Abstract
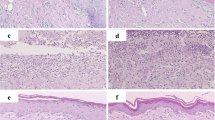
This study aimed to investigate the effects of photobiomodulation at a wavelength of 660 and 830 nm at different numbers of application points in the healing of open wounds in mice. In total, 120 mice were divided into 10 groups. The animals were submitted to cutaneous lesion of the open wound type (1.5 × 1.5 cm). Photobiomodulation at a wavelength of 660 and 830 nm and total energy of 3.6 J were used, applied at 1, 4, 5, and 9 points, for 14 days. The animals were subjected to analysis of the lesion area, skin temperature, and histological analysis. Macroscopic analysis results showed a difference (p < 0.05) between the irradiated groups and the sham group at 14 days PO. There was no statistical difference in skin temperature. Histological analysis findings showed better results for the epidermis thickness. Regarding the number of blood vessels, a difference was found between the 1- and 5-point 830-nm photobiomodulation groups and between the 4-point 660-nm group and the naive group. A significant difference in the number of fibroblasts was observed between the 830- and 660-nm photobiomodulation groups and the naive and sham groups. When comparing photobiomodulation wavelength, the 830-nm groups were more effective, and we emphasize the groups irradiated at 5 points, which showed an improvement in macroscopic analysis and epidermis thickness, an increase in the number of vessels, and a lower number of fibroblasts on the 14th day after skin injury.








Similar content being viewed by others
References
Campos ACL, Borges-Branco A, Groth AK (2007) Cicatrização de feridas. Arq Bras Cir Dig 20:51–58
Shah A, Amini-Nik S (2017) The role of phytochemicals in the inflammatory phase of wound healing. Int J Mol Sci. 18(5):1068. https://doi.org/10.3390/ijms18051068
Lanzafame RJ, Stadler I, Cunningham R, Muhlbauer A, Griggis J, Soltz R, Soltz BA (2013) Preliminary assessment of photoactivated antimicrobial collagen on bioburden in a murine pressure ulcer model. Photomed Laser Surg 31(11):539–546
das Neves LM, Leite GP, Marcolino AM, Pinfildi CE, Garcia SB, Araújo JE, Guirro ECO (2017) Laser photobiomodulation (830 and 660 nm) in mast cells, VEGF, FGF, and CD34 of the musculocutaneous flap in rats submitted to nicotine. Lasers Med Sci 32(2):335–341
Zielins ER, Brett EA, Luan A, Hu MS, Walmsley GG, Paik K, Senarath-Yapa K, Atashroo DA, Wearda T, Lorenz HP, Wan DC, Longaker MT (2015) Emerging drugs for the treatment of wound healing. Expert Opin Emerg Drugs 20(2):235–246
Norman G, Dumville JC, Moore ZE, Tanner J, Christie J, Goto S (2016) Antibiotics and antiseptics for pressure ulcers. Cochrane Database Syst Rev 4:Cd011586
Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA (2008) Treatment of pressure ulcers: a systematic review. Jama. 300(22):2647–2662
Han G, Ceilley R (2017) Chronic wound healing: a review of current management and treatments. Adv Ther 34(3):599–610
Zhang L, Weng C, Zhao Z, Fu X (2017) Extracorporeal shock wave therapy for chronic wounds: a systematic review and meta-analysis of randomized controlled trials. Wound Repair Regen 25(4):697–706
Neves LM, Guirro EC, Albuquerque FL, Marcolino AM (2016) Effects of high-voltage electrical stimulation in improving the viability of musculocutaneous flaps in rats. Ann Plast Surg 77(4):e50–e54
