Abstract
Purpose
To elucidate the role of the Klebsiella oxytoca species complex (KoSC) in epidemiology of VIM-type MBL-producing Enterobacterales in Poland.
Methods
The study comprised all 106 VIM-positive KoSC isolates collected by the Polish National Reference Centre for Susceptibility Testing during 2009–2019 from 60 institutions in 35 towns. All isolates were sequenced by Illumina MiSeq, followed by MinION sequencing of selected organisms. Genomes were subjected to bioinformatic analysis, addressing taxonomy, clonality, phylogeny and structural characterisation of key resistance determinants within their chromosomal and plasmidic loci.
Results
Among five species identified, K. oxytoca was predominant (n = 92), followed by Klebsiella michiganensis (n = 11). MLST distinguished 18 STs, with the most prevalent Klebsiella oxytoca ST145 (n = 83). The clone segregated a lineage with the In237-like integron [blaVIM-1–aacA4 genes; n = 78], recorded in 28 cities almost all over the country. The integron was located in a ~ 49–50 kb chromosomal mosaic region with multiple other resistance genes, linked to a ~ 51 kb phage-like element. The organism might have originated from Greece, and its evolution in Poland included several events of chromosomal ~ 54–258 kb deletions, comprising the natural β-lactamase blaOXY gene. A group of other isolates of various species and clones (n = 12) carried the integron In916 on self-transmissible IncA-type plasmids, effectively spreading in Italy, France and Poland.
Conclusion
KoSC has been one of the major VIM producers in Poland, owing largely to clonal expansion of the specific K. oxytoca–In237-like lineage. Its apparently enhanced epidemic potential may create a danger on international scale.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carbapenemase-producing Enterobacterales (CPE) are considered to be largely responsible for the current antimicrobial resistance (AMR) crisis around the world [1]. One of their critically important groups is metallo-β-lactamase (MBL) producers, including those with VIM-type enzymes. Initially, these were described in Pseudomonas spp. in the mid-1990s, followed soon by Enterobacterales [2, 3]. In general, the VIM-type carbapenemases are encoded by gene cassettes usually of class 1 integrons that in enterobacteria are located on a variety of plasmids and only occasionally in the chromosome. The first successful VIM CPE country-wide spread in Europe was observed in Greece in the early 2000s, leading to endemic situation with numerous host species, VIM variants and their genetic determinants [4,5,6]. Soon, regional or interregional dissemination of such organisms has been reported in other European countries, including Spain, Italy or Hungary [6,7,8,9].
The first VIM-producing Enterobacterales isolate in Poland, Klebsiella pneumoniae, was confirmed in 2006 by the National Reference Centre for Susceptibility Testing (NRCST) in Warsaw [10]. Till the end of 2012, 118 VIM CPE isolates were reported, with predominance of Enterobacter spp. (n = 64; 54.2%), followed by Klebsiella oxytoca (n = 23; 19.5%) [11]. Since then, annual numbers of VIM CPE multiplied, resulting in a total of 927 isolates from 2006 to 2019 [12]. Although surpassed by K. pneumoniae in recent years, the K. oxytoca species complex (KoSC) has remained to be a highly relevant fraction of VIM CPE, ranking third among the taxonomic groups (n = 106; 11.4%). Here, we report the genomic analysis of all VIM-producing KoSC isolates, collected from the first identification in 2009 till the end of 2019, being part of a comprehensive WGS study of all Polish VIM CPE confirmed by the NRCST in 2006–2019.
Materials and methods
Bacterial isolates, WGS and species identification
The study comprised 106 non-duplicate VIM-producing KoSC isolates from 105 patients, collected by the NRCST during the CPE surveillance in Poland from 2009 to 2019 (Table S1) [12]. The isolates were from 60 centres in 35 cities of all 16 main administrative regions. The majority of the isolates were detected in the region Mazowieckie (n = 56; 52.8%) and often in Warsaw (n = 34; 32.1%). Around a half of the isolates were recovered from infections (n = 52; 49.1%), mainly of the urinary tract (n = 27; 25.5%) and wounds (n = 15; 14.1%), and most of the remaining ones were from carriage (n = 53; 50.0%). The KoSC isolates were tested for the carbapenemase presence by CARBA NP [13], phenotypic and PCR tests [14] and sequenced by MiSeq (Illumina, San Diego, CA, USA), with reads assembled with SPAdes 3.15.5 [15]. Four isolates, representing predominant blaVIM-carrying integron types, were subjected to long-read sequencing by MinION (Oxford Nanopore Technologies, Oxford, UK). The MiSeq and MinION hybrid assemblies were done with Unicycler v.0.4.8 [16]. Species identification was based on average nucleotide identity (ANI) scores, using FastANI v.1.32 with ≥ 95% cutoff [17] and RefSeq reference genomes.
