Abstract
Objectives
Little is known about efficacy and safety of ethanol lock therapy (ELT) to treat totally implantable venous access device (TIVAD) infections. The objective of this trial was to evaluate the effectiveness and safety profile of a local treatment with ELT without removal for TIVAD infection due to coagulase-negative staphylococci.
Methods
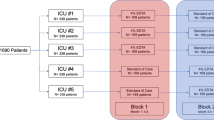
We performed a prospective, multicenter, double-blind, randomized clinical trial comparing the efficacy of 40% ELT versus vancomycin lock therapy (VLT) in TIVAD infections due to coagulase-negative staphylococci, complicated or not by bloodstream infection.
Results
Thirty-one patients were assigned to the ELT group and 30 to the VLT arm. Concomitant bacteremia was present in 41 patients (67.2%). Treatment success was 58.1 % (18 of 31) for the ELT arm and 46.7% (14 of 30) for the VLT arm (p = 0.37). The overall treatment success was 52.5% (32). The risk of treatment failure due to uncontrolled infections, superinfections, and mechanical complications did not differ significantly between participants receiving ELT (13 out of 31 [42%]) and those receiving VLT (16 out of 30 [53%]) with a hazard ratio of 0.70 (p = 0.343; 95% CI [0.34–1.46], Cox model). Catheter malfunctions were significantly more frequent in the ELT arm (11 patients versus 2 in the VLT group, p = 0.01).
Conclusions
We found an overall high rate of treatment failure that did not differ between the ELT arm and the VLT arm. TIVAD removal must be prioritized to prevent complications (uncontrolled infections, superinfections, and catheter malfunctions) except in exceptional situations.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to risk of individual privacy compromission but are available from the corresponding author on reasonable request
Abbreviations
- TIVADs:
-
totally implantable venous access devices
- ELT:
-
ethanol lock therapy
- VLT:
-
vancomycin lock therapy
- CRBSI:
-
catheter-related bloodstream infection
- CoNS:
-
coagulase-negative staphylococci
References
Walser EM (2012) Venous access ports: indications, implantation technique, follow-up, and complications. Cardiovasc Intervent Radiol 35:751–764. https://doi.org/10.1007/s00270-011-0271-2
Pinelli F, Cecero E, Degl’Innocenti D, Selmi V, Giua R, Villa G, Chelazzi C, Romagnoli S, Pittiruti M (2018) Infection of totally implantable venous access devices: a review of the literature. J Vasc Access 19:230–242. https://doi.org/10.1177/1129729818758999
Gapany C, Tercier S, Diezi M, Clement C, Lemay K, Joseph J-M (2011) Frequent accesses to totally implanted vascular ports in pediatric oncology patients are associated with higher infection rates. J Vasc Access 12:207–210. https://doi.org/10.5301/JVA.2011.6258
Dibb M, Lal S (2017) Home parenteral nutrition: vascular access and related complications. Nutr Clin Pract 32:769–776. https://doi.org/10.1177/0884533617734788
Wang TY, Lee KD, Chen PT, Chen MC, Chen YY, Huang CE, Kuan FC, Chen CC, Lu CH (2015) Incidence and risk factors for central venous access port-related infection in Chinese cancer patients. J Formos Med Assoc 114:1055–1060. https://doi.org/10.1016/j.jfma.2015.06.013
Shim J, Seo T-S, Song MG, Cha I-H, Kim JS, Choi CW, Seo JH, Oh SC (2014) Incidence and risk factors of infectious complications related to implantable venous-access ports. Korean J Radiol 15:494–500. https://doi.org/10.3348/kjr.2014.15.4.494
