. Trastuzumab deruxtecan in previously treated HER2-positive gastric cancer. N Engl J Med. 2020;382:2419–30.
Hironaka S, Ueda S, Yasui H, Nishina T, Tsuda M, Tsumura T, et al. Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial. J Clin Oncol. 2013;31:4438–44.
Sym SJ, Hong J, Park J, Cho EK, Lee JH, Park YH, et al. A randomized phase II study of biweekly irinotecan monotherapy or a combination of irinotecan plus 5-fluorouracil/leucovorin (mFOLFIRI) in patients with metastatic gastric adenocarcinoma refractory to or progressive after first-line chemotherapy. Cancer Chemother Pharmacol. 2013;71:481–8.
Thuss-Patience PC, Kretzschmar A, Bichev D, Deist T, Hinke A, Breithaupt K, et al. Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer–a randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur J Cancer. 2011;47:2306–14.
Kang JH, Lee SI, Lim DH, Park KW, Oh SY, Kwon HC, et al. Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone. J Clin Oncol. 2012;30:1513–8.
Kang Y-K, Boku N, Satoh T, Ryu M-H, Chao Y, Kato K, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:2461–71.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–20.
Fuchs CS, Doi T, Jang RW, Muro K, Satoh T, Machado M, et al. Safety and efficacy of pembrolizumab monotherapy in patients with previously treated advanced gastric and gastroesophageal junction cancer: phase 2 clinical KEYNOTE-059 trial. JAMA Oncol. 2018;4: e180013.
Janjigian YY, Shitara K, Moehler M, Garrido M, Salman P, Shen L, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet. 2021;398:27–40.
Champiat S, Dercle L, Ammari S, Massard C, Hollebecque A, Postel-Vinay S, et al. Hyperprogressive disease is a new pattern of progression in cancer patients treated by anti-PD-1/PD-L1. Clin Cancer Res. 2017;23:1920–8.
Gomez-Roca C, Koscielny S, Ribrag V, Dromain C, Marzouk I, Bidault F, et al. Tumour growth rates and RECIST criteria in early drug development. Eur J Cancer. 2011;47:2512–6.
Saada-Bouzid E, Defaucheux C, Karabajakian A, Coloma VP, Servois V, Paoletti X, et al. Hyperprogression during anti-PD-1/PD-L1 therapy in patients with recurrent and/or metastatic head and neck squamous cell carcinoma. Ann Oncol. 2017;28:1605–11.
Ferrara R, Mezquita L, Texier M, Lahmar J, Audigier-Valette C, Tessonnier L, et al. Hyperprogressive disease in patients with advanced non-small cell lung cancer treated with PD-1/PD-L1 inhibitors or with single-agent chemotherapy. JAMA Oncol. 2018;4:1543–52.
Sasaki A, Nakamura Y, Mishima S, Kawazoe A, Kuboki Y, Bando H, et al. Predictive factors for hyperprogressive disease during nivolumab as anti-PD1 treatment in patients with advanced gastric cancer. Gastric Cancer. 2019;22:793–802.
Aoki M, Shoji H, Nagashima K, Imazeki H, Miyamoto T, Hirano H, et al. Hyperprogressive disease during nivolumab or irinotecan treatment in patients with advanced gastric cancer. ESMO Open. 2019;4: e000488.
Takahashi Y, Sunakawa Y, Inoue E, Kawabata R, Ishiguro A, Kito Y, et al. Real-world effectiveness of nivolumab in advanced gastric cancer: the DELIVER trial (JACCRO GC-08). Gastric Cancer. 2021;25:235–44.
Nishikawa K, Yamada Y, Ishido K, Gotoh M, Bando H, Sugimoto N, et al. Impact of progression type on overall survival in patients with advanced gastric cancer based on randomized phase III study of S-1 plus oxaliplatin versus S-1 plus cisplatin. Gastric Cancer. 2017;20:640–5.
Therasse P, Arbuck S, Eisenhauer E, Wanders J, Kaplan R, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–16.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Ferte C, Fernandez M, Hollebecque A, Koscielny S, Levy A, Massard C, et al. Tumor growth rate is an early indicator of antitumor drug activity in phase I clinical trials. Clin Cancer Res. 2014;20:246–52.