MLST, clonal and phylogenetic analyses, characterisation of bla OXYgenes
MLST was performed by the mlst tool (https://github.com/tseemann/mlst). The in-sample clonality SNP analysis was done by BioNumerics v.7.6.3 (Applied Maths NV, Sint-Martens-Latem, Belgium). The SNP-based phylogenetic analysis in the international context was performed with all 271 KoSC genomes available in RefSeq as of the 1st of February 2023, using Parsnp v.1.5.4 (https://github.com/marbl/parsnp). Phylotrees were visualised by iTOL (https://itol.embl.de). Variants of the intrinsic KoSC β-lactamase blaOXY genes were identified using the BIGSdb database (https://bigsdb.pasteur.fr/klebsiella/). Broader blaOXY-containing genomic regions were studied using the progressive Mauve algorithm [18].
Integrons with bla VIMgenes and their chromosomal and plasmid context; resistomes andantimicrobial susceptibility
The composition of blaVIM-carrying integrons was characterised manually using Geneious Prime v.2022.0.1 (Biomatters, Auckland, New Zealand) and BLASTn. Chromosomal loci containing blaVIM-carrying integrons and blaOXY deletions were analysed using Mauve [18]; PHASTER [19] was applied to identify phage-like elements. Plasmid replicon types were identified by ABRicate using PlasmidFinder database [20]. The structural analysis of plasmids was executed using BLASTn and visualised by BRIG (http://brig.sourceforge.net/). Easyfig v.2.2.5 (http://mjsull.github.io/Easyfig/) was used to illustrate specific structures of the chromosome or plasmids with AMR genes. Acquired AMR genes (resistomes) were detected using ResFinder database, with the 99.5% identity criterion [21]. Susceptibility to 19 antimicrobials was tested for 23 representative KoSC isolates by broth microdilution, using Sensititre™ Gram Negative EUMDRXXF AST (Thermo Fisher Scientific, Waltham, MA, USA), MICRONAUT-S Pseudomonas MIC (Bruker Daltonics, Bremen, Germany), ComASP® cefiderocol (Liofilchem, Roseto degli Abruzzi, Italy) and aztreonam-avibactam in-house plates. EUCAST breakpoints (http://eucast.org) were used for interpretation of the results.
Serotypes and virulence genes
Identification of putative virulence determinants: capsule (CPS, K) and lipopolysaccharide (LPS, O) loci and yersiniabactin and kleboxymycin biosynthesis gene clusters was performed using Kaptive [22], Kleborate [23], Geneious Prime v.2022.0.1 and BLASTn as described previously [24].
Results
Taxonomy, clonality and bla OXYgenes
Five different KoSC species were detected among the 106 isolates: K. oxytoca (n = 92; 86.8%), K. michiganensis (n = 11, 10.4%) and K. grimontii, K. pasteurii and K. spallanzanii (n = 1; 0.9% each) (Table S1). The isolates were classified into 18 distinct STs, including five novel ones, with ten and six STs assigned to K. oxytoca and K. michiganensis, respectively (K. spallanzanii is not included in the MLST scheme) (Table S1). The K. oxytoca population was dominated vastly by ST145 (n = 83; 90.2% and 78.3% of K. oxytoca and all KoSC isolates, respectively). The occurrence of the remaining STs was marginal, including 13 STs with single isolates only.
Six phylogroups of the blaOXY gene were congruent with the taxonomic distribution, with lineage 2 characteristic for K. oxytoca and lineages 1 and 5 for K. michiganensis (Table S1) [25, 26]. A total of 17 gene alleles were distinguished, which in general correlated well with STs. The most abundant was the blaOXY-2–22 variant (n = 59; 55.7% of all KoSC), observed only in the K. oxytoca ST145 isolates; however, a remarkable fraction of this clone (n = 24; 22.6% of all KoSC) were blaOXY negative (confirmed by PCR [25]; addressed below).
bla VIMvariants and bla VIM -carrying integrons
Four blaVIM gene variants were detected, three of which represented the blaVIM-1 lineage: blaVIM-1 (n=96; 90.6%), blaVIM-4 (n=7; 6.6%) and the novel blaVIM-79 (n=1; 0.9%) (Table S1). The remaining blaVIM-2 genes were sporadic (n=2; 1.9%). Altogether, nine blaVIM-carrying integrons were found, with predominance of In237-like elements (blaVIM-1; n=81, 76.4% in total), followed by In916 (blaVIM-1; n=13; 12.3%), and In238, In238a and In238-79 together (blaVIM-4/-79; n=8; 7.5% in total) (Tables S1 and S2). The In237-like integron differs from In237 by two SNPs at positions 60 and 68 in the blaVIM-1 attC site [11]. The In238a element differs from In238 by not having a specific 169-bp duplication at the 3′-end of the blaVIM cassette (present also in In238-79, In237 and In237-like elements) [11, 27, 28], whereas In238-79 differs from In238 by one point mutation converting blaVIM-4to blaVIM-79.
Epidemiology, clonality and phylogeny of the K. oxytoca ST145 clone
In the study period, the predominant K. oxytoca ST145 clone (n = 83) was recorded in 46 hospitals in 28 towns of 14/16 Polish administrative regions, mainly Mazowieckie (n = 49; 59.0% of ST145) with Warsaw (n = 28) (Figure S1A). The vast majority of the ST145 isolates carried the In237-like integron (n = 78 in total; 93.9%); few isolates had In916 or In238-like elements (n = 4; 4.8%, and n = 1; 1.2%, respectively).