Zerati AE, Figueredo TR, de Moraes RD, da Cruz AM, da Motta-Leal Filho JM, Freire MP, Wolosker N, de Luccia N (2016) Risk factors for infectious and noninfectious complications of totally implantable venous catheters in cancer patients. J Vasc Surg Venous Lymphat Disord 4:200–205. https://doi.org/10.1016/j.jvsv.2015.10.008
Lebeaux D, Fernández-Hidalgo N, Chauhan A, Lee S, Ghigo J-M, Almirante B, Beloin C (2014) Management of infections related to totally implantable venous-access ports: challenges and perspectives. Lancet Infect Dis 14:146–159. https://doi.org/10.1016/S1473-3099(13)70266-4
Laporte-Amargos J, Sastre E, Bergas A, Pomares H, Paviglianiti A, Rodriguez-Arias M, Pallares N, Badia-Tejero AM, Pons-Oltra P, Carratalà J, Gudiol C (2023) Increasing gram-negative catheter-related bloodstream infection in cancer patients. Pathogens 12:228. https://doi.org/10.3390/pathogens12020228
Flynn PM, Willis B, Gaur AH, Shenep JL (2003) Catheter design influences recurrence of catheter-related bloodstream infection in children with cancer. J Clin Oncol 21:3520–3525. https://doi.org/10.1200/JCO.2003.03.012
Aumeran C, Guyot P, Boisnoir M, Robin-Hennequin C, Vidal M, Forestier C, Traore O, Lesens O, Clermont-Ferrand Biofilm Study Group (2013) Activity of ethanol and daptomycin lock on biofilm generated by an in vitro dynamic model using real subcutaneous injection ports. Eur J Clin Microbiol Infect Dis 32:199–206. https://doi.org/10.1007/s10096-012-1732-5
Morales M, Méndez-Alvarez S, Martín-López J-V, Marrero C, Freytes CO (2004) Biofilm: the microbial “bunker” for intravascular catheter-related infection. Support Care Cancer 12:701–707. https://doi.org/10.1007/s00520-004-0630-5
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJA, Sherertz RJ, Warren DK (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49:1–45. https://doi.org/10.1086/599376
Rijnders BJ, Van Wijngaerden E, Vandecasteele SJ, Stas M, Peetermans WE (2005) Treatment of long-term intravascular catheter-related bacteraemia with antibiotic lock: randomized, placebo-controlled trial. J Antimicrob Chemother 55:90–94. https://doi.org/10.1093/jac/dkh488
Raad I, Hanna H, Dvorak T, Chaiban G, Hachem R (2007) Optimal antimicrobial catheter lock solution, using different combinations of minocycline, EDTA, and 25-percent ethanol, rapidly eradicates organisms embedded in biofilm. Antimicrob Agents Chemother 51:78–83. https://doi.org/10.1128/AAC.00154-06
Chambers ST, Pithie A, Gallagher K, Liu T, Charles CJ, Seaward L (2007) Treatment of Staphylococcus epidermidis central vascular catheter infection with 70% ethanol locks: efficacy in a sheep model. J Antimicrob Chemother 59:779–782. https://doi.org/10.1093/jac/dkl542
Balestrino D, Souweine B, Charbonnel N, Lautrette A, Aumeran C, Traoré O, Forestier C (2009) Eradication of microorganisms embedded in biofilm by an ethanol-based catheter lock solution. Nephrol Dial Transplant 24:3204–3209. https://doi.org/10.1093/ndt/gfp187
Sofroniadou S, Revela I, Kouloubinis A, Makriniotou I, Zerbala S, Smirloglou D, Kalocheretis P, Drouzas A, Samonis G, Iatrou C (2017) Ethanol combined with heparin as a locking solution for the prevention of catheter related blood stream infections in hemodialysis patients: a prospective randomized study. Hemodial Int 21:498–506. https://doi.org/10.1111/hdi.12524
Schoot RA, van Ommen CH, Stijnen T, Tissing WJE, Michiels E, Abbink FCH, Raphael MF, Heij HA, Lieverst JA, Spanjaard L, Zwaan CM, Caron HN, van de Wetering MD (2015) Prevention of central venous catheter-associated bloodstream infections in paediatric oncology patients using 70% ethanol locks: a randomised controlled multi-centre trial. Eur J Cancer 51:2031–2038. https://doi.org/10.1016/j.ejca.2015.06.126
