Abstract
Photodynamic therapy (PDT) has been suggested as an adjunctive therapeutic approach for peri-implantitis. This systematic review aimed to assess the clinical and radiographic outcomes of adjunctive PDT (aPDT) for the treatment of peri-implantitis among diabetics and cigarette smokers. Randomized controlled trials (RCTs), which assessed the clinical and radiographic outcomes of aPDT versus other intervention(s) and/or MD alone among diabetics and smokers with peri-implantitis, were considered eligible for the review. Meta-analysis was performed for calculating the standard mean difference (SMD) with a 95% confidence interval (CI). The methodological quality of the included studies was evaluated using the modified Jadad quality scale. The meta-analysis revealed no significant differences between the influence of aPDT and other intervention/MD alone on the peri-implant PI among diabetics at the final follow-up. However, statistically significant improvements in the peri-implant PD, BOP, and CBL were observed after the application of aPDT among diabetics. Similarly, no significant differences were found between the influence of aPDT and other interventions/MD alone on the peri-implant PD among smokers with peri-implant diseases at the final follow-up. However, statistically significant improvements in the peri-implant PI, BOP, and CBL were observed after the application of aPDT among smokers. Significant improvements in the peri-implant PD, BOP, and CBL among diabetics and the peri-implant PI, BOP, and CBL among smokers after the application of aPDT at the final follow-up. However, large-scale, well-designed, and long-term RCTs are recommended in this domain.



Similar content being viewed by others
Data availability
All relevant data has been incorporated into the manuscript.
References
Romanos GE, Javed F, Delgado-Ruiz RA, Calvo-Guirado JL (2015) Peri-implant diseases: a review of treatment interventions. Dent Clin 59:157–178
Vohra F, Al-Rifaiy MQ, Lillywhite G, Abu Hassan MI, Javed F (2014) Efficacy of mechanical debridement with adjunct antimicrobial photodynamic therapy for the management of peri-implant diseases: a systematic review. Photochem Photobiol Sci 13:1160–1168
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35:286–291
Lindhe J, Meyle J, Group D of the European Workshop on Periodontology (2008) Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol 35:282–285
ALHarthiAlamryBinShabaib SSNZMS (2022) Effect of multiple sessions of photodynamic therapy on bone regeneration around dental implants among patients with peri-implantitis. Photodiagn Photodyn Ther 37:102612
Bastos M, Tucci M, De Siqueira A, De Faveri M, Figueiredo L, Vallim P et al (2017) Diabetes may affect the expression of matrix metalloproteinases and their inhibitors more than smoking in chronic periodontitis. J Periodont Res 52:292–299
Katz J, Bhattacharyya I, Farkhondeh-Kish F, Perez F, Caudle R, Heft M (2005) Expression of the receptor of advanced glycation end products in gingival tissues of type 2 diabetes patients with chronic periodontal disease: a study utilizing immunohistochemistry and RT-PCR. J Clin Periodontol 32:40–44
Dietrich T, Bernimoulin JP, Glynn RJ (2004) The effect of cigareté smoking on gingival bleeding. J Periodontol 75:16–22
Oates TW, Dowell S, Robinson M, McMahan CA (2009) Glycemic control and implant stabilization in type 2 diabetes mellitus. J Dent Res 88:367–371
Oates TW Jr, Galloway P, Alexander P, Green AV, Huynh-Ba G, Feine J et al (2014) The effects of elevated hemoglobin A1c in patients with type 2 diabetes mellitus on dental implants. J Am Dent Assoc 145:1218–1226