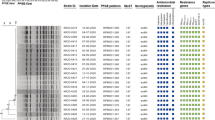
All of the ST145 isolates were subjected to the SNP-based clonal comparative analysis that revealed 1446 polymorphic positions within 4.9 Mb (78%) of the reference genome, characterising the original VIM-producing ST145 isolate from 2009 (isolate NMI776/09 with the In237-like integron). SNP numbers between any individual isolate and the reference ranged from 14 to 126 SNPs (Table S3). However, the 78 isolates with the In237-like element formed a distinct cluster with 0–69 SNPs between each other, indicating clonal outbreak, separated clearly from the remaining five isolates with In916 or In238 integrons (Figure S1B). The further in-depth investigation of the outbreak isolates has split them into those with the natural β-lactamase blaOXY gene (allele blaOXY-2–22; n = 59) and those lacking the gene (n = 24). The comparison of all blaOXY-negative genomes with the ‘oldest’ ST145-In237-like blaOXY-positive isolate (isolate NMI2092/09) revealed that blaOXY negatives have arisen from a series of chromosomal deletions, ranging from ~ 54 to ~ 258 kb (Table S4). The majority of the deletions characterised single isolates, and the phylogenetic ST145 analysis revealed these to be distributed across the phylotree, indicating mainly independent and unique character of the deletions (Fig. 1). However, some identical or similar in size deletions (~ 152 kb, ~ 159–161 kb and ~ 216 kb) were observed in multiple isolates each, and the analysis showed these to form clusters of closely related isolates, demonstrating spread of some of the blaOXY-negative sublineages, combined with further modifications of the original deletions.
SNP-based phylogenetic tree of Polish K. oxytoca ST145 isolates compared with all international ST145 genomes available in RefSeq. Numbers on the inner circle are the original numbers of the study isolates or RefSeq assembly numbers. The presence of carbapenemases is indicated in the outer circles using corresponding colours. Country symbols: CN, China; ES, Spain; GB, Great Britain; PL, Poland; US, USA. The tree was constructed using Parsnp and visualised with iTOL
The phylogenetic analysis of all 83 Polish and eight international ST145 genomes identified in RefSeq has separated the outbreak ST145-In237-like isolates from those with the In916 or In238 integrons and the isolates from other countries (China, n = 5; and the UK, USA and Spain, n = 1 each) (Fig. 1). Of note, a single isolate from China (GCF_002265085) was the only other blaOXY-negative ST145 record found in RefSeq; however, the lack of blaOXY was observed also in isolates of ST2 from the UK (GCA_022432685) and undefined ST from South Africa (GCF_015694225).
Phylogeny of minor STs
Only seven of the remaining STs identified in Polish KoSC were represented in the RefSeq database. A single VIM-1-positive K. oxytoca ST2 isolate was related to a Spanish VIM-1 producer (229 SNPs; another blaVIM integron), and both were located on the main branch of the ST2 phylotree, along with multiple other isolates from European countries mainly (Figure S2). The other STs had only few RefSeq genomes each (results not shown).
Acquired AMR genes and susceptibility patterns
Seventy-one acquired AMR gene profiles were defined in the study isolates, with 4–19 genes per genome and a mean of 11.1 (Table S1). The AMR gene content varied even within the ST145-In237-like outbreak cluster, presenting 46 gene profiles, each with up to 17 isolates. The only AMR genes common for all of the outbreak isolates were blaVIM-1 and aacA4 of the In237-like integrons. Apart from other aminoglycoside resistance genes, all or most of the outbreak isolates carried the AmpC-like cephalosporinase gene blaCMY-31 (91.0%) and genes of resistance to sulphonamides (100%), trimethoprim (91.0%) and phenicols (69.2%).
Twenty-three isolates (including four ST145-In237-like outbreak organisms), representing all species, STs and various resistomes, were subjected to susceptibility testing. All these showed AMR phenotypes correlating well with the resistomes, and in general, the isolates were not extensively drug resistant (Table S5). Levels of resistance to carbapenems varied, and the majority of the isolates were susceptible or susceptible at increased exposure to meropenem (and, consistently, its combination with vaborbactam). All of the isolates had low MICs of aztreonam with avibactam, and all but one were susceptible to cefiderocol. Aminoglycosides (amikacin and gentamicin) and quinolones (especially levofloxacin) were active in vitro against the majority of the organisms, and all isolates were fully susceptible to colistin.
