Abstract
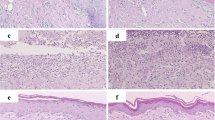
Many studies have been conducted on the treatment of burns because they are important in morbidity and mortality. These studies are mainly focused on improving care and quality of life of patients. The aim of this study was evaluate the LED phototherapy effects in rats skin full-thickness burns induced by CO2 laser. The animals were divided in NT group that did not received any treatment and LED group that received LED irradiation at 685 nm, 220 mW, and 4.5 J/cm2 during 40 s by burned area. Biopsies were obtained after 7, 14, and 21 days of treatment and submitted to histological and immunohistochemical analysis. The LED phototherapy shows anti-inflammatory effects, improves angiogenesis, and stimulates the migration and proliferation of fibroblasts. The T CD8+ lymphocytes were more common in burned areas compared to T CD4+ lymphocytes since statistically significant differences were observed in the LED group compared to the NT group after 7 days of treatment. These results showed that LED phototherapy performs positive influence in full-thickness burns repair from the healing process modulated by cellular immune response. The obtained results allowed inferring that burns exhibit a characteristic cell immune response and this cannot be extrapolated to other wounds such as incision and wounds induced by punch, among others.




Similar content being viewed by others
References
Vale ECS (2005) Primeiro atendimento em queimaduras: A abordagem do dermatologista. An Bras Dermatol 80(1):9–19. https://doi.org/10.1590/S0365-05962005000100003
Silva VCC (2006) O efeito do laser de baixa potência (658nm) na reparação tecidual de queimaduras de terceiro grau em ratos. Dissertation, Vale of the Paraiba University
Chiari A, Fernandes MC, Negrini F, Oliveira J, Mesquita RA (2007) Hidroterapia e exercícios respiratórios associados à massoterapia na reabilitação de pacientes com queimaduras acometendo a região torácica. Fisioter Bras 8(6):441–447
Leão CRG, Andrade ES, Fabrini DS, Oliveira RA, Machado GLB, Gontijo LC (2011) Epidemiologia das queimaduras no estado de Minas Gerais. Rev Bras Cir Plast 26(4):573–577. https://doi.org/10.1590/S1983-51752011000400006
Alrawi M, Crowley T, Pape S (2014) Bacterial colonization of the burn wound: a UK experience. J Wound Care 23(5):274–277. https://doi.org/10.12968/jowc.2014.23.5.274
Orban C, Tomescu D (2013) The importance of early diagnosis of sepsis in severe burned patients: outcomes of 100 patients. Chirurgia (Bucur) 108(3):385–388
Hrynyk M, Neufeld RJ (2014) Insulin and wound healing. Burns 40(8):1443–1446. https://doi.org/10.1016/j.burns.2014.03.020
World Health Organization (2011) Burn prevention: sucess stories and lessons learned. World Library Catologuing in Publication, Geneva 100p
Peck MD (2011) Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 37(7):1087–1100. https://doi.org/10.1016/j.burns.2011.06.005
Fiório FB, Albertini R, Leal-Júnior ERP, Carvalho PT (2014) Effect of low-level laser therapy on types I and III collagen and inflammatory cells in rats with induced third-degree burns. Lasers Med Sci 29:313–319. https://doi.org/10.1007/s10103-013-1341-2
Chiarotto GB, Neves LMG, Esquisatto MAM, Amaral MEC, Santos GMT, Mendonça FAS (2014) Effects of laser irradiation (670-nm InGaP and 830-nm GaAlAs) on burn of second-degree in rats. Lasers Med Sci 29(5):1685–1693. https://doi.org/10.1007/s10103-014-1573-9