Takahari D, Boku N, Mizusawa J, Takashima A, Yamada Y, Yoshino T, et al. Determination of prognostic factors in Japanese patients with advanced gastric cancer using the data from a randomized controlled trial, Japan clinical oncology group 9912. Oncologist. 2014;19:358–66.
Kang YK, Reck M, Nghiem P, Feng Y, Plautz G, Kim HR, et al. Assessment of hyperprogression versus the natural course of disease development with nivolumab with or without ipilimumab versus placebo in phase III, randomized, controlled trials. J Immunother Cancer. 2022;10:e004273.
Shibutani M, Maeda K, Nagahara H, Fukuoka T, Matsutani S, Kashiwagi S, et al. Impact of the occurrence of new lesions on the survival of patients who undergo chemotherapy for metastatic colorectal cancer. Mol Clin Oncol. 2019;10:285–92.
Chau I, Norman AR, Cunningham D, Waters JS, Oates J, Ross PJ. Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer–pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol. 2004;22:2395–403.
Iwasa S, Kudo T, Takahari D, Hara H, Kato K, Satoh T. Practical guidance for the evaluation of disease progression and the decision to change treatment in patients with advanced gastric cancer receiving chemotherapy. Int J Clin Oncol. 2020;25:1223–32.
Kang YK, Morita S, Satoh T, Ryu MH, Chao Y, Kato K, et al. Exploration of predictors of benefit from nivolumab monotherapy for patients with pretreated advanced gastric and gastroesophageal junction cancer: post hoc subanalysis from the ATTRACTION-2 study. Gastric Cancer. 2022;25:207–17.
Pan WT, Zhou SN, Pan MX, Luo QY, Zhang L, Yang DJ, et al. Role of systemic treatment for advanced/metastatic gastric carcinoma in the third-line setting: a Bayesian network analysis. Front Oncol. 2020;10:513.
Yao X, Ajani JA, Song S. Molecular biology and immunology of gastric cancer peritoneal metastasis. Transl Gastroenterol Hepatol. 2020;5:57.
Zhang D, He W, Wu C, Tan Y, He Y, Xu B, et al. Scoring system for tumor-infiltrating lymphocytes and its prognostic value for gastric cancer. Front Immunol. 2019;10:71.
Huang AC, Postow MA, Orlowski RJ, Mick R, Bengsch B, Manne S, et al. T-cell invigoration to tumour burden ratio associated with anti-PD-1 response. Nature. 2017;545:60–5.
Cho IR, Park JC, Park CH, Jo JH, Lee HJ, Kim S, et al. Pre-treatment neutrophil to lymphocyte ratio as a prognostic marker to predict chemotherapeutic response and survival outcomes in metastatic advanced gastric cancer. Gastric Cancer. 2014;17:703–10.
Shitara K, Van Cutsem E, Bang YJ, Fuchs C, Wyrwicz L, Lee KW, et al. Efficacy and safety of pembrolizumab or pembrolizumab plus chemotherapy vs chemotherapy alone for patients with first-line, advanced gastric cancer: the KEYNOTE-062 phase 3 randomized clinical trial. JAMA Oncol. 2020;6:1571–80.
Bang YJ, Ruiz EY, Van Cutsem E, Lee KW, Wyrwicz L, Schenker M, et al. Phase III, randomised trial of avelumab versus physician’s choice of chemotherapy as third-line treatment of patients with advanced gastric or gastro-oesophageal junction cancer: primary analysis of JAVELIN Gastric 300. Ann Oncol. 2018;29:2052–60.