Chromosomal AMR locus with the In237-like integron in the outbreak ST145 clone
The previous, standard molecular biology study has assigned the In237-like integron to the chromosome of the early K. oxytoca ST145 outbreak isolates, 2009–2012 [11]. The present analysis has confirmed that observation and revealed details of the In237-like chromosomal loci. Two outbreak isolates, namely the first blaOXY-positive and blaOXY-negative isolates NMI2092/09 and NMI776/09, respectively, used as references in the clonal analyses described above, were long-read sequenced. The examination of the NMI2092/09 isolate has shown the In237-like integron to reside in a Tn21-like mercury resistance transposon, truncated by IS26 and located within a unique ~ 52 kb mosaic region (MR) with multiple other mobile elements (Fig. 2). The MR contained also eight additional AMR genes (Table S1), including blaCMY-31 within an ISEcp1 transposition module, and it followed directly a ~ 51 kb phage-like segment, ‘Phage 1’, identified by PHASTER to be intact but of no extensive identity to any phage known. The entire ‘Phage 1’–MR structure was inserted into a tRNAArg gene with a partial, 45 bp duplication, placed ~ 29.5 kb downstream of the blaOXY-2–22 gene. The blaOXY-negative NMI776/09 isolate also contained a ‘Phage 1’–MR combo in the tRNAArg gene, sharing ~ 49.6 kb of MR with NMI2092/09, with the In237-like-Tn21 truncated by IS4321. Interestingly, another phage-like structure of ~ 34 kb, ‘Phage 2’, plus additional ~ 12 kb of unknown origin was identified directly behind the MR, and the comparison with the NMI2092/09 genome revealed that this entire region has replaced ~ 83 kb of the original K. oxytoca chromosome, comprising blaOXY.
Genetic context of the chromosomal AMR islands and adjacent regions in the blaOXY-positive isolate NMI2092/09 and blaOXY-negative isolate NMI776/09, compared to the corresponding loci with tRNAArg and blaOXY genes loci in the K. oxytoca RefSeq reference strain FDAARGOS 500 (GenBank accession number CP033844). The entire fragment compared is flanked by the tRNAArg gene (K. oxytoca FDAARGOS 500 locus tag EGY21_24185) and fimbrial protein genes (locus tags EGY21_24550 and EGY21_24555). Arrows indicate all CDSs proportionally to their sizes and orientation; the only selected genes or mobile elements are marked with colours and/or names. The shaded areas between linear structures indicate homologous regions and the level of their sequence identity. The Tn21-like structures with the In237-like integron are enlarged below the chromosomal comparisons using dotted lines
‘Phage 1’ was identified in all of the Polish ST145-In237-like outbreak and five ST145-In916/In238 non-outbreak isolates and in 5/8 international ST145 isolates from Spain, the USA and China, indicating no strict correlation between this structure and the MR with the In237-like-Tn21 element. It was inserted always in the tRNAArg gene, but as revealed in two long-read sequenced non-outbreak ST145-In916/In238 isolates (NMI253/19 and NMI2990/17; described below), their ‘Phage 1’ was shorter (~ 48 kb) and had no any AMR region associated. Otherwise, apart from the NMI776/09 isolate, ‘Phage 2’ was detected in two isolates only, both blaOXY positive, and not in any other isolate with the blaOXY deletion.
Plasmid profiles; bla VIM -carrying plasmids
At least one of 23 different plasmid replicon types was detected in 64 isolates of all STs (60.4%), producing profiles of 0–5 replicons per isolate (Table S6). The 42 isolates with no or no typeable plasmid belonged exclusively to the ST145 outbreak cluster with chromosomal In237-like elements.
Detailed structure of plasmids with blaVIM-carrying integrons was revealed for two long-read sequenced non-outbreak K. oxytoca ST145 isolates, having In916 (isolate NMI253/19) or In238 (NMI2990/17). In916 was identified on a ~ 134 kb IncA-type plasmid (p253A). The comparative analysis of p253A against public sequence databases showed its high identity to the previously published In916-harbouring IncA plasmids p743A, p7753A, p5955A and p9546_2 from Polish Enterobacter spp. or K. pneumoniae [12, 29], as well as a series of such plasmids from Italian Enterobacterales [30], and Dutch Aeromonas sp. (MH220284) (Figure S3). Main differences between all these plasmids arose from multiple rearrangements within the AMR mosaic region, containing a IS26–blaSHV-12–In916–IS26 module, described originally in Italy [30]. In p253A, this region was significantly smaller than in the previously published plasmids (~ 23 kb versus ~ 37.8 to ~ 51.8 kb, respectively), had less AMR genes and no mercury resistance operon and was flanked by ISKpn19-like elements on both sides (Figure S4).
In238 was located in the NMI2990/17 isolate on a ~ 23 kb plasmid (p2990) of unknown replicon. The BLASTn-based comparison revealed its low overall similarity (coverage, ~ 35%; identity, > 99%) to few international plasmids only. p2990 comprised regions encoding plasmid replication and stability, conjugal transfer (TraK, J-like and TrbJ, K, L-like families) and type I and II toxin-antitoxin systems (ptaRNA1-, RelE/StbE- and VapC-families) (results not shown).
The analysis of the short-read data for the remaining isolates with the likely plasmidic location of blaVIM integrons was not able to associate these elements with individual plasmids in a number of these. It demonstrated In916 to reside on IncA-type plasmids in all other isolates with this integron (n = 12), regardless the species and ST (Table S6). The only other case was the K. oxytoca ST2 isolate with In238-79 (blaVIM-79) which was assigned to an IncM1-like plasmid.
