Abstract
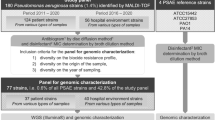
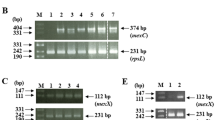
Our study aims to define the epidemiology of carbapenem resistance mechanisms in clinical isolates of Pseudomonas aeruginosa (PA). We evaluated 11,457 clinical PA strains isolated between 2009 and 2015 at the tertiary care University Hospital in Heidelberg, Germany. Thirty-four percent of the isolates (3867/11,457) were MDR (multidrug-resistant), 16% (1816/11,457) were XDR (extensively drug resistant), and less than 1% (82/11,457) had a PDR (pandrug-resistant) profile. Of those, 23% carried a carbapenemase gene (CPM positive) with 12% VIM-2, 10% VIM-1, and less than 1% IMP-1. Comparing MIC (minimal inhibitory concentration) distributions, the mean rank for meropenem, imipenem, gentamicin, and fosfomycin was significantly higher in the CPM-positive group than in the CPM-negative XDR group (p ≤ 0.004). oprD (outer membrane protein) mutations were found in 19/19 tested strains; 12/19 carried a CPM and had a higher mutation rate. Meropenem resistance was mostly associated with the presence of CPM. Only 1/19 strains was meropenem resistant in the absence of CPM genes; nevertheless, it carried an oprD mutation in a strategic site (loop 2). Of 19 CPM-negative strains tested, 7 (36%) showed EP (efflux pumps) hyperexpression versus 12 in the CPM-positive strains. In our study, nearly 50% of the PA isolates exhibited resistance to the tested first-line antibiotics. Our study also demonstrates that carbapenemase genes can be isolated in approximately 23% of XDR PA strains in our population. This finding supports the clinical relevance of PA driven by the possible presence of multiple resistance mechanisms acquired under exposure to antibiotics or by horizontal transfer of resistance genes.
Similar content being viewed by others
Abbreviations
- PA:
-
Pseudomonas aeruginosa
- MDR:
-
Multidrug-resistant
- XDR:
-
Extensively drug-resistant
- PDR:
-
Pandrug-resistant
- PTZ:
-
Piperacillin tazobactam
- CAZ:
-
Ceftazidime
- GEN:
-
Gentamicin
- IMP:
-
Imipenem
- MEM:
-
Meropenem
- FOS:
-
Fosfomycin
- ICU:
-
Intensive care unit
- ESBL:
-
Extended spectrum beta-lactamase
- CPM:
-
Carbapenemases
- oprD:
-
Outer membrane protein gene
- OprD:
-
Outer membrane protein amino acid sequence
- EP:
-
Efflux pumps
- PaβN:
-
Phe-Arg-β-naphthylamide
- MBL:
-
Metallo-beta-lactamases
- MIC:
-
Minimal inhibitory concentration
References
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL et al (2018) Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 18(3):318–327
Webber MA, Piddock LJ (2003) The importance of efflux pumps in bacterial antibiotic resistance. J Antimicrob Chemother 51(1):9–11
Choudhury D, Das Talukdar A, Dutta Choudhury M, Maurya AP, Paul D, Dhar Chanda D et al (2015) Transcriptional analysis of MexAB-OprM efflux pumps system of Pseudomonas aeruginosa and its role in carbapenem resistance in a tertiary referral hospital in India. PLoS One 10(7):e0133842
Mesaros N, Glupczynski Y, Avrain L, Caceres NE, Tulkens PM, Van Bambeke F (2007) A combined phenotypic and genotypic method for the detection of Mex efflux pumps in Pseudomonas aeruginosa. J Antimicrob Chemother 59(3):378–386
Lomovskaya O, Warren MS, Lee A, Galazzo J, Fronko R, Lee M et al (2001) Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob Agents Chemother 45(1):105–116