Bora Karsli P, Gurcay E, Karaahmet OZ, Cakci A (2017) High-voltage electrical stimulation versus ultrasound in the treatment of pressure ulcers. Adv Skin Wound Care 30(12):565–570
Khouri C, Kotzki S, Roustit M, Blaise S, Gueyffier F, Cracowski JL (2017) Hierarchical evaluation of electrical stimulation protocols for chronic wound healing: an effect size meta-analysis. Wound Repair Regen 25(5):883–891
Chen B, Kao HK, Dong Z, Jiang Z, Guo L (2017) Complementary effects of negative-pressure wound therapy and pulsed radiofrequency energy on cutaneous wound healing in diabetic mice. Plast Reconstr Surg 139(1):105–117
Nicoletti G, Perugini P, Bellino S, Capra P, Malovini A, Jaber O, Tresoldi M, Faga A (2017) Scar remodeling with the association of monopolar capacitive radiofrequency, electric stimulation, and negative pressure. Photomed Laser Surg 35(5):246–258
Dungel P, Hartinger J, Chaudary S, Slezak P, Hofmann A, Hausner T, Strassl M, Wintner E, Redl H, Mittermayr R (2014) Low-level light therapy by LED of different wavelength induces angiogenesis and improves ischemic wound healing. Lasers Surg Med 46(10):773–780
Machado RS, Viana S, Sbruzzi G (2017) Low-level laser therapy in the treatment of pressure ulcers: systematic review. Lasers Med Sci 32(4):937–944
Karu TI, Pyatibrat LV, Afanasyeva NI (2005) Cellular effects of low power laser therapy can be mediated by nitric oxide. Lasers Surg Med 36:307–314
De Oliveira RF, Oliveira DA, Monteiro W, Zangaro RA, Magini M, Soares CP (2008) Comparison between the effect of low-level laser therapy and low-intensity pulsed ultrasonic irradiation in vitro. Photomed Laser Surg 26(1):6–9
Lins R, Dantas E, Lucena K, Catão M, Granville-Garcia A, Carvalho Neto L (2010) Efeitos bioestimulantes do laser de baixa potência no processo de reparo. An Bras Dermatol. 85(6):849–55. https://doi.org/10.1590/s0365-05962010000600011
Andrade FS, Clark RM, Ferreira ML (2014) Effects of low-level laser therapy on wound healing. Rev Col Bras Cir 41(2):129–133
Sousa RC, Maia Filho AL, Nicolau RA, Mendes LM, Barros TL, Neves SM (2015) Action of AlGaInP laser and high-frequency generator in cutaneous wound healing. A comparative study. Acta Cir Bras 30(12):791–798
de Freitas LF, Hamblin MR (2016) Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron 22(3):1–17. https://doi.org/10.1109/JSTQE.2016.2561201
Freitas APP, Antiorio ATB, Seabra DI (2017) Anestesia e analgesia em animais de laboratório. In: UNICAMP
Guia anestesia e analgesia em animais de laboratório. In: (CEUA), 2017
Schoell AR, Heyde BR, Weir DE, Chiang PC, Hu Y, Tung DK (2009) Euthanasia method for mice in rapid time-course pulmonary pharmacokinetic studies. J Am Assoc Lab Anim Sci 48(5):506–511
Manual de normas do Laboratório de Técnica Operatória e Cirurgia Experimental. In: UFSC, Santa Catarina, ed. 2013
Solmaz H, Dervisoglu S, Gulsoy M, Ulgen Y (2016) Laser biostimulation of wound healing: bioimpedance measurements support histology. Lasers Med Sci 31(8):1547–1554
Uzeda-E-Silva VD, Rodriguez TT, Rocha IA, Xavier FCA, Santos JN, Cury PR, Ramalho LMP (2016) Laser phototherapy improves early stage of cutaneous wound healing of rats under hyperlipidic diet. Lasers Med Sci 31(7):1363–1370
Chiarotto GB, Neves LM, Esquisatto MA, do Amaral ME, dos Santos GM, Mendonca FA (2014) Effects of laser irradiation (670-nm InGaP and 830-nm GaAlAs) on burn of second-degree in rats. Lasers Med Sci 29(5):1685–1693