Gómez-Moreno G, Aguilar-Salvatierra A, Rubio Roldán J, Guardia J, Gargallo J, Calvo-Guirado JL (2015) Peri-implant evaluation in type 2 diabetes mellitus patients: a 3-year study. Clin Oral Implants Res 26:1031–1035
Aguilar-Salvatierra A, Calvo-Guirado JL, González-Jaranay M, Moreu G, Delgado-Ruiz RA, Gómez-Moreno G (2016) Peri-implant evaluation of immediately loaded implants placed in esthetic zone in patients with diabetes mellitus type 2: a two-year study. Clin Oral Implants Res 27:156–161
Akram Z, Alqahtani F, Alqahtani M, Al-Kheraif AA, Javed F (2020) Levels of advanced glycation end products in gingival crevicular fluid of chronic periodontitis patients with and without type-2 diabetes mellitus. J Periodontol 91:396–402
Sima C, Glogauer M (2013) Diabetes mellitus and periodontal diseases. Curr DiabRep 13:445–452
Javed F, Al-Hezaimi K, Salameh Z, Almas K, Romanos GE (2011) Proinflammatory cytokines in the crevicular fluid of patients with peri-implantitis. Cytokine 53:8–12
Javed F, AlGhamdi AST, Ahmed A, Mikami T, Ahmed HB, Tenenbaum HC (2013) Clinical efficacy of antibiotics in the treatment of peri-implantitis. Int Dent J 63:169–176
Kotsovilis S, Karoussis IK, Trianti M, Fourmousis I (2008) Therapy of peri-implantitis: a systematic review. J Clin Periodontol 35:621–629
Valderrama P, Blansett JA, Gonzalez MG, Cantu MG, Wilson TG (2014) Suppl 1: detoxification of implant surfaces affected by peri-implant disease: an overview of non-surgical methods. Open Dent J 8:77–84
Garcia-Diaz M, Huang Y-Y, Hamblin MR (2016) Use of fluorescent probes for ROS to tease apart Type I and Type II photochemical pathways in photodynamic therapy. Methods 109:158–166
Horne TK, Cronje MJ (2017) Cancer tissue classification, associated therapeutic implications and PDT as an alternative. Anticancer Res 37:2785–2807
Kataoka H, Nishie H, Hayashi N, Tanaka M, Nomoto A, Yano S et al (2017) New photodynamic therapy with next-generation photosensitizers. Ann Transl Med 5:183
Davanzo NN, Pellosi DS, Franchi LP, Tedesco AC (2017) Light source is critical to induce glioblastoma cell death by photodynamic therapy using chloro-aluminiumphtalocyanine albumin-based nanoparticles. Photodiagn Photodyn Ther 19:181–183
Del Amo FS-L, Yu S-H, Wang H-L (2016) Non-surgical therapy for peri-implant diseases: a systematic review. J Oral Maxillofac Res 7:e13
Schwarz F, Schmucker A, Becker J (2015) Efficacy of alternative or adjunctive measures to conventional treatment of peri-implant mucositis and peri-implantitis: a systematic review and meta-analysis. Int J Implant Dent 1:1–34
Ghanem A, Pasumarthy S, Ranna V, Kellesarian SV, Abduljabbar T, Vohra F et al (2016) Is mechanical curettage with adjunct photodynamic therapy more effective in the treatment of peri-implantitis than mechanical curettage alone? Photodiagn Photodyn Ther 15:191–196
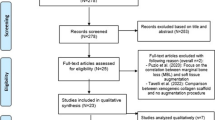
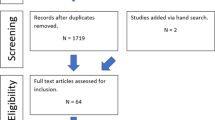
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Stone P (2002) Popping the (PICO) question in research and evidence-based practice. Nurs Res 15:197–198
Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord 12:232–236
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Esposito M, Ardebili Y, Worthington HV (2019) Interventions for replacing missing teeth: different types of dental implants. Cochrane Database of Syst Rev 2019:CD003815
Ahmed P, Bukhari IA, Albaijan R, Sheikh SA, Vohra F (2020) The effectiveness of photodynamic and antibiotic gel therapy as an adjunct to mechanical debridement in the treatment of peri-implantitis among diabetic patients. Photodiagn Photodyn Ther 32:102077
Labban N, Al Shibani N, Al-Kattan R, Alfouzan AF, Binrayes A, Assery MK (2021) Clinical, bacterial, and inflammatory outcomes of indocyanine green-mediated photodynamic therapy for treating periimplantitis among diabetic patients: a randomized controlled clinical trial. Photodiagn Photodyn Ther 35:102350