Epp SF, Kohler T, Plesiat P, Michea-Hamzehpour M, Frey J, Pechere JC (2001) C-terminal region of Pseudomonas aeruginosa outer membrane porin OprD modulates susceptibility to meropenem. Antimicrob Agents Chemother 45(6):1780–1787
Ochs MM, Bains M, Hancock RE (2000) Role of putative loops 2 and 3 in imipenem passage through the specific porin OprD of Pseudomonas aeruginosa. Antimicrob Agents Chemother 44(7):1983–1985
Ochs MM, McCusker MP, Bains M, Hancock RE (1999) Negative regulation of the Pseudomonas aeruginosa outer membrane porin OprD selective for imipenem and basic amino acids. Antimicrob Agents Chemother 43(5):1085–1090
Poirel L, Naas T, Nordmann P (2010) Diversity, epidemiology, and genetics of class D beta-lactamases. Antimicrob Agents Chemother 54(1):24–38
Potron A, Poirel L, Nordmann P (2015) Emerging broad-spectrum resistance in Pseudomonas aeruginosa and Acinetobacter baumannii: mechanisms and epidemiology. Int J Antimicrob Agents 45(6):568–585
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 6.0, 2016. http://www.eucast.org
Standardization IO for. ISO 20776-1.2006 Clinical laboratory testing and in vitro diagnostic test systems — susceptibility testing of infectious agents and evaluation of performance of antimicrobial susceptibility test devices — Part 1: reference method for testing the in vitro activity of antimicrobial agents against rapidly growing aerobic bacteria involved in infectious diseases [Internet]. 2006. Report No.: 20776–1.2006. Available from: https://www.iso.org/obp/ui/#iso:std:iso:20776:-1:ed-1:v1:en
Kaiser SJ, Mutters NT, DeRosa A, Ewers C, Frank U, Günther F (2017) Determinants for persistence of Pseudomonas aeruginosa in hospitals: interplay between resistance, virulence and biofilm formation. Eur J Clin Microbiol Infect Dis 36(2):243–253
Winsor GL, Griffiths EJ, Lo R, Dhillon BK, Shay JA, Brinkman FSL (2016) Enhanced annotations and features for comparing thousands of Pseudomonas genomes in the Pseudomonas genome database. Nucleic Acids Res 44(Database issue):D646–D653
Gutierrez O, Juan C, Cercenado E, Navarro F, Bouza E, Coll P et al (2007) Molecular epidemiology and mechanisms of carbapenem resistance in Pseudomonas aeruginosa isolates from Spanish hospitals. Antimicrob Agents Chemother 51(12):4329–4335
El Amin N, Giske CG, Jalal S, Keijser B, Kronvall G, Wretlind B (2005) Carbapenem resistance mechanisms in Pseudomonas aeruginosa: alterations of porin OprD and efflux proteins do not fully explain resistance patterns observed in clinical isolates. APMIS. 113(3):187–196
Ocampo-Sosa AA, Cabot G, Rodriguez C, Roman E, Tubau F, Macia MD et al (2012) Alterations of OprD in carbapenem-intermediate and -susceptible strains of Pseudomonas aeruginosa isolated from patients with bacteremia in a Spanish multicenter study. Antimicrob Agents Chemother 56(4):1703–1713
Pragasam AK, Raghanivedha M, Anandan S, Veeraraghavan B (2016) Characterization of Pseudomonas aeruginosa with discrepant carbapenem susceptibility profile. Ann Clin Microbiol Antimicrob 15:12
KRINKO. Zur aktuellen Situation bei Carbapenemase-bildenden gramnegativen Bakterien Ein Bericht des NRZ für gramnegative Krankenhauserreger. RKI Robert Koch Institut
Wendel AF, Brodner AH, Wydra S, Ressina S, Henrich B, Pfeffer K et al (2013) Genetic characterization and emergence of the metallo-beta-lactamase GIM-1 in Pseudomonas spp. and Enterobacteriaceae during a long-term outbreak. Antimicrob Agents Chemother 57(10):5162–5165