Desmet KD, Paz DA, Corry JJ, Eells JT, Wong-Riley MT, Henry MM, Buchmann EV, Connelly MP, Dovi JV, Liang HL, Henshel DS, Yeager RL, Millsap DS, Lim J, Gould LJ, Das R, Jett M, Hodgson BD, Margolis D, Whelan HT (2006) Clinical and experimental applications of NIRLED photobiomodulation. Photomedicine Laser Surg 24(2):121–128. https://doi.org/10.1089/pho.2006.24.121
Meyer PF, Araújo HG, Carvalho MGF, Tatum BIS, Fernandes ICAG, Ronzio OA, Pinto MVM (2010) Avaliação dos efeitos do LED na cicatrização de feridas cutâneas em ratos Wistar. Fisioter Bras 11(6):428–432
Kerppers II, Lima CJ, Fernandes AB, Villaverde AB (2015) Effect of light-emitting diode (ʎ 627 nm and 945 nm ʎ) treatment on first intention healing: immunohistochemical analysis. Lasers Med Sci 30:397–401. https://doi.org/10.1007/s10103-014-1668-3
Opel DR, Hagstrom E, Pace AK, Sisto K, Hirano-Ali AS, Desai S, Swan J (2015) Light-emitting diodes: a brief review and clinical experience. J Clin Aesthet Dermatol 8(6):36–44
Sampaio SCO, Monteiro JSC, Cangussú MC, Santos GMP, Santos MA, Santos JN, Pinheiro AL (2013) Effect of laser and LED phototherapies on the healing of cutaneous wound on healthy and iron-deficient Wistar rats and their impact on fibroblastic activity during wound healing. Lasers Med Sci 28(3):799–806. https://doi.org/10.1007/s10103-012-1161-9
Chaves MEA, Araújo AR, Piancastelli ACC, Pinotti M (2014) Effects of low-power light therapy on wound healing: LASER x LED. An Bras Dermatol 89(4):616–623. https://doi.org/10.1590/abd1806-4841.20142519
Siqueira CPCM, Filho DOT, Lima FM, Silva FP, Durante H, Dias IFL, Duarte JL, Kashimoto RK, Castro VAB (2009) Efeitos biológicos da luz: aplicação de terapia de baixa potência empregando LEDs (Light Emitting Diode) na cicatrização da úlcera venosa: relato de caso. Semina Cien Biol Saude 30(1):37–46
Melo MS, Alves LP, Navarro RS, Lima CJ, Munin E, Vilela-Goulart MG, Gomes MF, Salgado MAC, Zângaro RA (2014) Experimental full-thickness burns induced by CO2 laser. Lasers Med Sci 29(5):1709–1714. https://doi.org/10.1007/s10103-014-1585-5
Alves DB, Tozeti IA, Gatto FA, Cassandri F, Ferreira AMT, Fernandes CES, Falcão GR, Scapulatempo IDL, Padovani CTJ, Abdo MAGS (2010) Linfócitos CD4 e CD8 e células NK no estroma da cérvice uterina de mulheres infectadas pelo papilomavírus humano. Rev Soc Bras Med Trop 43(4):425–429. https://doi.org/10.1590/S0037-86822010000400018
Dornelas MT, Rodrigues MF, Machado DC, Gollner AM, Ferreira AP (2009) Expressão de marcadores de proliferação celular e apoptose no carcinoma espinocelular de pele e ceratose actínica. An Bras Dermatol 84(5):469–475. https://doi.org/10.1590/S0365-05962009000500004
Fiório FB, Silveira L Jr, Munin E, Lima CJ, Fernandes KP, Mesquita-Ferrari RA, Carvalho PT, Lopes-Martins RA, Aimbire F, Carvalho RA (2011) Effect of incoherent LED radiation on third degree burning wounds in rats. J Cosmet Laser Ther 13(6):315–322. https://doi.org/10.3109/14764172.2011.630082
Neves SM, Nicolau RA, Maia Filho ALM, Mendes LM, Veloso AM (2014) Digital photogrammetry and histomorphometric assessment of the effect of non-coherent light (light-emitting diode) therapy (λ640±20 nm) on the repair of third-degree burns in rats. Lasers Med Sci 29:203–212. https://doi.org/10.1007/s10103-013-1312-7
Filho GB (1998) Bogliolo: Patologia Geral. Guanabara Koogan, Rio de Janeiro
Catão MHCV, Costa RO, Nonaka CFW, Albuquerque Júnior RLC, Costa IRRS (2016) Green LED light has anti-inflammatory effect on burns in rats. Burns 42:392–396. https://doi.org/10.1016/j.burns.2015.07.003
Ilkovitch D (2011) Role of immune-regulatory cells in skin pathology. J Leukoc Biol 89:41–49. https://doi.org/10.1189/jlb.0410229