Acknowledgements
We thank all the study participants, physicians, nurses, and staff members who supported this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Shigenori Kadowaki received research grants from Taiho, Lilly, MSD, Chugai, Nobelpharma, Ono, Daiichi Sankyo and Yansen, and honoraria from Lilly, Taiho, Ono, BMS, Chugai, Bayer, Merck Serono, Daiichi Sankyo and Eisai, outside the submitted work. Dr. Naoki Takahashi received honoraria from Taiho, Ono, and Bristol-Myers Squibb, outside the submitted work. Dr. Takayuki Ando received honoraria from Lilly, Taiho, Ono, Daiichi Sankyo and Bristol-Myers Squibb, outside the submitted work. Dr. Yoshiyuki Yamamoto received honoraria from Ono and Merck, outside the submitted work. Dr. Yosuke Kito received honoraria from Taiho, Takeda, Daiichi Sankyo and Merck BioPharma, outside the submitted work. Dr. Toshihiko Matsumoto received honoraria from Lilly, Taiho, Ono, Daiichi Sankyo, Merck and Bristol-Myers Squibb, outside the submitted work. Dr. Michitaka Nagase participated on a data safety monitoring board or advisory board of Chugai, outside the submitted work. Dr. Takao Tamura received research grants from Taiho and Chugai, and honoraria from Ono, Lilly, Takeda and Bristol-Myers Squibb, outside the submitted work. Dr. Taito Esaki received research grants from MSD, Novartis, Dainippon Sumitomo, Ono, Daiichi Sankyo, Astellas, Astellas Amgen Biopharma, Parexel, Chugai, Quintiles, Syneos Health and Pfyzer, and honoraria from MSD, Ono, Daiichi Sankyo, Lilly, Tahio, Chugai and Sanofi, outside the submitted work. Dr. Yuji Miura received honoraria from Astellas, Bristol-Myers Squibb, Eisai, Merck, MSD, Ono and Takeda, outside the submitted work. Dr. Eishi Baba received research grants from Taiho and Chugai, and honoraria from Ono, Chugai, Taiho, Lilly, Daiichi Sankyo, Merck, BMS, Novartis, Janssen, Miyarisan, MSD, Sanofi, Eisai and Takeda, and participated on a data safety monitoring board or advisory board of Daiichi Sankyo, Astellas and AstraZeneca, outside the submitted work. Dr. Akitaka Makiyama received honoraria from Lilly, Taiho, Ono, Daiichi Sankyo and Bristol-Myers Squibb, outside the submitted work. Dr. Kengo Nagashima received consulting fees from Fujimoto, SENJU and Toray Industries, outside the submitted work. Dr. Hirokazu Shoji received honoraria from Ono, and other financial or non-financial interests from Ono, MSD and Astellas, outside the submitted work. Dr. Narikazu Boku received research grants from Takeda and Ono, and honoraria from Taiho, Ono, Daiichi Sankyo and Bristol-Myers Squibb, outside the submitted work. All remaining authors have declared no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10120_2022_1349_MOESM1_ESM.docx
Supplementary file1 Supplementary Figure 1. Kaplan-Meier plots showing overall survival (OS). (a) OS curves after initiation of nivolumab according to whether or not new lesions appeared. Blue lines indicate patients with new lesions and red lines indicate patients with no new lesions. (b) OS curves after initiation of nivolumab according to whether new lesions appeared in different organs or in the same organs. Blue lines indicate patients with new lesions in different organs and red lines indicate patients with new lesions in the same organs (DOCX 60 KB)
10120_2022_1349_MOESM2_ESM.pdf
Supplementary file2 Supplementary Figure 2. Kaplan-Meier plots for overall survival (OS). OS curves after initiation of nivolumab according to presence or absence of an increase in tumor growth rate of ≥ two-fold, new lesions in different organs and appearance/increase of ascites: group 1 [+/+/+], group 2 [+/+/-], group 3 [+/-/+], group 4 [+/-/-], group 5 [-/+/+], group 6 [-/+/-], group 7 [-/-/+] and group 8 [-/-/-]. Red lines indicate patients of group 1, blue lines indicate patients of group 2, green lines indicate patients of group 3, purple lines indicate patients of group 4, orange lines indicate patients of group 5, yellow lines indicate patients of group 6, brown lines indicate patients of group 7 and pink lines indicate patients of group 8 (PDF 375 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aoki, M., Kadowaki, S., Takahashi, N. et al. Pattern of disease progression during third-line or later chemotherapy with nivolumab associated with poor prognosis in advanced gastric cancer: a multicenter retrospective study in Japan. Gastric Cancer 26, 132–144 (2023). https://doi.org/10.1007/s10120-022-01349-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-022-01349-y