Salonen BR, Bonnes SL, Vallumsetla N, Varayil JE, Mundi MS, Hurt RT (2018) A prospective double blind randomized controlled study on the use of ethanol locks in HPN patients. Clin Nutr 37:1181–1185. https://doi.org/10.1016/j.clnu.2017.05.009
Souweine B, Lautrette A, Gruson D, Canet E, Klouche K, Argaud L, Bohe J, Garrouste-Orgeas M, Mariat C, Vincent F, Cayot S, Cointault O, Lepape A, Guelon D, Darmon M, Vesin A, Caillot N, Schwebel C, Boyer A et al (2015) Ethanol lock and risk of hemodialysis catheter infection in critically ill patients. A randomized controlled trial. Am J Respir Crit Care Med 191:1024–1032. https://doi.org/10.1164/rccm.201408-1431OC
Broom JK, Krishnasamy R, Hawley CM, Playford EG, Johnson DW (2012) A randomised controlled trial of Heparin versus EthAnol Lock THerapY for the prevention of Catheter Associated infecTion in Haemodialysis patients--the HEALTHY-CATH trial. BMC Nephrol 13:146. https://doi.org/10.1186/1471-2369-13-146
Pérez-Granda MJ, Barrio JM, Muñoz P, Hortal J, Rincón C, Rabadán PM, Pernia MS, Bouza E (2014) Ethanol lock therapy (E-Lock) in the prevention of catheter-related bloodstream infections (CR-BSI) after major heart surgery (MHS): a randomized clinical trial. PLoS One 9:e91838. https://doi.org/10.1371/journal.pone.0091838
Lopes BC, Borges PSGN, Gallindo RM, Tenório TBS, Machado LB, de Orange FA (2019) Ethanol lock therapy for the prevention of nontunneled catheter-related bloodstream infection in pediatric patients. JPEN J Parenter Enteral Nutr 43:1044–1052. https://doi.org/10.1002/jpen.1508
Worth LJ, Slavin MA, Heath S, Szer J, Grigg AP (2014) Ethanol versus heparin locks for the prevention of central venous catheter-associated bloodstream infections: a randomized trial in adult haematology patients with Hickman devices. J Hosp Infect 88:48–51. https://doi.org/10.1016/j.jhin.2014.06.007
Slobbe L, Doorduijn JK, Lugtenburg PJ, El Barzouhi A, Boersma E, van Leeuwen WB, Rijnders BJA (2010) Prevention of catheter-related bacteremia with a daily ethanol lock in patients with tunnelled catheters: a randomized, placebo-controlled trial. PLoS One 5:e10840. https://doi.org/10.1371/journal.pone.0010840
Wolf J, Connell TG, Allison KJ, Tang L, Richardson J, Branum K, Borello E, Rubnitz JE, Gaur AH, Hakim H, Su Y, Federico SM, Mechinaud F, Hayden RT, Monagle P, Worth LJ, Curtis N, Flynn PM (2018) Treatment and secondary prophylaxis with ethanol lock therapy for central line-associated bloodstream infection in paediatric cancer: a randomised, double-blind, controlled trial. Lancet Infect Dis 18:854–863. https://doi.org/10.1016/S1473-3099(18)30224-X
Khosroshahi HT, Mahdipur H, Parkhideh S, Basmenji S, Khalilzadeh M, Tozihi M (2015) The effectiveness of systemic antibiotic therapy with and without ethanol-locked solution in the treatment of hemodialysis-related catheter infection. Saudi J Kidney Dis Transpl 26:477–481. https://doi.org/10.4103/1319-2442.157315
Mermel LA, Farr BM, Sherertz RJ, Raad II, O’Grady N, Harris JS, Craven DE, Infectious Diseases Society of America, American College of Critical Care Medicine, Society for Healthcare Epidemiology of America (2001) Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis 32:1249–1272. https://doi.org/10.1086/320001
Kurul S, Saip P, Aydin T (2002) Totally implantable venous-access ports: local problems and extravasation injury. Lancet Oncol 3:684–692. https://doi.org/10.1016/s1470-2045(02)00905-1