Serotypes and virulence genes
The CPS K-antigen biosynthesis locus was identified sporadically (n = 5, 4.7%), whereas that of the LPS O-antigen was common (n = 104; 98.1%), with four variants detected (Table S6). The entire K. oxytoca ST145 clone and single ST2, ST346 and ST347 isolates were characterised by OL104. The yersiniabactin locus was observed broadly (n = 94; 88.7%), including all K. oxytoca organisms (Table S6). The kleboxymycin biosynthesis gene cluster was detected less frequently (n = 40; 37.7%), being present in various genotypes, including 27 K. oxytoca ST145-In237-like outbreak isolates (Table S6).
Discussion
KoSC has been an important producer of VIM-like MBLs in Poland, occupying the third position among all VIM CPE from 2006 to 2019 (11.3%), behind Enterobacter spp. (40.1%) and the K. pneumoniae species complex, KpSC (23.1%) [12]. The VIM-positive KoSC population has been mainly K. oxytoca itself (86.8%), which then to a similar extent has been dominated by the ST145-In237-like lineage (84.8%). Its clonal expansion has been one of the most spectacular phenomena in epidemiology of VIM CPE in Poland so far.
Originally recorded in 2009, subsequently, the K. oxytoca ST145-In237-like genotype has spread first in three provinces, mainly the central Mazowieckie with Warsaw [11], and then almost all over the country. It has had several specific characteristics, rarely or not observed in other Polish VIM CPE. The In237-like integron is a member of the In238 type, multiple variants of which have been identified in Enterobacterales and other Gram-negative rods in Poland and mid-Southern Europe since the 1990/2000s [11, 27, 28, 31, 32]. This individual element had been found originally in Escherichia coli from 2001 in Greece, the first VIM CPE ever reported [27], and in Poland, it has been recorded since 2009 mainly in the K. oxytoca ST145 outbreak lineage so far [11, 12, 32]. The second distinct feature of the genotype has been the location of the integron with its Tn21-like transposon inside the chromosomal MR linked to the putative phage, ‘Phage 1’. ‘Phage 1’ has been common in ST145 genomes, including those having no MRs with In237-like integrons, and both the scenario and mechanisms of acquisition of these individual elements remain unclear. Moreover, apart from the In237-like cassettes, the MR carried up to nine other AMR genes, with the uncommon blaCMY-31, conferring multi-drug resistance (MDR) altogether. This single chromosomal island was the major or even the only AMR source in the outbreak isolates which is rare in Enterobacterales, exploiting plasmids as main AMR genetic platforms. Overall, the isolates showed similarity to VIM-1 + CMY-31-producing K. oxytoca isolates from community-onset infections in Greece from 2005 to 2007, including the identical blaOXY allele [33]. This indicated the likely origin of the ST145-In237-like lineage; however, the Greek strains have not been typed by MLST, and their genomes seem to have not been sequenced or available.
The other interesting observation regarding the epidemic ST145-In237-like genotype referred to the frequent chromosomal deletions containing blaOXY genes, observed in 30.8% of the outbreak isolates. The blaOXY genes encode intrinsic KoSC-specific β-lactamases, estimated to have evolved along with individual phylogenetic lineages over approximately 100 million years [25, 26]. The blaOXY deletions have been found only in three other KoSC genomes deposited in the international databases, including one ST145 from China. Therefore, it is possible that these might have been occurring preferentially in the ST145 genetic background, which is supported also by multiplicity of independent deletion events in the study isolates. The detailed structural analysis of the index blaOXY-negative ST145-In237-like isolate suggested that the deletion could have been caused by the other putative phage (‘Phage 2’), inserted in the neighbourhood of the ‘Phage 1’–MR (In237-like) locus, and that there might have been an association between various rearrangements in this peculiar part of the genome. However, the lack of ‘Phage 2’ in other blaOXY-negative isolates excluded the hypothesis of a single deletion mechanism and has left the phenomenon of the repetitive deletions without explanation.
The second, though less important factor of the blaVIM genes’ spread in the Polish KoSC population were In916-carrying IncA-type plasmids, observed in four non-outbreak ST145 isolates and nine isolates of various species/STs, documenting horizontal transmission. In contrast to other European countries where In916 has been associated with several plasmid incompatibility groups such as IncA, IncFIIK, IncHI2 or IncN [34,35,36], in Poland, the integron has been found exclusively on IncA plasmids so far. These have been of high identity rates to those analysed in Italy [12, 29], indicating the actual origin and large-scale, successful expansion of these molecules among Enterobacterales in Europe.