Rieber H, Frontzek A, Pfeifer Y (2012) Emergence of metallo-beta-lactamase GIM-1 in a clinical isolate of Serratia marcescens. Antimicrob Agents Chemother 56(9):4945–4947
Kaase M, Szabados F, Pfennigwerth N, Anders A, Geis G, Pranada AB et al (2014) Description of the metallo-beta-lactamase GIM-1 in Acinetobacter pittii. J Antimicrob Chemother 69(1):81–84
Wendel AF, Kolbe-Busch S, Ressina S, Schulze-Robbecke R, Kindgen-Milles D, Lorenz C et al (2015) Detection and termination of an extended low-frequency hospital outbreak of GIM-1-producing Pseudomonas aeruginosa ST111 in Germany. Am J Infect Control 43(6):635–639
Jovcic B, Lepsanovic Z, Suljagic V, Rackov G, Begovic J, Topisirovic L et al (2011) Emergence of NDM-1 metallo-beta-lactamase in Pseudomonas aeruginosa clinical isolates from Serbia. Antimicrob Agents Chemother 55(8):3929–3931
Janvier F, Jeannot K, Tessé S, Robert-Nicoud M, Delacour H, Rapp C et al (2013) Molecular characterization of blaNDM-1 in a sequence type 235 Pseudomonas aeruginosa isolate from France. Antimicrob Agents Chemother 57(7):3408–3411
Rahman M, Shukla SK, Prasad KN, Ovejero CM, Pati BK, Tripathi A et al (2014) Prevalence and molecular characterisation of New Delhi metallo-β-lactamases NDM-1, NDM-5, NDM-6 and NDM-7 in multidrug-resistant Enterobacteriaceae from India. Int J Antimicrob Agents 44(1):30–37
team EC for DP and C (ECDC)-HCU-E editorial (2013) Isolation of NDM-1-producing Pseudomonas aeruginosa sequence type ST235 from a stem cell transplant patient in Italy, May 2013 [internet]. [cited 2017 Sep 20]. Available from: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20633
Yokoyama K, Arakawa Y (2003) Acquisition of 16S rRNA methylase gene in Pseudomonas aeruginosa. Lancet 362(9399):1888–1893
Fontes LC, Neves PR, Oliveira S, Silva KC, Hachich EM, Sato MIZ et al (2011) Isolation of Pseudomonas aeruginosa coproducing metallo-β-lactamase SPM-1 and 16S rRNA methylase RmtD1 in an Urban River▿. Antimicrob Agents Chemother 55(6):3063–3064
Gurung M, Moon DC, Tamang MD, Kim J, Lee YC, Seol SY et al (2010) Emergence of 16S rRNA methylase gene armA and cocarriage of blaIMP-1 in Pseudomonas aeruginosa isolates from South Korea. Diagn Microbiol Infect Dis 68(4):468–470
Edalucci E, Spinelli R, Dolzani L, Riccio ML, Dubois V, Tonin EA et al (2008) Acquisition of different carbapenem resistance mechanisms by an epidemic clonal lineage of Pseudomonas aeruginosa. Clin Microbiol Infect 14(1):88–90
Funding
The study was supported by a grant from the Ministry of Science, Research and the Arts of Baden-Württemberg (MWK) within the project “Surveillance von Mehrfach-Antibiotika-Resistenzen“; grant recipient NTM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
All used isolates were routinely collected in the microbiology laboratory of the Heidelberg University Hospital and stored at − 70 °C. The current study thus is descriptive of those isolates. Data collected from patients was anonymized and restricted to possible clinical symptoms of infection. Ethical approval and informed consent statements were therefore not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Rosa, A., Mutters, N.T., Mastroianni, C.M. et al. Distribution of carbapenem resistance mechanisms in clinical isolates of XDR Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis 38, 1547–1552 (2019). https://doi.org/10.1007/s10096-019-03585-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03585-0