Alqahtani F, Alqhtani N, Alkhtani F, Divakar DD, Al-Kheraif AA, Javed F (2019) Efficacy of mechanical debridement with and without adjunct antimicrobial photodynamic therapy in the treatment of peri-implantitis among moderate cigarette-smokers and waterpipe-users. Photodiagn Photodyn Ther 28:153–158
Al-Khureif AA, Mohamed BA, Siddiqui AZ, Hashem M, Khan AA, Divakar DD (2020) Clinical, host-derived immune biomarkers and microbiological outcomes with adjunctive photochemotherapy compared with local antimicrobial therapy in the treatment of peri-implantitis in cigarette smokers. Photodiagn Photodyn Ther 30:101684
Al Deeb M, Alresayes S, Mokeem SA, Alhenaki AM, AlHelal A, Vohra F et al (2020) Clinical peri-implant health and biological bone marker levels in tobacco users treated with photodynamic therapy. Photodiagn Photodyn Ther 31:101821
Albaker AM, ArRejaie AS, Alrabiah M, Al-Aali KA, Mokeem S, Alasqah MN et al (2018) Effect of antimicrobial photodynamic therapy in open flap debridement in the treatment of peri-implantitis: a randomized controlled trial. Photodiagn Photodyn Ther 23:71–74
Moher D, Liberati A, Tetzlaff J, Altman DG, Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264-269
Gold SI, Vilardi MA (1994) Pulsed laser beam effects on gingiva. J Clin Periodontol 21:391–396
Radvar M, MacFarlane T, MacKenzie D, Whitters C, Payne A, Kinane D (1996) An evaluation of the Nd: YAG laser in periodontal pocket therapy. Br Dent J 180:57–62
Akram Z, Raffat MA, Shafqat SS, Mirza S, Ikram S (2019) Clinical efficacy of photodynamic therapy as an adjunct to scaling and root planing in the treatment of chronic periodontitis among cigarette smokers: A systematic review and meta-analysis. Photodiagn Photodyn Ther 26:334–341
Shahmohammadi R, Younespour S, Paknejad M, Chiniforush N, Heidari M (2022) Efficacy of Adjunctive Antimicrobial Photodynamic Therapy to Mechanical Debridement in the Treatment of Peri-implantitis or Peri-implant Mucositis in Smokers: A Systematic Review and Meta-analysis. Photochem Photobiol 98:232–241
Zhao Y, Yan Q, Wu X, Hua F, Shi B (2022) The benefit of antimicrobial photodynamic therapy to mechanical debridement in the treatment of smokers with peri-implant diseases: a systematic review and meta-analysis. Lasers Med Sci 37:3051–3066
LeLorier J, Gregoire G, Benhaddad A, Lapierre J, Derderian F (1997) Discrepancies between meta-analyses and subsequent large randomized, controlled trials. New Eng J Med 337:536–452
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
All authors participated in designing the protocol. First, all authors participated in the design of the study. M.K.A. and A.A.A. then did the literature search. M.K.A. and A.A.A. selected the studies and extracted the relevant information, then assessed, and confirmed by the senior author, A.A.A. All authors then participated in synthesizing the data. M.K.A., M.U.Z., A.R., and F.A. also wrote the first draft of the paper. M.K.A. provided critical guidance on the analysis and overall direction of the study. All authors critically revised successive drafts of the paper and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
No ethical approval was required as this manuscript is a review article with no original research data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alam, M.K., Alqahtani, A.A., Zaman, M.U. et al. Clinical and radiographic outcomes of adjunctive photodynamic therapy for treating peri-implantitis among diabetics and cigarette smokers: a systematic review of randomized controlled trials. Lasers Med Sci 38, 142 (2023). https://doi.org/10.1007/s10103-023-03807-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03807-0