Blotnick S, Peoples GE, Freeman MR, Erbelein TJ, Klagsbrun M (1994) T lymphocytes synthesize and export heparin-binding epidermal growth factor-like growth factor and basic fibroblast growth factor, mitogens for vascular cells and fibroblasts: differential production and release by CD4+ and CD8+ T cells. Cell Biology. Proc Nati Acad Sci USA 91:2890–2894
Dall Agnol MA, Nicolau RA, Lima CJ, Munin E (2009) Comparative analysis of coherent light action (laser) versus non-coherent light (light-emitting diode) for tissue repair in diabetic rats. Lasers Med Sci 24:909–916. https://doi.org/10.1007/s10103-009-0648-5
Corazza AV, Jorge J, Kurachi C, Bagnato VS (2007) Photobiomodulation on the angiogenesis of skin wounds in rats using different light sources. Photomed Laser Surg 25(2):102–106. https://doi.org/10.1089/pho.2006.2011
Sousa AP, Paraguassú GM, Silveira NT, Souza J, Cangussú MC, Santos JN, Pinheiro AL (2013) Laser and LED phototherapies on angiogenesis. Lasers Med Sci 28(3):981–987. https://doi.org/10.1007/s10103-012-1187-z
Catão MHV, Nonaka CF, Albuquerque RL, Bento PM, Costa RO (2015) Effects of red laser, infrared, photodynamic therapy and green LED on the healing process of third-degree burns: clinical and histological study in rats. Lasers Med Sci 30(1):421–428. https://doi.org/10.1007/s10103-014-1687-0
Meireles GC, Santos JN, Chagas PO, Moura AP, Pinheiro AL (2008) A comparative study of the effects of laser photobiomodulation on the healing of third-degree burns: a histological study in rats. Photomed Laser Surg 26(2):159–166. https://doi.org/10.1089/pho.2007.2052
Buchanan IB, Maile R, Frelinger JA, Fair JH, Meyer AA, Cairns BA (2006) The effect of burn injury on CD8+ and CD4+ T cells in an irradiation model of homeostatic proliferation. J Trauma 61:1062–1068. https://doi.org/10.1097/01.ta.0000195984.56153.21
Kokhaei P, Barough MS, Hassan ZM (2014) Cimetidine effects on the immunosuppression induced by burn injury. Int Immunopharmacol 22(1):273–276. https://doi.org/10.1016/j.intimp.2014.07.003
Davis PA, Corless DJ, Aspinall R, Wastell C (2001) Effect of CD4+ e CD8+ cell depletion on wound healing. Br J Surg 88:298–304. https://doi.org/10.1046/j.1365-2168.2001.01665.x
Chen L, Mehta ND, Zhao Y, DiPietro LA (2014) Absence of CD4 or CD8 lymphocytes changes infiltration of inflammatory cells and profiles of cytokine expression in skin wounds, but does not impair healing. Exp Dermatol 23:189–194. https://doi.org/10.1111/exd.12346
Acknowledgments
Milene da Silva Melo thanks the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, São Paulo, Brazil/Process no. 09/53509-2) for the doctoral scholarship.
Renato Amaro Zângaro thanks the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, São Paulo, Brazil/Process no. 11/50468-3) for the financial support to the equipment and consumables.
Funding
This study is supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Processes No. 09/53509-2 and 11/50468-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures in the animals of this study were in accordance with the ethical standards and were carried out with the approval of the Research Ethics Committee of the São José dos Campos Dental School, Institute of Science and Technology of the Paulista State University (ICT-UNESP), São José dos Campos, SP, Brazil (Protocol No 10/2011-PA/CEP).
Rights and permissions
About this article
Cite this article
da Silva Melo, M., Alves, L.P., Fernandes, A.B. et al. LED phototherapy in full-thickness burns induced by CO2 laser in rats skin. Lasers Med Sci 33, 1537–1547 (2018). https://doi.org/10.1007/s10103-018-2515-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2515-8