In contrast to KpSC, the knowledge on KoSC virulence factors and their genetic determinants has been scarce so far. Reports on those have been usually based on homologous sequences, being extrapolations of the KpSC data, and non-including evidence from functional studies [24, 37]. Similarly, the study isolates have been checked only for the presence of several putative virulence determinants. Like in other recent studies [24, 38], the CPS K-antigen locus was of low incidence (~ 7.3%), in contrast to the LPS O-antigen biosynthesis locus (~ 97.2%) and the siderophore yersiniabactin ybt loci (88.7%). However, despite the high nucleotide sequence identity to the KpSC ybt loci, those in KoSC had different genetic context and no identifiable mobility-associated genes [39]. The gene cluster of the best-known KoSC-specific virulence factor, i.e. the toxin kleboxymycin, involved in the antibiotic-associated haemorrhagic colitis (AAHC) [40,41,42], was recorded in ~ 42% of the isolates. These were mainly K. oxytoca but also K. michiganensis, K. grimontii and K. pasteurii, and similar to the observations of Long et al., the cluster was absent in K. spallanzanii, possibly not causing the AAHC [38].
Although limited to the single country, this work has provided a remarkable amount of broader scale relevant data on epidemiology and genetics of KoSC, especially K. oxytoca, which has rarely been an object of specific studies. K. oxytoca has been a significant opportunistic pathogen and reservoir of AMR genes, and in Polish hospitals, it has been one of the most important producers of VIM-type carbapenemases. The critical part of our study concerned the K. oxytoca ST145-In237-like outbreak lineage of the most likely Greek origin, which since 2009 has been disseminating over the almost entire Poland’s territory. The detailed genomic analysis has revealed a number of specific characteristics of the organism, including the chromosomal MDR island carrying the In237-like integron and the blaCMY-31 cephalosporinase gene. The epidemic potential of the lineage creates a risk of its further expansion into other regions in Europe.
Data availability
Genomic sequences have been deposited in the NCBI under the BioProject number PRJNA983967, https://www.ncbi.nlm.nih.gov/bioproject/PRJNA983967, and BioSample numbers SAMN35742457-35,742,562. Plasmid sequences have been assigned the following accession numbers: p253A, OR232699 and p2990, OR232700.
Code availability
Not applicable.
References
Lee CS, Doi Y (2014) Therapy of infections due to carbapenem-resistant Gram-negative pathogens. Infect Chemother 46(3):149–164
Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL (2012) Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev 25(4):682–707
Walsh TR, Toleman MA, Poirel L, Nordmann P (2005) Metallo-β-lactamases: the quiet before the storm? Clin Microbiol Rev 18(2):306–325
Psichogiou M, Tassios PT, Avlamis A, Stefanou I, Kosmidis C, Platsouka E, Paniara O, Xanthaki A, Toutouza M, Daikos GL, Tzouvelekis LS (2008) Ongoing epidemic of blaVIM-1-positive Klebsiella pneumoniae in Athens, Greece: a prospective survey. J Antimicrob Chemother 61(1):59–63
Miriagou V, Douzinas EE, Papagiannitsis CC, Piperaki E, Legakis NJ, Tzouvelekis LS (2008) Emergence of Serratia liquefaciens and Klebsiella oxytoca with metallo-β-lactamase-encoding IncW plasmids: further spread of the blaVIM-1-carrying integron In-e541. Int J Antimicrob Agents 32(6):540–541
Canton R, Akova M, Carmeli Y, Giske CG, Glupczynski Y, Gniadkowski M, Livermore DM, Miriagou V, Naas T, Rossolini GM, Samuelsen O, Seifert H, Woodford N, Nordmann P (2012) Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect 18(5):413–431
Albiger B, Glasner C, Struelens MJ, Grundmann H, Monnet DL (2015) European survey of carbapenemase-producing Enterobacteriaceae working g (2015) carbapenemase-producing Enterobacteriaceae in Europe: assessment by national experts from 38 countries. Euro Surveill 20(45):pii=30062. https://doi.org/10.2807/1560-7917.ES.2015.20.45.30062
Nordmann P, Poirel L (2014) The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect 20(9):821–830
Oteo J, Ortega A, Bartolome R, Bou G, Conejo C, Fernandez-Martinez M, Gonzalez-Lopez JJ, Martinez-Garcia L, Martinez-Martinez L, Merino M, Miro E, Mora M, Navarro F, Oliver A, Pascual A, Rodriguez-Bano J, Ruiz-Carrascoso G, Ruiz-Garbajosa P, Zamorano L, Bautista V, Perez-Vazquez M, Campos J (2015) Prospective multicenter study of carbapenemase-producing Enterobacteriaceae from 83 hospitals in Spain reveals high in vitro susceptibility to colistin and meropenem. Antimicrob Agents Chemother 59(6):3406–3412