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, REDCap Consortium (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Wolf J, Shenep JL, Clifford V, Curtis N, Flynn PM (2013) Ethanol lock therapy in pediatric hematology and oncology. Pediatr Blood Cancer 60:18–25. https://doi.org/10.1002/pbc.24249
Buonsenso D, Salerno G, Sodero G, Mariani F, Pisapia L, Gelormini C, Di Nardo M, Valentini P, Scoppettuolo G, Biasucci DG (2022) Catheter salvage strategies in children with central venous catheter-related or -associated bloodstream infections: a systematic review and meta-analysis. J Hosp Infect 125:1–20. https://doi.org/10.1016/j.jhin.2022.03.010
Mermel LA, Alang N (2014) Adverse effects associated with ethanol catheter lock solutions: a systematic review. J Antimicrob Chemother 69:2611–2619. https://doi.org/10.1093/jac/dku182
Guenu S, Heng A-E, Charbonné F, Galmier M-J, Charlès F, Deteix P, Souweine B, Lartigue C (2007) Mass spectrometry and scanning electron microscopy study of silicone tunneled dialysis catheter integrity after an exposure of 15 days to 60% ethanol solution. Rapid Commun Mass Spectrom 21:229–236. https://doi.org/10.1002/rcm.2837
Msakni N, Galmier M-J, Couret M-J, Szczepaniak C, Bouchon B, Souweine B, Lartigue C (2013) Complementary mass spectrometric approaches and scanning electron microscopy to study the structural stability of polyurethane tunneled dialysis catheters after exposure to ethanol solutions. Rapid Commun Mass Spectrom 27:2343–2354. https://doi.org/10.1002/rcm.6691
Calvet L, Piot M, Lartigue C, Souweine B, Tardy-Poncet B (2015) Anticoagulant properties of enoxaparin 400 IU/mL-40% ethanol catheter lock solution. Springerplus 4:746. https://doi.org/10.1186/s40064-015-1533-2
Balestrino D, Quintana M, Charbonnel N, Forestier C, Lartigue C, Souweine B (2016) Compatibility of injectable anticoagulant agents in ethanol; in vitro antibiofilm activity and impact on polyurethane catheters of enoxaparin 400 U/mL in 40% v/v ethanol. PLoS One 11:e0159475. https://doi.org/10.1371/journal.pone.0159475
Schilcher G, Schlagenhauf A, Schneditz D, Scharnagl H, Ribitsch W, Krause R, Rosenkranz AR, Stojakovic T, Horina JH (2013) Ethanol causes protein precipitation--new safety issues for catheter locking techniques. PLoS One 8:e84869. https://doi.org/10.1371/journal.pone.0084869
Acknowledgements
We thank our microbiologist colleagues Julien Delmas and Frédéric Robin for their technical assistance. We thank Dr. Natacha Mrozek, Dr. Magali Vidal, Dr. Clément Théis, and Delphine Martineau for their participation.
Funding
The research protocol was accepted for funding by an Inter-Regional Hospital Clinical Research Program (PHRC-IR Auvergne-Rhône-Alpes).
Author information
Authors and Affiliations
Contributions
O.L. contributed to the study conception and design. Data collection was performed by all the other authors. The first draft of the manuscript was written by O.L. and L.S., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the CPP Sud-Est VI ethics committee n°AU 1120, the CNIL (French Data Protection Authority) n°1223379, and the ANSM (National Drug Agency) and registered under the ClinicalTrials.gov Identifier number NCT02411331.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lesens, O., Forestier, E., Botelho-Nevers, E. et al. Comparing ethanol lock therapy versus vancomycin lock in a salvation strategy for totally implantable vascular access device infections due to coagulase-negative staphylococci (the ETHALOCK study): a prospective double-blind randomized clinical trial. Eur J Clin Microbiol Infect Dis 43, 223–232 (2024). https://doi.org/10.1007/s10096-023-04702-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04702-w