Rocha Júnior AM, Oliveira RG, Farias RE, Andrade LCF, Aarestrup FM (2006) Modulação da proliferação fibroblástica e da resposta inflamatória pela terapia a laser de baixa intensidade no processo de reparo tecidual. An Bras Dermatol 81:150–156
das Neves LM, Marcolino AM, Prado RP, Ribeiro TS, Pinfildi CE, Thomazini JA (2011) Low-level laser therapy on the viability of skin flap in rats subjected to deleterious effect of nicotine. Photomed Laser Surg 29(8):581–587
Neves LMS, Marcolino AM, Prado RP, Thomazini JA (2011) Laser 830nm na viabilidade do retalho cutâneo de ratos submetidos à nicotina. Acta Ortop Bras 19(6):342–345
Gupta A, Dai T, Hamblin MR (2014) Effect of red and near-infrared wavelengths on low-level laser (light) therapy-induced healing of partial-thickness dermal abrasion in mice. Lasers Med Sci 29(1):257–265
Rathnakar B, Rao BS, Prabhu V, Chandra S, Rai S, Rao ACK, Sharma M, Gupta PK, Mahato KK (2016) Photo-biomodulatory response of low-power laser irradiation on burn tissue repair in mice. Lasers Med Sci 31(9):1741–1750
Sommer AP, Pinheiro AL, Mester AR, Franke RP, Whelan HT (2001) Biostimulatory windows in low-intensity laser activation: lasers, scanners, and NASA’s light-emitting diode array system. J Clin Laser Med Surg 19(1):29–33
Hamblin MR (2018) Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem Photobiol 94(2):199–212
Carroll J (2008) A 3D dose model for low level laser/led therapy biostimulation and bioinhibition. 3 Chap; pp. 327 - 443. In: Hamblin MR, Waynant RW, Anders J. Mechanisms for Low-Light Therapy III. Proc. SPIE 6846. https://doi.org/10.1117/12.771183
Pinfildi CE, Liebano RE, Hochman BS, Ferreira LM (2005) Helium-neon laser in viability of random skin flap in rats. Lasers Surg Med 37(1):74–77
Prado RP, Pinfildi CE, Liebano RE, Hochman BS, Ferreira LM (2009) Effect of application site of low-level laser therapy in random cutaneous flap viability in rats. Photomed Laser Surg 27(3):411–416
Pinfildi CE, Hochman BS, Nishioka MA, Sheliga TR, Neves MAI, Liebano RE, Ferreira LM (2013) What is better in TRAM flap survival: LLLT single or multi-irradiation? Lasers Med Sci 28(3):755–761. https://doi.org/10.1007/s10103-012-1130-3
Martignago CCS, Tim CR, Assis L, Neves LMG, Bossini PS, Renno AC, LIebano RE, Parizotto N (2018) Comparison of two different laser photobiomodulation protocols on the viability of random skin flap in rats. Lasers Med Sci 34:1041–1047. https://doi.org/10.1007/s10103-018-2694-3
Goncalves RV, Novaes RD, Matta SL, Benevides GP, Faria FR, Pinto MV (2010) Comparative study of the effects of gallium-aluminum-arsenide laser photobiomodulation and healing oil on skin wounds in Wistar rats: a histomorphometric study. Photomed Laser Surg 28(5):597–602
Goncalves RV, Novaes RD, Cupertino Mdo C, Moraes B, Leite JPV, Peluzio MCG, Pinto MVM, Patta LP (2013) Time-dependent effects of low-level laser therapy on the morphology and oxidative response in the skin wound healing in rats. Lasers Med Sci 28(2):383–390. https://doi.org/10.1007/s10103-012-1066-7
Carneiro C, Schleder JC, Fischer SV, Zedebski RAM, Verner AF, Lipinski L (2015) Efeito de lasers de baixa potência no reparo de lesões cutâneas. Publicatio uepg Ciências biológicas e da saúde (online) 21:109–115
Yadav A, Gupta A (2017) Noninvasive red and near-infrared wavelength-induced photobiomodulation: promoting impaired cutaneous wound healing. Photodermatol Photoimmunol Photomed 33(1):4–13