Sekowska A, Gospodarek E, Kruszynska E, Hryniewicz W, Gniadkowski M, Duljasz W, Kusza K, Wawrzyniak K (2010) First isolation of metallo-β-lactamase producing Klebsiella pneumoniae strain in Poland. Anestezjol Intens Ter 42(1):27–30
Izdebski R, Baraniak A, Żabicka D, Sękowska A, Gospodarek E, Hryniewicz W, Gniadkowski M (2018) VIM/IMP carbapenemase-producing Enterobacteriaceae in Poland: epidemic Enterobacter hormaechei and Klebsiella oxytoca lineages. J Antimicrob Chemother 73(10):2675–2681
Izdebski R, Biedrzycka M, Urbanowicz P, Żabicka D, Gniadkowski M (2023) Genome-based epidemiologic analysis of VIM/IMP carbapenemase-producing Enterobacter spp., Poland. Emerg Infect Dis 29(8):1618–1626
Nordmann P, Poirel L, Dortet L (2012) Rapid detection of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 18(9):1503–1507
Baraniak A, Machulska M, Zabicka D, Literacka E, Izdebski R, Urbanowicz P, Bojarska K, Herda M, Kozinska A, Hryniewicz W, Gniadkowski M, Group N-PS (2019) Towards endemicity: large-scale expansion of the NDM-1-producing Klebsiella pneumoniae ST11 lineage in Poland, 2015–16. J Antimicrob Chemother 74(11):3199–3204
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, Pyshkin AV, Sirotkin AV, Vyahhi N, Tesler G, Alekseyev MA, Pevzner PA (2012) SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19(5):455–477
Wick RR, Judd LM, Gorrie CL, Holt KE (2017) Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol 13(6):e1005595
Jain C, Rodriguez RL, Phillippy AM, Konstantinidis KT, Aluru S (2018) High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat Commun 9(1):5114. https://doi.org/10.1038/s41467-018-07641-9
Darling AC, Mau B, Blattner FR, Perna NT (2004) Mauve: multiple alignment of conserved genomic sequence with rearrangements. Genome Res 14(7):1394–1403
Arndt D, Grant JR, Marcu A, Sajed T, Pon A, Liang Y, Wishart DS (2016) PHASTER: a better, faster version of the PHAST phage search tool. Nucleic Acids Res 44(W1):W16-21
Carattoli A, Zankari E, Garcia-Fernandez A, Voldby Larsen M, Lund O, Villa L, Moller Aarestrup F, Hasman H (2014) In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother 58(7):3895–3903
Zankari E, Hasman H, Cosentino S, Vestergaard M, Rasmussen S, Lund O, Aarestrup FM, Larsen MV (2012) Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother 67(11):2640–2644
Wick RR, Heinz E, Holt KE, Wyres KL (2018) Kaptive Web: user-friendly capsule and lipopolysaccharide serotype prediction for Klebsiella genomes. J Clin Microbiol 56(6):e00197-e218
Lam MMC, Wick RR, Watts SC, Cerdeira LT, Wyres KL, Holt KE (2021) A genomic surveillance framework and genotyping tool for Klebsiella pneumoniae and its related species complex. Nat Commun 12(1):4188. https://doi.org/10.1038/s41467-021-24448-3
Stewart J, Judd LM, Jenney A, Holt KE, Wyres KL, Hawkey J (2022) Epidemiology and genomic analysis of Klebsiella oxytoca from a single hospital network in Australia. BMC Infect Dis 22(1):704. https://doi.org/10.1186/s12879-022-07687-7
Fevre C, Jbel M, Passet V, Weill FX, Grimont PA, Brisse S (2005) Six groups of the OXY β-lactamase evolved over millions of years in Klebsiella oxytoca. Antimicrob Agents Chemother 49(8):3453–3462
Yang J, Long H, Hu Y, Feng Y, McNally A, Zong Z (2022) Klebsiella oxytoca complex: update on taxonomy, antimicrobial resistance, and virulence. Clin Microbiol Rev 35(1):e0000621
Scoulica EV, Neonakis IK, Gikas AI, Tselentis YJ (2004) Spread of blaVIM-1-producing E. coli in a university hospital in Greece. Genetic analysis of the integron carrying the blaVIM-1 metallo-β-lactamase gene. Diagn Microbiol Infect Dis 48(3):167–172
Patzer J, Toleman MA, Deshpande LM, Kaminska W, Dzierzanowska D, Bennett PM, Jones RN, Walsh TR (2004) Pseudomonas aeruginosa strains harbouring an unusual blaVIM-4 gene cassette isolated from hospitalized children in Poland (1998–2001). J Antimicrob Chemother 53(3):451–456
Biedrzycka M, Izdebski R, Urbanowicz P, Polanska M, Hryniewicz W, Gniadkowski M, Literacka E (2022) MDR carbapenemase-producing Klebsiella pneumoniae of the hypervirulence-associated ST23 clone in Poland, 2009–19. J Antimicrob Chemother 77(12):3367–3375
Arcari G, Di Lella FM, Bibbolino G, Mengoni F, Beccaccioli M, Antonelli G, Faino L, Carattoli A (2020) A multispecies cluster of VIM-1 carbapenemase-producing Enterobacterales linked by a novel, highly conjugative, and broad-host-range IncA plasmid forebodes the reemergence of VIM-1. Antimicrob Agents Chemother 64(4):e02435-e2519
Libisch B, Gacs M, Csiszar K, Muzslay M, Rokusz L, Fuzi M (2004) Isolation of an integron-borne blaVIM-4 type metallo-β-lactamase gene from a carbapenem-resistant Pseudomonas aeruginosa clinical isolate in Hungary. Antimicrob Agents Chemother 48(9):3576–3578
