Abstract
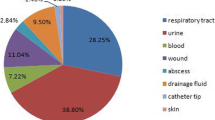
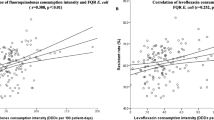
This study sought to discuss the correlation between the third-generation cephalosporins (3GC)-resistant Escherichia coli and Klebsiella pneumoniae and antibiotic consumption intensity from 143 Chinese tertiary hospitals in 2014. With a retrospective design, the correlation between antibiotic consumption and 3GC-resistant E. coli and K. pneumoniae were performed. 3GC-resistant E. coli was significantly correlated with the consumption of all antibiotics (r = 0.252, p < 0.01), β-Lactams antibiotics (r = 0.313, p < 0.01), β-Lactams excluding combinations with β-lactamase inhibitors (r = 0.365, p < 0.01), cephalosporin (r = 0.398, p < 0.01), cephalosporins excluding combinations with β-lactamase inhibitors (r = 0.374, p < 0.01), 3GC (r = 0.321, p < 0.01), and 3GC excluding combinations with β-lactamase inhibitors (r = 0.343, p < 0.01). 3GC-resistant K. pneumoniae was significantly correlated with the consumption of all antibiotics (r = 0.200, p < 0.05), β-Lactams antibiotics (r = 0.232, p < 0.01), cephalosporin (r = 0.215, p < 0.05), 3GC (r = 0.383, p < 0.01), 3GC excluding combinations with β-lactamase inhibitors (r = 0.245, p < 0.01), and β-lactam-β-lactamase inhibitor combinations (r = 0.218, p < 0.05). There was a significant relationship between the antibiotic consumption and the rates of 3GC-resistant E. coli and K. pneumoniae. Clinicians should grasp the indication of antibiotics use to reduce the production of drug-resistant bacteria.



Similar content being viewed by others
References
Temkin E, Fallach N, Almagor J et al (2018) Estimating the number of infections caused by antibiotic-resistant Escherichia coli and Klebsiella pneumoniae in 2014: a modelling study. Lancet Glob Health 6:e969–e979
Hwang AY, Gums JG (2016) The emergence and evolution of antimicrobial resistance: impact on a global scale. Bioorg Med Chem 24:6440–6445
Stewardson AJ, Allignol A, Beyersmann J et al (2016) The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: a multicentre retrospective cohort study. Euro Surveill 21:30319
Alvarez-Uria G, Gandra S, Mandal S et al (2018) Global forecast of antimicrobial resistance in invasive isolates of Escherichia coli and Klebsiella pneumoniae. Int J Infect Dis 68:50–53
Heng ST, Chen SL, Wong JGX et al (2018) No association between resistance mutations, empiric antibiotic, and mortality in ceftriaxone-resistant Escherichia coli and Klebsiella pneumoniae bacteremia. Sci Rep 8:12785
de Kraker ME, Wolkewitz M, Davey PG et al (2011) Burden of antimicrobial resistance in European hospitals: excess mortality and length of hospital stay associated with bloodstream infections due to Escherichia coli resistant to third-generation cephalosporins. J Antimicrob Chemother 66:398–407
Marchaim D, Gottesman T, Schwartz O et al (2010) National multicenter study of predictors and outcomes of bacteremia upon hospital admission caused by Enterobacteriaceae producing extended-spectrum beta-lactamases. Antimicrob Agents Chemother 54:5099–5104
de Kraker ME, Davey PG, Grundmann H et al (2011) Mortality and hospital stay associated with resistant Staphylococcus aureus and Escherichia coli bacteremia: estimating the burden of antibiotic resistance in Europe. PLoS Med 8:e1001104
Yang P, Chen Y, Jiang S et al (2018) Association between antibiotic consumption and the rate of carbapenem-resistant Gram-negative bacteria from China based on 153 tertiary hospitals data in 2014. Antimicrob Resist Infect Control 19:137
Rotty J, Hoy J (2008) New therapeutic agents in the management of HIV: an overview of darunavir for clinicians. Sex Health 5:235–241
Meyer E, Gastmeier P, Deja M et al (2013) Antibiotic consumption and resistance: data from Europe and Germany. Int J Med Microbiol 303:388–395
Gbaguidi-Haore H, Dumartin C, L'Hériteau F et al (2013) Antibiotics involved in the occurrence of antibiotic-resistant bacteria: a nationwide multilevel study suggests differences within antibiotic classes. J Antimicrob Chemother 68:461–470
Meyer E, Schwab F, Schroeren-Boersch B et al (2010) Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit Care 14:R113
Daoud Z, Salem-Sokhn E, Dahdouh E et al (2017) Resistance and clonality in Escherichia coli and Klebsiella spp. and relationship with antibiotic consumption in major Lebanese hospitals. J Glob Antimicrob Resist 11:45–51
Wushouer H, Zhang ZX, Wang JH et al (2018) Trends and relationship between antimicrobial resistance and antibiotic use in Xinjiang Uyghur Autonomous Region, China: based on a 3 year surveillance data, 2014-2016. J Infect Public Health 11:339–346
Hsueh PR, Chen WH, Luh KT (2005) Relationships between antimicrobial use and antimicrobial resistance in Gram-negative bacteria causing nosocomial infections from 1991-2003 at a university hospital in Taiwan. Int J Antimicrob Agents 26:463–472
Peirano G, Pitout JDD (2019) Extended-Spectrum β-lactamase-producing Enterobacteriaceae: update on molecular epidemiology and treatment options. Drugs 79:1529–1541
Padmini N, Ajilda AAK, Sivakumar N et al (2017) Extended spectrum β-lactamase producing Escherichia coli and Klebsiella pneumoniae: critical tools for antibiotic resistance pattern. J Basic Microbiol 57:460–470
Quan J, Zhao D, Liu L et al (2017) High prevalence of ESBL-producing Escherichia coli and Klebsiella pneumoniae in community-onset bloodstream infections in China. J Antimicrob Chemother 72:273–280
Nakai H, Hagihara M, Kato H et al (2016) Prevalence and risk factors of infections caused by extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae. J Infect Chemother 22:319–326
Chopra T, Marchaim D, Johnson PC et al (2015) Risk factors for bloodstream infection caused by extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae: a focus on antimicrobials including cefepime. Am J Infect Control 43:719–723
Funding
This study was sponsored by National Natural Science Foundation of China (81361138021, 81711530049), Key Research and Development Program of Zhejiang Province (2015C03032), and Zhejiang Province Medical Science and Technology Project (2017KY339).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Given that this study was performed without accessing patient information, approval of the ethics committee was not required.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Yang, P., Chen, Y., Jiang, S. et al. Association between the rate of third generation cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae and antibiotic consumption based on 143 Chinese tertiary hospitals data in 2014. Eur J Clin Microbiol Infect Dis 39, 1495–1502 (2020). https://doi.org/10.1007/s10096-020-03856-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03856-1