Gal P, Vidinsky B, Toporcer T, Mokrý M, Mozes S, Longauer F, Sabo J (2006) Histological assessment of the effect of laser irradiation on skin wound healing in rats. Photomed Laser Surg 24(4):480–488
Leite GP, das Neves LM, Silva CA, Guirro RRJ, Souza TR, Souza AK, Garcia SB, Guirro ECO (2017) Photobiomodulation laser and pulsed electrical field increase the viability of the musculocutaneous flap in diabetic rats. Lasers Med Sci 32(3):641–648. https://doi.org/10.1007/s10103-017-2160-7
Melo VA, Anjos DCS, Albuquerque Júnior R, Melo DB, Carvalho FUR (2011) Effect of low level laser on sutured wound healing in rats. Acta Cir Bras 26:129–134. https://doi.org/10.1590/s0102-86502011000200010
Wagner VP, Curra M, Webber LP, Nor C, Matte U, Meurer L, Martins MD (2016) Photobiomodulation regulates cytokine release and new blood vessel formation during oral wound healing in rats. Lasers Med Sci 31(4):665–671. https://doi.org/10.1007/s10103-016-1904-0
Medeiros AC, Dantas-Filho AM (2017) Cicatrização das feridas cirúrgicas. J Surg Clin Res 7(2):87–102. https://doi.org/10.20398/jscr.v7i2.11438
Gonçalves RV, Mezêncio JMS, Benevides GP, Matta SLP, Neves CA, Sarandy MM, Vilela EF (2010) Effect of gallium-arsenide laser, gallium-aluminum-arsenide laser and healing ointment on cutaneous wound healing in Wistar rats. Braz J Med Biol Res 43:350–355. https://doi.org/10.1590/S0100-879X2010007500022
Sampaio SCPO, Monteiro JSC, Cangussu MCT, Santos GMP, Santos MAV, Santos JN, Pineiro ALB (2013) Effect of laser and LED phototherapies on the healing of cutaneous wound on healthy and iron-deficient Wistar rats and their impact on fibroblastic activity during wound healing. Lasers Med Sci 28(3):799–806. https://doi.org/10.1007/s10103-012-1161-9
Chaves ME, Araujo AR, Piancastelli AC, Pinotti M (2014) Effects of low-power light therapy on wound healing: LASER × LED. An Bras Dermatol 89(4):616–623
Solmaz H, Ulgen Y, Gulsoy M (2017) Photobiomodulation of wound healing via visible and infrared laser irradiation. Lasers Med Sci 32(4):903–910
Christensen J, Matzen LH, Vaeth M, Schou S, Wenzel A (2012) Thermography as a quantitative imaging method for assessing postoperative inflammation. Dentomaxillofac Radiol 41(6):494–499
Dostalova T, Kroulikova V, Podzimek S, Jelinkova H (2017) Low-level laser therapy after wisdom teeth surgery: evaluation of immunologic markers (secretory immunoglobulin a and lysozyme levels) and thermographic examination: placebo controlled study. Photomed Laser Surg 35(11):616–621
Carvalho A, Bizo MHA, Toma HS, Guedes KMR, Muraro LS, Musis C (2017) Effect of gallium arsenide low-level laser therapy on the inflammatory phase of skin wound healing in rats. Acta Vet Bras 11(4):226–230. https://doi.org/10.21708/avb.2017.11.4.7274
Funding
This research was funded by the Coordination for Improvement of Higher Education Personnel (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-CAPES). Financial support was received for the master’s student.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee (CEUA) under number 4017201117.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hendler, K.G., Canever, J.B., de Souza, L.G. et al. Comparison of photobiomodulation in the treatment of skin injury with an open wound in mice. Lasers Med Sci 36, 1845–1854 (2021). https://doi.org/10.1007/s10103-020-03216-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03216-7