Urbanowicz P, Izdebski R, Baraniak A, Zabicka D, Hryniewicz W, Gniadkowski M (2021) Molecular and genomic epidemiology of VIM/IMP-like metallo-β-lactamase-producing Pseudomonas aeruginosa genotypes in Poland. J Antimicrob Chemother 76(9):2273–2284
Tsakris A, Poulou A, Markou F, Pitiriga V, Piperaki ET, Kristo I, Pournaras S (2011) Dissemination of clinical isolates of Klebsiella oxytoca harboring CMY-31, VIM-1, and a new OXY-2-type variant in the community. Antimicrob Agents Chemother 55(7):3164–3168
Arcari G, Raponi G, Sacco F, Bibbolino G, Di Lella FM, Alessandri F, Coletti M, Trancassini M, Deales A, Pugliese F, Antonelli G, Carattoli A (2021) Klebsiella pneumoniae infections in COVID-19 patients: a 2-month retrospective analysis in an Italian hospital. Int J Antimicrob Agents 57(1):106245
Emeraud C, Petit C, Gauthier L, Bonnin RA, Naas T, Dortet L (2022) Emergence of VIM-producing Enterobacter cloacae complex in France between 2015 and 2018. J Antimicrob Chemother 77(4):944–951
Papagiannitsis CC, Izdebski R, Baraniak A, Fiett J, Herda M, Hrabak J, Derde LP, Bonten MJ, Carmeli Y, Goossens H, Hryniewicz W, Brun-Buisson C, Gniadkowski M, Mosar Wp WP, groups WPs, Mosar Wp WP, groups WPs, (2015) Survey of metallo-β-lactamase-producing Enterobacteriaceae colonizing patients in European ICUs and rehabilitation units, 2008–11. J Antimicrob Chemother 70(7):1981–1988
Moradigaravand D, Martin V, Peacock SJ, Parkhill J (2017) Population structure of multidrug resistant Klebsiella oxytoca within hospitals across the UK and Ireland identifies sharing of virulence and resistance genes with K. pneumoniae. Genome Biol Evol 9(3):574–587
Long H, Hu Y, Feng Y, Zong Z (2022) Genome analysis of Klebsiella oxytoca complex for antimicrobial resistance and virulence genes. Antimicrob Agents Chemother 66(3):e0218321
Lam MMC, Wick RR, Wyres KL, Gorrie CL, Judd LM, Jenney AWJ, Brisse S, Holt KE (2018) Genetic diversity, mobilisation and spread of the yersiniabactin-encoding mobile element ICEKp in Klebsiella pneumoniae populations. Microb Genom 4(9):e000196
Tse H, Gu Q, Sze KH, Chu IK, Kao RY, Lee KC, Lam CW, Yang D, Tai SS, Ke Y, Chan E, Chan WM, Dai J, Leung SP, Leung SY, Yuen KY (2017) A tricyclic pyrrolobenzodiazepine produced by Klebsiella oxytoca is associated with cytotoxicity in antibiotic-associated hemorrhagic colitis. J Biol Chem 292(47):19503–19520
Dornisch E, Pletz J, Glabonjat RA, Martin F, Lembacher-Fadum C, Neger M, Hogenauer C, Francesconi K, Kroutil W, Zangger K, Breinbauer R, Zechner EL (2017) Biosynthesis of the enterotoxic pyrrolobenzodiazepine natural product tilivalline. Angew Chem 56(46):14753–14757
Hogenauer C, Langner C, Beubler E, Lippe IT, Schicho R, Gorkiewicz G, Krause R, Gerstgrasser N, Krejs GJ, Hinterleitner TA (2006) Klebsiella oxytoca as a causative organism of antibiotic-associated hemorrhagic colitis. N Engl J Med 355(23):2418–2426
Acknowledgements
We are very thankful to all colleagues of the National Reference Centre for Susceptibility Testing for their excellent work within the CPE surveillance programme. We would also like to cordially thank all microbiologists from clinical diagnostic laboratories who contributed to the study collection of bacterial isolates. A part of the data described in the paper were presented online as posters at the 30th European Congress of Clinical Microbiology and Infectious Diseases (30th ECCMID), 18–21 April 2020, P7454; online as posters at the 31st ECCMID, 9–12 July 2021, P4072 and as oral presentation at 32nd ECCMID, 23–26 April 2022, Lisbon, Portugal, O0230.
Funding
This work was supported by the Polish National Science Centre Grant 2019/33/B/NZ7/01461 and SPUB MIKROBANK from the Polish Ministry of Education and Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The isolates used in the current study were obtained during a routine national surveillance activity of the National Reference Centre for Susceptibility Testing, under the mandate of the Ministry of Health. The study was performed in a retrospective manner with an anonymisation of patients’ data; thus, ethical approval and informed consent were not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biedrzycka, M., Urbanowicz, P., Żabicka, D. et al. Country-wide expansion of a VIM-1 carbapenemase-producing Klebsiella oxytoca ST145 lineage in Poland, 2009–2019. Eur J Clin Microbiol Infect Dis 42, 1449–1457 (2023). https://doi.org/10.1007/s10096-023-04682-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04682-x