Abstract
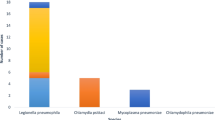
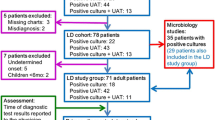
Currently, diagnosis of legionellosis relies mainly on urinary antigen testing (UAT) for Legionella pneumophila serogroup 1 (Lp1). However, this test has several limitations, particularly missing non-Lp1 infections. The purpose of this large multicenter study was to investigate the risk of missing legionellosis relying on UAT solely. Molecular results of Legionella detection as part of a first-line (syndromic) testing algorithm for severe respiratory tract infections were investigated retrospectively and compared with UAT results in 14 Belgian laboratories. Overall, 44.4% (20/45) UAT results appeared false negative and were reclassified as legionellosis based on PCR findings [Legionnaires’ disease, 37.5% (15/40); Pontiac fever, 100% (5/5)]. A total of 39.4% (26/66) diagnosis probably would have been missed or delayed without a syndromic approach, as UAT or specific molecular testing for Legionella was not requested by the clinician. Furthermore, we confirmed the higher sensitivity of molecular Legionella detection in lower respiratory tract compared with upper respiratory tract specimens (p = 0.010).
Similar content being viewed by others
References
Cunha BA, Burillo A, Bouza E (2016) Legionnaires’ disease. Lancet 387(10016):376–385
Chen DJ, Procop GW, Vogel S, Yen-Lieberman B, Richter SS (2015) Utility of PCR, culture, and antigen detection methods for diagnosis of Legionellosis. J Clin Microbiol 53(11):3474–3477
Gadsby NJ, Helgason KO, Dickson EM, Mills JM, Lindsay DS, Edwards GF et al (2016) Molecular diagnosis of Legionella infections—clinical utility of front-line screening as part of a pneumonia diagnostic algorithm. J Inf Secur 72(2):161–170
Mercante JW, Winchell JM (2015) Current and emerging Legionella diagnostics for laboratory and outbreak investigations. Clin Microbiol Rev 28(1):95–133
World Health Organization. Facts on gender and tobacco [Internet]. 2010 [cited 1 November 2019]. Available from: https://www.who.int/gender/documents/10facts_gender_tobacco_en.pdf
Dirven K, Ieven M, Peeters MF, van der Zee A, De Schrijver K, Goossens H (2005) Comparison of three Legionella urinary antigen assays during an outbreak of legionellosis in Belgium. J Med Microbiol 54(Pt 12):1213–1216
Miyata J, Huh JY, Ito Y, Kobuchi T, Kusukawa K, Hayashi H (2017) Can we truly rely on the urinary antigen test for the diagnosis? Legionella case report. J Gen Fam Med 18(3):139–143
Peci A, Winter AL, Gubbay JB (2016) Evaluation and comparison of multiple test methods, including real-time PCR, for Legionella detection in clinical specimens. Front Public Health 4:175
Pierre DM, Baron J, Yu VL, Stout JE (2017) Diagnostic testing for Legionnaires’ disease. Ann Clin Microbiol Antimicrob 16(1):59
European Centre for Disease Prevention and Control (2019) Legionnaires’ disease. In: ECDC. Annual epidemiological report for 2017. ECDC, Stockholm
European Centre for Disease Prevention and Control (2017) European Legionnaires’ Disease Surveillance Network (ELDSNet) – Operating procedures for the surveillance of travel-associated Legionnaires’ disease in the EU/EEA. ECDC, Stockholm
Diederen BM, Peeters MF (2007) Are oropharyngeal swabs suitable as samples for Legionella-specific PCR testing? J Clin Microbiol 45(10):3482–3483
R Core Team (2016) R: A Language and Environment for Statistical Computing. Vienna, Austria. Available from: https://www.R-project.org
World Health Organization. Legionellosis [Internet]. February 2018 [cited 8 July 2019]. Available from: https://www.who.int/news-room/fact-sheets/detail/legionellosis
Avni T, Bieber A, Green H, Steinmetz T, Leibovici L, Paul M (2016) Diagnostic accuracy of PCR alone and compared to urinary antigen testing for detection of Legionella spp.: a systematic review. J Clin Microbiol 54(2):401–411
Steensels D, Reynders M, Descheemaeker P, Curran MD, Jacobs F, Denis O et al (2015) Clinical evaluation of a multi-parameter customized respiratory TaqMan(®) array card compared to conventional methods in immunocompromised patients. J Clin Virol 72:36–41
Belgische Vereniging voor Infectiologie en Klinische Microbiologie. IGGI Infectiologiegids - Guide d'Infectiologie [Internet]. October 2018 [cited 8 November 2019]. Available from: https://www.bvikm.org
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC et al (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44:S27–S72
Agentschap Zorg & Gezondheid. Legionellose [Internet]. April 2018 [cited 9 July 2019]. Available from: https://www.zorg-en-gezondheid.be/legionellose
European Centre for Disease Prevention and Control. EU case definitions [Internet]. July 2018 [cited 9 July 2019]. Available from: https://ecdc.europa.eu/en/surveillance-and-disease-data/eu-case-definitions
Centers for Disease Control and Prevention. Legionnaires Disease Case Definitions [Internet]. June 2010 [cited 9 July 2019]. Available from: https://www.cdc.gov/legionella/health-depts/surv-reporting/case-definitions.html
Acknowledgments
We would like to thank the participating laboratories for kindly providing the lab-technical and clinical data concerning their patients.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muyldermans, A., Descheemaeker, P., Boel, A. et al. What is the risk of missing legionellosis relying on urinary antigen testing solely? A retrospective Belgian multicenter study. Eur J Clin Microbiol Infect Dis 39, 729–734 (2020). https://doi.org/10.1007/s10096-019-03785-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03785-8